Antepartum hemorrhage
Gynecology
1
Antepartum hemorrhage
Assisted prof. dr. Alaa AL-Naser
Objectives
1.Be familiar with RCOG guide lines: APH
2.Causes(P.P, A.P, Vasaprevia, Accreta)
3.Understand the mechanism of DIC
4.Safe use of blood products
5.Be competent in Mx of APH & major obstetric Hg.
6.Have attended skills drills on obstetric collapse.
7.Be able to localize the placenta in T3 , FH activity
4% of women may develop antepartum hemorrhage( bleeding from or in to
the genital tract from 24 weeks gestation and prior to the birth of baby)
Causes:
placenta previa (1/200)
placental abruption (1/100)
uterine rupture (<1% in scarred uterus)
vasa previa (1/2000-3000)
Abruptio placenta
Premature separation of normally implanted placentae. The bleeding from A.P
insinuate itself between the membrane and uterus, ultimately blood escaping
through the cervix causing external bleeding, less often doesn't escape
externally
but is retained between the detached placenta and the uterus leading to
concealed hemorrhage.
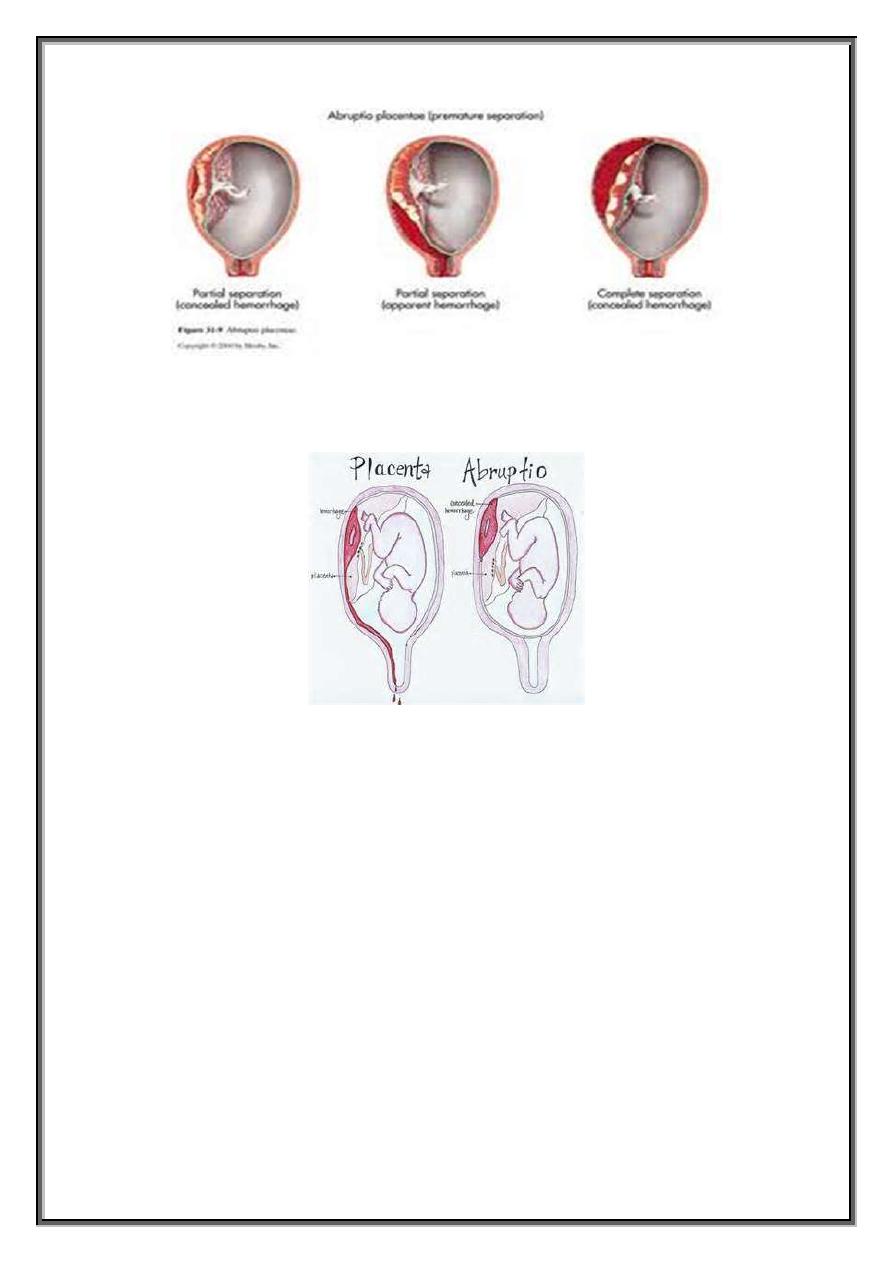
Abruption placenta either total separation of placenta or partial. Concealed Hg.
Carries greater maternal and fetal risk and hazards(consumptive
coagulopathy, extent of Hg.readily appreciated, diagnosis typically delayed)
Antepartum hemorrhage
Gynecology
2
Significance
A.P severely depend on who quickly the woman is seen following symptom
onset, with delay extensive separation occurs causing fetal death.
Incidence 1/100 deliveries.
Risk factors
Age increase incidence of A.P with maternal age 2.3 times in woman
above 40 Y.O
Parity higher rate of A.P with increase parity
Race and ethnicity A.P common in African-American and Caucasian
women(1-200), Asian (1-300), Latin American(1-450)
Familial woman with sever abruption risk to her sister double
HT(gestational, chronic, PE or combination increased incidence of
abruption), severity of HT does not correlate with increased incidence.
