
36
College of Medicine/Babylon University
Medical Physics Module
Lecture 6:
Physics of the lung and Breathing
Objectives: after the end of this lecture, the student must know:
1- How blood and lungs interact
2- Role of surfactant in preventing lung collapse
3- Physics of certain lung diseases.
We breath 6 liters of air per minute (this is also about the volume of blood the
heart pumps each minute). Men breath 12 times per minute at rest while women
and infants breath 20 times, 60 times per second respectively.
The air we inspire about (80 % N2 + 20 % O2), the air we expire (80% N2+16 %
O2 + 4%CO2)
The lungs have large convoluted shape with surface area about 80m². It is
surprising that we do not have more disease of lung.
The Air Ways
The air passes through windpipe (trachea), each bronchus divide multiple
times (about 15 times) until it reach to a sac like structure called alveoli of
0.2mm diameter and 0.4 μm wall thickness, each alveolus surrounded by blood
capillary. So O2 can diffuse from alveolus into RBC and CO2 diffuse from blood
into air in the alveolus.
1- Large chunks removed by cough
2- Small particles carried upward to the mouth by millions of small hairs or cilia
of 0.1mm long that have wave like motion.
Each cilia vibrates about 1000 times a minute. The mucus moves 1-2
cm/min (1 mile/week). Cilia as escalator system of trachea. It takes 30 min for

37
College of Medicine/Babylon University
Medical Physics Module
particle of dust to be cleared out of the bronchi and trachea into throat where
it is expelled or swallowed.
How Blood And Lungs Interact
About (1 Liter) of blood supply the lungs, but only 70 ml is in the capillaries
of the lungs getting O2.
The transfer of O2 and CO2 into and out of blood is controlled by law of
diffusion. Molecules diffuse from region of higher concentration to lower
concentration until concentration uniform.
A molecule of O2 diffuse faster than CO2 because of its smaller mass. The
lungs are not emptied during expiration, during normal breath the lungs retains
about 30% of their volume at the end of each expiration.
Measurement Of Lungs Volumes
During normal breathing we inhale 500 cm³ of air with each breath. If a
person cough or sneeze hard the velocity of air in the trachea can reach the
velocity of sound in air.
This high velocity can cause partial collapse of air ways because of Bernoulli
effect.
In coughing to dislodge foreign object, this partial collapse increases air
velocity and increase the force on foreign object.
Not all air we inspire adds O2, the volume of trachea and bronchi called
anatomic dead space, since air in space is not exposed to blood in pulmonary
capillaries the space about 150 cm
3.
College of Medicine/Babylon University
Medical Physics Module
Physics Of The Alveoli
The alveoli like millions of small interconnected bubbles, have tendency to
get smaller due to surface tension of unique fluid lining. This lining called
surfactant
. The absence of surfactant in the lungs of some new born infant is
the cause of respiratory distress syndromes (RDS) called hyaline membrane
disease which causes death.
To understand the physics of alveoli we have to understand physics of bubble.
The pressure inside bubble is inversely proportional to the radius and directly to
the surface tension.
