
1
Pediatric surgery
Lec.2
د
.ا
ﯾ
ﺴ
ﺮ
ﺣ
ﻤ
ﯿ
ﺪ
ا
ﺘﻟ
ﻤ
ﯿ
ﻤ
ﻲ
Intestinal atresia and stenosis
Congenital defects in continuity of the intestine are
morphologically divided into either stenosis or atresia and
constitute one of the most common causes of neonatal intestinal
obstruction.
Pyloric atresia
Pyloric atresia is a rare autosomal genetic defect and has a well
documted association with epidermolysis bullosa , in which the
pyloric lumen is completely obliterated by either a diaphragm or a
solid core of tissue, or a complete absence of the pylorus with loss
of bowel continuity is noted. Nonbilious vomiting and upper
abdominal distention result. Abdominal radiograph shows a single
gas bubble or air/fluid level and no distal air in the gastrointestinal
(GI) tract . The differential diagnosis includes high duodenal
atresia and malrotation with volvulus of the midgut. Gastric
perforation may lead to peritonitis and toxemia.
Surgical excision for membranous atresia or a side-to-side
gastroduodenostomy successfully restores continuity. Long- term
outcome is excellent except for those with epidermolysis bullosa.

2
DUODENAL ATRESIA AND STENOSIS
Etiology
Duodenal atresia and stenosis are most commonly believed to be
caused by a failure of recanalization ,it can be divided into either:
A: incomplete obstruction, may be due to a diaphragm or web
with a small opening.
B:Atresia or complete obstruction, may be seen with duodenal
muscular continuity or with a gap that is usually filled with
pancreatic tissue. prematurity. growth retardation, and coexistent
malformations are common. Almost 50% of duodenal atresia are
associated with some other anomaly (e.g., cardiac,genitourinarv,
anorectal, or, occasionally, esophageal atresia)and up to 40% have
trisomy 2l.
pathology
the site of obstruction is usually classified as either
preampullary(one third), or postampullary(two third) and
Depending on the degree of obstruction, the proximal duodenum
and stomach dilate to several times their normal size. The bowel
distal to the obstruction is collapsed,and in the cases of complete
atresia, thin walled. Because the obstruction is high, it is
decompressed proximally in and perforation is rare. Associated
polyhydramnois is recorded in up to one half of cases, with
premature delivery in one third. Growth retardation also is
common, which may imply that the fetus has been deprived of the
nutritional contribution of swallowed amniotic fluid.
Diagnosis
Prenatal diagnosis
Polyhydramnios results from high intestinal obstruction because
the reabsorption of amniotic fluid is disturbed. The dilated stomach
and proximal duodenum may be seen on antenatal ultrasonography
(us), as may associated cardiac abnormalities. Most cases of
duodenal atresia are detected between months 7 and 8 of

3
intrauterine life, but a normal US of the fetus with polyhydramnios
at that time does not absolutely exclude duodenal obstruction.
Postnatal diagnosis
The vomiting of clear or bile-stalned fluid usually starts within
hours of birth. Distention or abnormal stooling may or may not be
present. Aspiration via a nasogastric tube of more than 20 mL of
gastric contents in a newborn suggests intestinal obstruction; the
normal aspirate is less than 5 mL.M The diagnosis of an
incomplete obstruction (stenosis or web) may be delayed until well
beyond the neonatal period. Because most duodenal obstructions
occur distal to the ampulla, the vomitus is bile stained in more than
two thirds. Occasionally, blood-stained vomitus results from
gastritis. Abdominal distention may not be evident (high level
obstruction) , owing to vomiting. Delayed diagnosis may result in
dehydration, hyponatremia, and hypochloremia. Jaundice, if
present, is rarely obstructive and is more likely due to prematurity
and dehydration.
An upright abdominal radiograph using instilled air, if necessary,
as contrast, is sufficient to confirm the diagnosis by demonstrating
double bubble appearance. Intestinal gas beyond the duodenum
indicates incomplete obstruction(stenosis)
Management
Once the diagnosis has been established, gastric decompression
and correction of fluid and electrolyte disturbances are begun.
Other associated anomalies should be excluded by appropriate
investigation with radiography, US, and echocardiography. Only
after the baby has been resuscitated is operative correction
performed The operation preferred by most is a diamond-shaped
or side-to-side duodeuoduodenostomy.
JEJUNOILEAL ATRESIA AND STENOSIS
Etiology
Although several mechanisms have been postulated to explain the
intestinal atresia malformations the most favored theory is that of a