PROM, preterm delivery, 3 fold risk of A.P with PROM and the risk
increase with infection(because inflammation and infection is primary
cause of abruption)
Smoking 2 fold increase with smoking, 5-8 fold if smoking with chronic
HT
Cocaine abuse
Thrombophilia's(inherited or acquired, factor V leiden or
prothrombinogen mutation)
Traumatic abruption like motor vehicle accident or physical violence
Antepartum hemorrhage
Gynecology
3
Leiomyoma specially if located behind the placental implantation site
predispose to abruption.
Recurrent abruption specially that cause fetal death have higher
recurrence rate.
Pathology
Placental abruption is initiated by Hg. Into decidua basalis then decidua splits,
leaving a thin layer adhered to the myometrium.
The process in its earliest stage consist of development of decidual hematoma
that is leads to separation, compression and ultimate destruction of the
placenta adjacent to it.
Histological inflammation and infection lead to abruption.
In early stage, no clinical symptom, discovered upon examination of the
freshly delivered placenta.
Concealed Hg
.
1. Effusion behind the placenta but its margin remain adherent.
2. Placenta completely separated but the membrane retain their attachment to
the uterine wall.
3. Blood cross the amniotic cavity after breaking through the membrane.
4. The fetal head is so closely applied the lower uterine segment that blood
cannot makes its way.
Chronic placental abruption : Hg with retro placental hematoma formation is
somehow arrested completely without delivery.
Fetomaternal Hg. Bleeding in A.P always almost maternal(separation with in
maternal decidua), non-traumatic abruption only 10 ml fetal blood while in
traumatic abruption more fetal blood because tear from placental surface
rather than separation.
Clinical diagnosis:
The sign and symptoms of A.P vary considerably, external bleeding can be
profuse with placenta not completely separated(no fetal compromise), rarely
no external bleeding with placenta completely separated(fetus dead)
DIC(consumptive coagulopathy)
Abdominal pain, uterine tenderness, back pain.
Preterm labor initially diagnosed, frequent uterine contraction and persistent
uterine hyper tonus.
Sonographically infrequent confirms the diagnosis of placental abruption at
least acutely because the placenta and fresh clot have similar sonographic
finding.
D.DX
Sever abruption obvious
Mild-moderate, any vaginal bleeding with a life fetus necessary to exclude P.P
and other cause of bleeding by clinical and sonographic assessment.
Antepartum hemorrhage
Gynecology
4
Painful uterine bleeding---A.P
Painless uterine bleeding---P.P
Labor accompany previa may cause pain suggestive placental abruption.
Pain from abruption may mimic labor, it may be painless especially with
posterior placenta, so the cause of bleeding remain obscure even after
delivery.
Complication
1. Shock in A.P disproportionate to amount of Hg., placental thromboplastin
enter maternal circulation---intravascular coagulation, hypovolemic shock seen
in 1/2 of patient, oliguria from decrease renal perfusion which is responsive to
vigorous I.V fluid and blood infusion.
2. Consumptive coagulopathy A.P is one of the most common cause of
coagulopathy in obstetric. 1/3 of A.P that kill the baby have measurable
coagulopathy, hypofibrinogenaemia less than 150 mg/dl, elevated FDP&D-
dimer, coagulopathy higher with concealed A.P because intrauterine pressure
higher thus forcing thromboplastin into maternal venous system, procougulant
also consumed in retro placental clot.
Thrombocytopenia may or may not accompany hypofibrinogenimia, but it is
common after repeated blood transfusion.
3. renal failure acute renal failure is seen in sever A.P sp. If treat of
hypovolaemia is delayed or incomplete, most cases are reversible.
4. Sheehan syndrome sever intra partum or postpartum is rarely followed by
pituitary failure(failure of lactation, amenorrhea, breast atrophy, loss of pubic
&axillary hair, adrenal cortical insufficiency)
5. couvelarae uterus wide spread extravasation of blood into uterine
musculature beneath uterine serosa, sometime beneath tubal serosa, broad
ligament ovaries, free in the peritoneal cavity, this myometrial Hg. Interfere
with myometrium contraction cause atonia.
6. adult respiratory distress syndrome, multiorgan failure, death.
7. fetal complication (growth restriction with chronic abruption, fetal hypoxia or
asphyxia, preterm birth, perinatal mortality.
Management
Patient suspected to have A.P should have rapid initial evaluation and the
subsequent Mx. Depend on
1. Gestational age
2. Severity of A.P
3. Status of the mother and fetus
Antepartum hemorrhage
Gynecology
5
Most cases hypovolemia so
– continuous fetal monitoring – I.V access 2
wide bore IV cannula
-pulse &BP closely monitored
-Foleys catheter, maternal UOP hourly monitored(30 ml/hr)
-CBC, blood group ,RH, PT,PTT
-blood and its product replacement(FFP,cryoprecipitate&platelets),maintain
the hematocrit above 30%(300 ml Packed RBC contain 200 ml RBC rise
hematocrit 3-4% in absence of continuous bleeding, give six unit of platelet if
marked thrombocytopenia(less 50,000/microl) with serious bleeding or
planned C/S, FFP or cryoprecipitate is indicated for fibrinogen level less than
150.
Subsequent management
Live fetus near term
the fetus should delivered by quickest safest mothed,
vaginal delivery is safest, C/S indicated if FH tracing is not reassuring, there is
ongoing major blood loss or other serious maternal complication, vaginal
delivery contraindicated.
Live birth remote from term
FH reassuring, stable maternal condition, delaying
delivery near term, glucocorticoid
Feta death
delivery mode vaginally to decrease maternal morbidity and
mortality, unless CI to vaginal delivery, or urgent delivery needed to
stabilization maternal condition.