P = 4 γ / R
Where R radius, γ surface tension
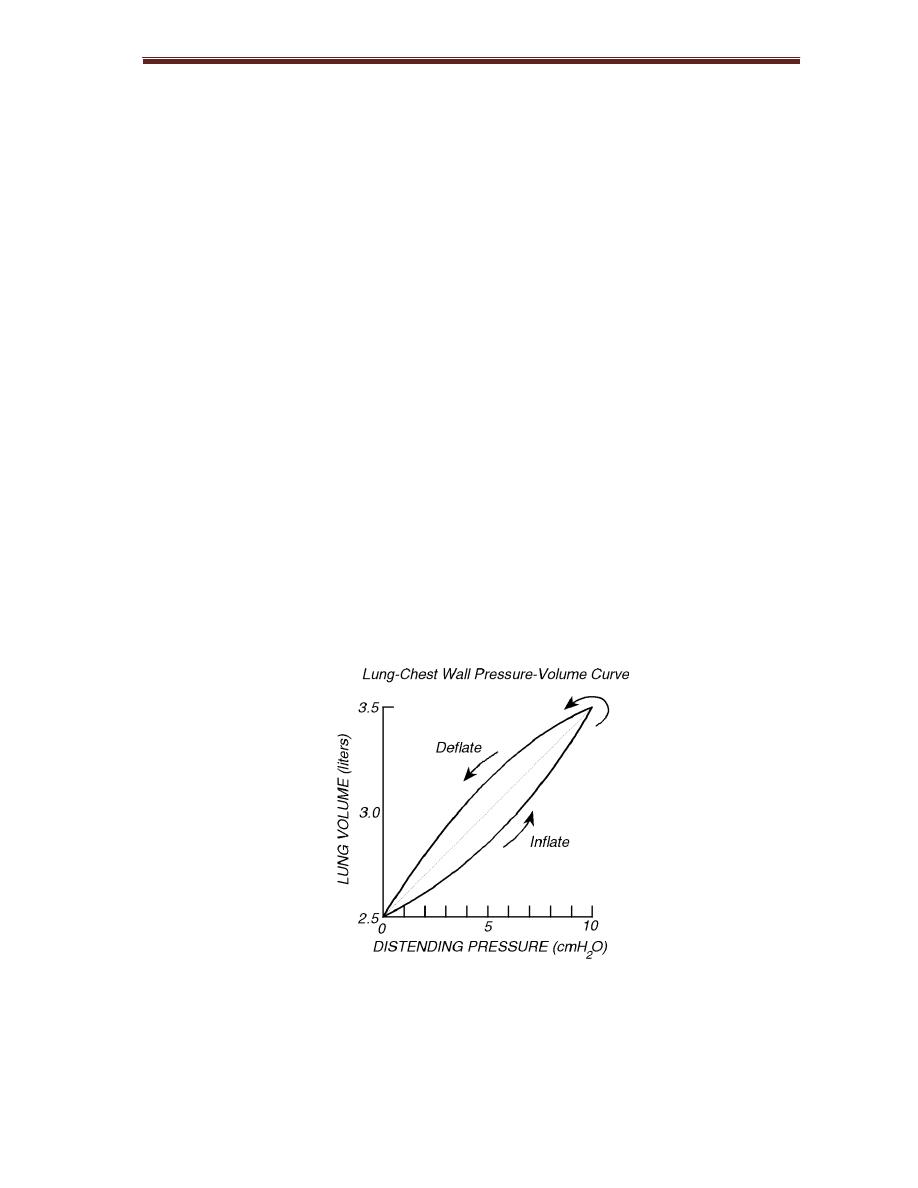
Figure 6-1 shows P-V curves for human lungs when p needed to then reinflate
the lungs
Figure 6-1:
P-V curve
Two Forces Keep Lungs From Collapsing
1- surface tension between lungs and chest
wall

39
College of Medicine/Babylon University
Medical Physics Module
2- 2- Air pressure inside the lungs
College of Medicine/Babylon University
Medical Physics Module
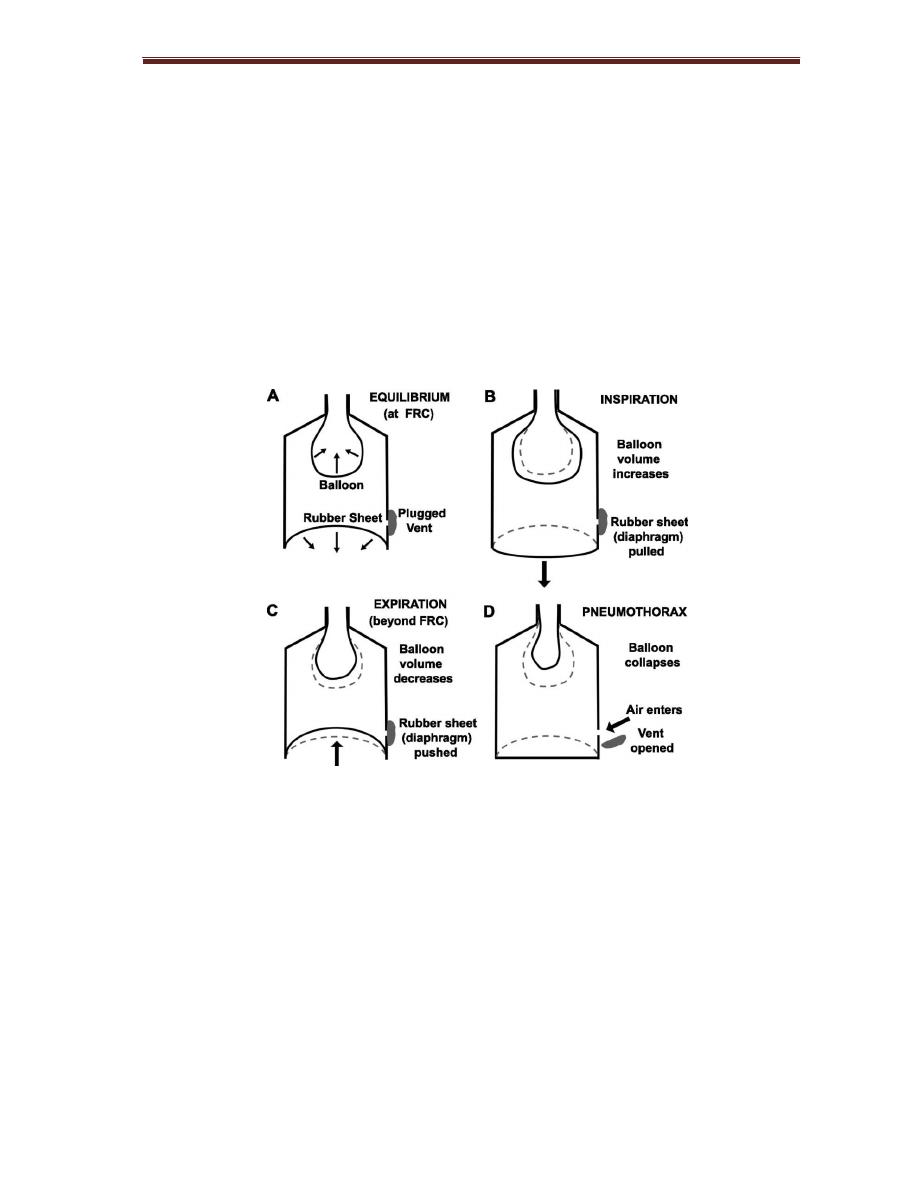
Since each lung is its own sealed compartment, it is possible to collapse one
lung only. This is done by inserting a hollow needle between ribs and allowing
air to flow into intrathoracic space, the air trapped in the space is gradually
absorbed by tissue and lung expand to normal over few weeks, sometimes
lung collapses spontaneously with no known cause.
The lungs returns to normal as the air is absorbed into surrounding tissues.
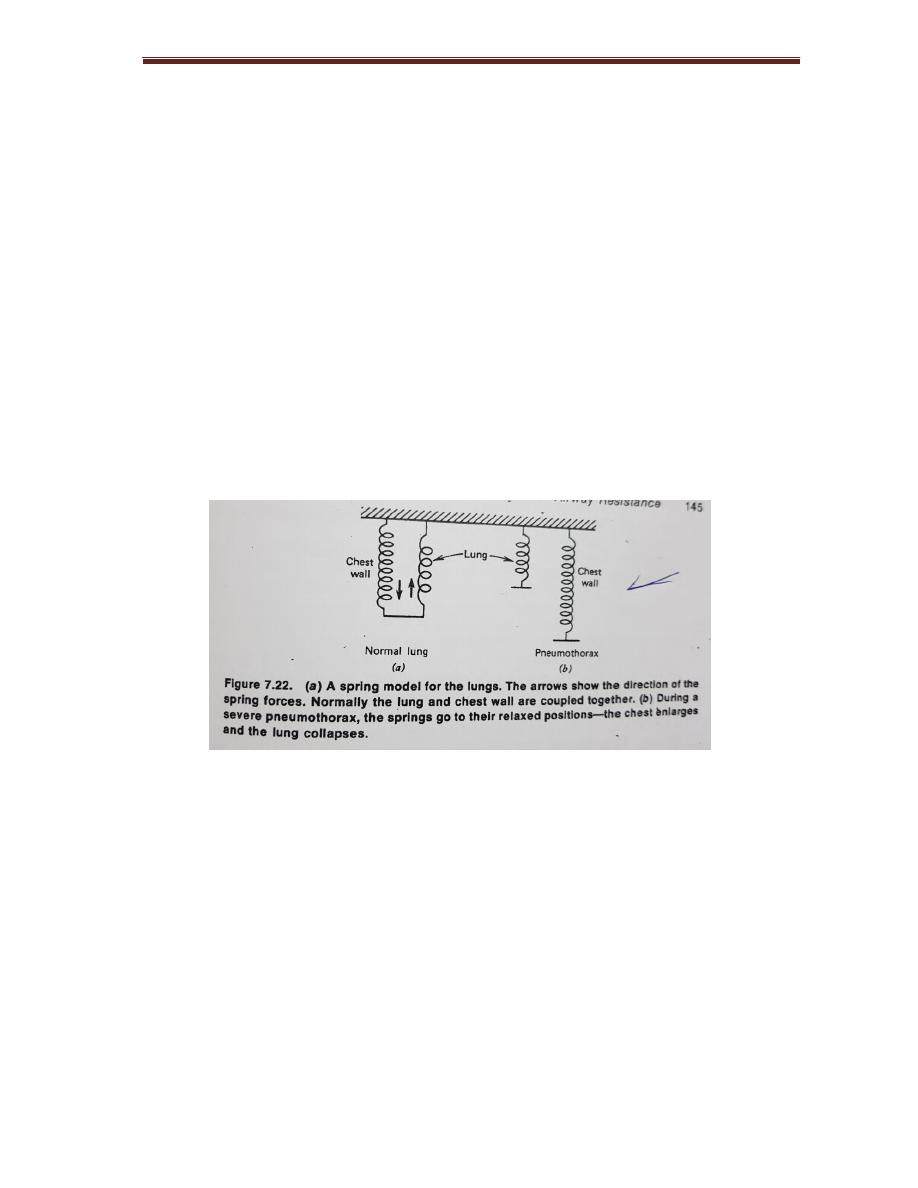
Since both lung and chest are elastic we can represent them with springs.