4
localized intrauterine vascular accident with ischemic necrosis of
the sterile bowel and subsequent resorption of the affected segment
or segments
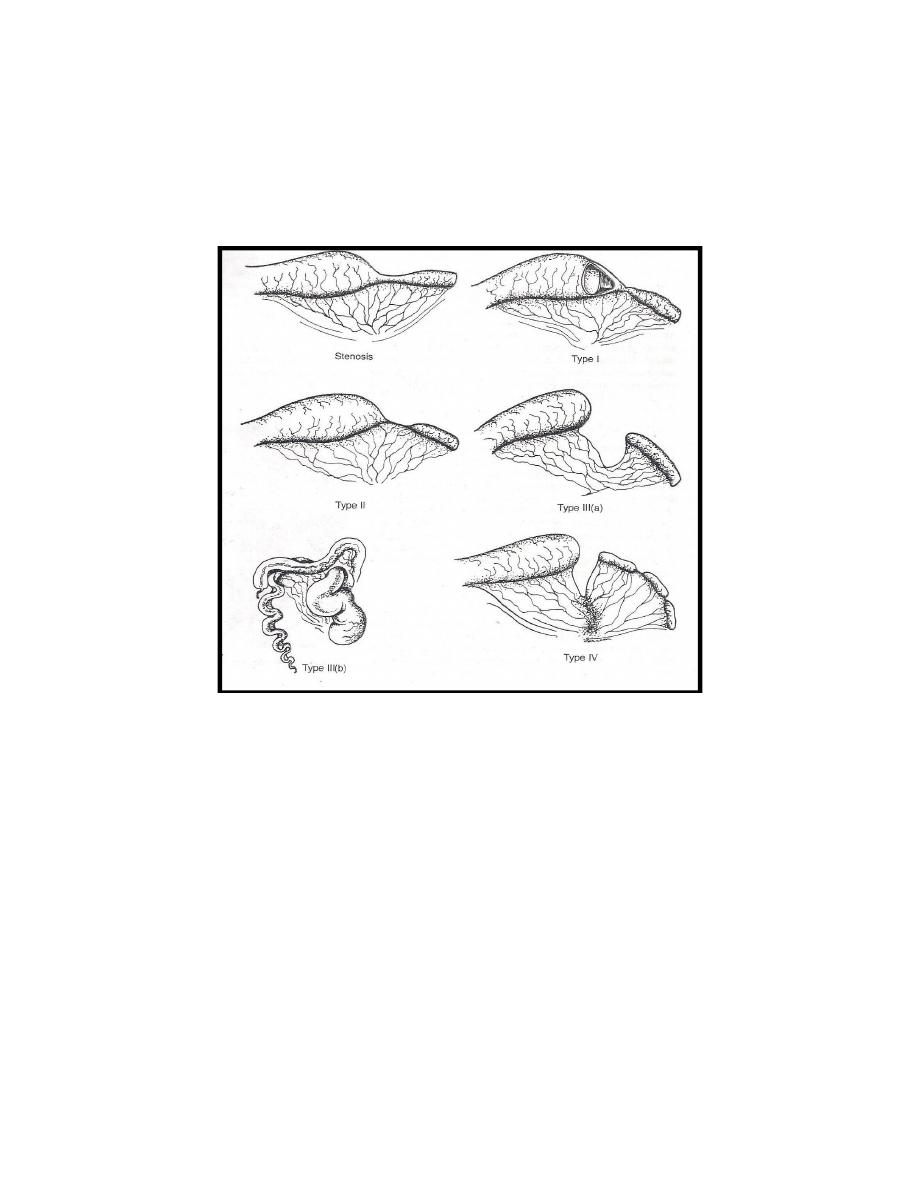
classification
jejunoileal obstruction can be classified as either Atresia or
Stenosis
1_Stenosis is defined as a localized narrowing of the intestinal
lumen without disruption of continuity or defect in the mesentery.
The small intestine is of normal length.
2_Atresia that can be classified into four types according to their
mophological and prognostic value
Atresia Type I
In atresia type I the obstruction is caused by a membrane or web
formed by mucosa and submucosa. The proximal dilated bowel
and distal collapsed bowel are in continuity without a mesenteric
defect. The bowel length is of normal length.
Atresia Type II
In atresia type II (blind ends joined by a fibrous cord), the
proximal bowel terminates in a bulbous blind end, which is
connected to the collapsed distal bowel by a short fibrous cord
along the edge of an intact mesentery. The total small bowel length
is usually normal.
Atresia Type 111(a)
in atresia type 111(a) (disconnected blind ends), the atresia ends
blindly both proximally and distally, as in type II, but the fibrous
connecting cord is absent, and a V-shaped rnesenteric defect of
varying size is seen The total length of the bowel is subnormal and
variable,
Atresia Type 111(b)
aItresia type 111(b) ( Christmas tree) consists of a proximal jejunal
atresia near the ligament of Treitz
The distal small bowel lies free in the abdomen and assumes a
helix configuration around a single perfusing artery.
5
Atresia Type IV
in atresia type IV, multiple-segment atresias of a combination of
types I to III are present and bowel length is foreshortened.
Figure (1) classification of ileojejunal atresia
Diagnosis:
In babies with atresia or stenosis ,bilious vomiting usually
developing the first day of life but in 20% of children it may be
delayed for 2 to 3 days.the higher the obstruction, the earlier and
more
forcefull
the
vomiting.dehydration,uncongucated
hyperbilirubinemia,and aspiration pneumonia occur with delay
diagnosis abdominal distention is more pronounced with distal
small bowel obstruction .
Plain x ray abdomen using the air as a contrast shows multiple
fluid levels .

6
Management
Delay in diagnosis may lead to impairment of viability (50%),
frank necrosis and perforation (10% to 20%) of the bulbous
proximal end, fluid and electrolyte abnormalities, and increased
incidence of sepsis.Electrolyte and volume resuscitation is started.
Nasogastric or orogastric tube decompression may improve
diaphragmatic excursion and prevent vomiting and aspiration.
Surgical Considerations
The operative procedure depends on the pathologic findings.
Resection of the proximal dilated and hypertrophied bowel with
primary end-to-end anastomosis between the proximal and distal
bowel.
Colonic atresia
.Atresia of the colon is a rare form of intestinal atresia and
composes from 1.8% to 15 % of all intestinal atresias and
stenoses). Atresias can occur at any level along the colon
Concomitant small bowel atresia, Hirschsprung’s disease, and
gastroschisis are not infrequently associated with colonic atresia.
The atresia is most likely due to mesenteric vascular impairment or
intrauterine volvulus.
Prenatal diagnosis:
can be suspected on US in the presence of bowel obstruction and
if the diameter of the colon is larger than expected for gestational
age.
Postnatal diagnosis:
These infants are usually term and have rapidly progressing
findings of distal intestinal obstruction. Delay in diagnosis can lead
to ischemia and proximal bowel perforation.
Abdominal radiographs confirm distal bowel obstruction, often
with a disproportionately large loop related to the dilated proximal
colonic segment. A contrast enema confirms colonic atresia,

7
showing a small-diameter colon that terminates adjacent to the
obstructed colonic segment.
The surgical approach depends on the clinical status o the patient,
the level of atresia. the status of the bowel proximal to the atresia,
any associated small intestinal
It is important to ensure patency of the entire colon, because
multiple atresias and stenosis
can occur, and the final procedure is end to end anastomosis.
Prognosis
is usually excellent but depends on residual small bowel length,
concomitant small bowel pathology, and associated anomalies.