Figure 6-3: simple model for mechanism of breathing during (A) normal
conditions, B inspiration, C expiration and D pneumothorax.
Air Way Resistance
During
inspiration the forces on airways tend to open them further, during
expiration the forces tend to close the airways and restrict flow.
Voltage replaced by pressure difference ∆P
Current replaced by rate of air flow or V
College of Medicine/Babylon University
Medical Physics Module
Air way resistance
Rg = ∆ P / V
Most of resistance in the upper airway passages.
10% of Rg is in the terminal airways (bronchioles and alveoli) do not affect air
way resistance until they are far advanced.
Physics Of Common Lung Diseases
Emphysema
the division between alveoli break down produces large lung
spaces, this destruction of lung tissue reduces the springiness of lungs. The
lungs become more complaint, small change in pressure produces larger than
normal change in volume.
Emphysema
Produces two changes:
1- The lungs become flabby and expands
2- The tissues do not pull very hard on the airways permitting the narrowed
airways to collapse easily during expiration
In asthma due to increasing airway resistance, some of resistance is due to
swelling (edema) and mucus in the smaller airways but much of it is due to
contraction of smooth muscles round the large air ways.
Fibrosis of lungs
, the membranes between alveoli thicken.
This has two effects
1- the compliance of the lungs decreases
2- The diffusion of O2 into capillary decreases
Fibrosis can occur if the lungs have been irradiated e.g. in treatment of

42
College of Medicine/Babylon University
Medical Physics Module
Small group discussion:
Qx/ Can you test the pulmonary function and how?
Qx/ What are the suspected abnormalities that can be seen on a Spirogram of
asthmatic patient?
Qx/ In a patient with sever emphysema, which of the following are above the
normal:
i. Airway resistance.
ii. Inspiratory reverse volume.
iii. Functional residual capacity.
iv. Vital capacity.
v. Compliance.
