Upper GI Bleeding&Portal Hypertension
Dr. Ali JafferUpper GI surgeon
Background
Bleeding derived from a source proximal to the ligament of Treitz.Bleeding from the upper GI tract is approximately 4 times more common than bleeding from the lower GI tract.
Mortality rates from UGIB are 6-10% overall.
Comorbid diseases increase the death rate.
Rebleeding and continued bleeding is a significant factor of mortality.
Aetiology
Causes of upper gastrointestinal bleeding.Condition %
Ulcers 60
Oesophageal 6
Gastric 21
Duodenal 33
Erosions 26
Oesophageal 13
Gastric 9
Duodenal 4
Mallory–Weiss tear 4
Oesophageal varices 4
Tumour 0.5
Vascular lesions, e.g. Dieulafoy’s disease 0.5
Others 5
Prognosis
The following risk factors are associated with an increased mortality, recurrent bleeding, the need for endoscopic hemostasis, or surgery :
1. Age older than 60 years
2. Severe comorbidity
3. Active bleeding (eg, witnessed hematemesis, red blood per nasogastric tube, fresh blood per rectum)
4. Hypotension
5. Red blood cell transfusion greater than or equal to 6 units
6. Inpatient at time of bleed
7. Severe coagulopathy
Patients who present in hemorrhagic shock have a mortality rate of up to 30%
History
Important informationpotential comorbid conditions,
medication history, and potential toxic exposures
severity, timing, duration, and volume of the bleeding
Hematemesis
Melena
Hematochezia
Syncope
Dyspepsia
Epigastric pain
Heartburn
Diffuse abdominal pain
Dysphagia
Weight loss
Jaundice
Physical Examination
The goal; to evaluate for shock and blood loss.
Assessing the patient for hemodynamic instability and clinical signs of poor perfusion is important early in the initial evaluation to properly triage patients with massive hemorrhage.
Worrisome clinical signs and symptoms of hemodynamic compromise include
Tachycardia of more than 100 beats per minute (bpm)Systolic blood pressure of less than 90 mm Hg,
Cool extremities, syncope, and other obvious signs of shock,
Ongoing brisk hematemesis,
The occurrence of maroon or bright-red stools, which requires rapid blood transfusion.
Pulse and blood pressure should be checked with the patient in supine and upright positions to note the effect of blood loss. Significant changes in vital signs with postural changes indicate an acute blood loss of approximately 20% or more of the blood volume.
Signs of chronic liver disease should be noted, including spider angiomata, gynecomastia, splenomegaly, ascites, ....etc.
nodular liver, an abdominal mass, and enlarged and firm lymph nodes.
Work upAssessment of hemorrhagic shock
patients who present in hemorrhagic shock have a mortality rate of up to 30%
Estimated Fluid and Blood Losses in Shock
Class 1
Class 2Class 3
Class 4Blood Loss, mL
Up to 750750-1500
1500-2000
>2000
Blood Loss,% blood volume
Up to 15%
15-30%
30-40%
>40%
Pulse Rate, bpm
< 100
>100
>120
>140
Blood Pressure
Normal
Normal
Decreased
Decreased
Respiratory Rate
Normal or Increased
Decreased
Decreased
Decreased
Urine Output, mL/h
>35
30-40
20-30
14-20
CNS/Mental Status
Slightly
anxious
Mildly
anxious
Anxious,
confused
Confused,
lethargic
Work up
Hemoglobin Value and Type and Crossmatch Blood
CBC should be checked frequently (4-6h) during the first day.
The patient should be crossmatched for 2-6 units, based on the rate of active bleeding.
Patients with significant comorbid conditions (eg, advanced cardiovascular disease) should receive blood transfusions to maintain myocardial oxygen delivery to avoid myocardial ischemia.
The more units required, the higher the mortality rate.
Operative intervention is indicated once the blood transfusion number reaches more than 5 units.
Coagulation Profile
The patient's prothrombin time (PT), activated partial thromboplastin time (PTT), and international normalized ratio (INR) should be checked to document the presence of coagulopathy. The coagulopathy may be consumptive and associated with a thrombocytopeniaWork up
EndoscopyDiagnostic&theraputic
Endoscopy should be performed immediately after endotracheal intubation (if indicated), hemodynamic stabilization, and adequate monitoring in an intensive care unit (ICU) setting have been achieved.
Chest Radiography
Computed Tomography Scanning
Liver disease for cirrhosis, pancreatitis with pseudocyst and hemorrhage, aortoenteric fistula, and other unusual causes of upper GI hemorrhage.
Nuclear Medicine Scanning
Nuclear medicine scans may be useful in determining the area of active hemorrhage.
Angiography
Angiography may be useful if bleeding persists and endoscopy fails to identify a bleeding site.
Transcatheter arterial embolization (TAE) should be considered for all patients with a known source of arterial UGIB that does not respond to endoscopic management, with active bleeding and a negative endoscopy.
Nasogastric Lavage
PPIs
Treatment of underlying cause
Portal Hypertension
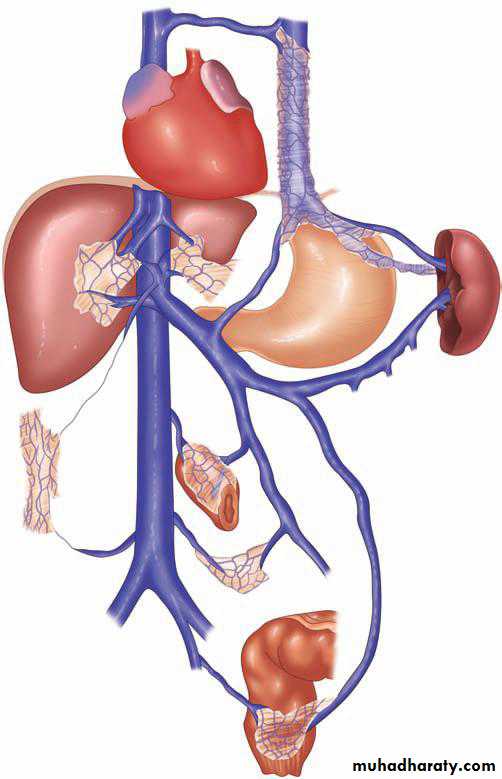
The portal venous system contributes approximately 75% of the blood and 72% of the oxygen supplied to the liver.
In the average adult, 1000 to 1500 mL/min of portal venous blood is supplied to the liver.
The normal portal venous pressure is 5 to 10 mmHg, and at this pressure, very little blood is shunted from the portal venous system into the systemic circulation.
As portal venous pressure increases, the collateral communications with the systemic circulation dilate, and a large amount of blood may be shunted around the liver and into the systemic circulation.
Lower oesophagus; Left gastric veins (portal system) -> lower branches of oesophageal veins (systemic veins)
Upper part of anal canal; Superior rectal veins (portal) -> inferior and middle rectal veins (systemic)
Umbilicus; Paraumbilical veins (portal) -> epigastric veins (systemic)
Area of the liver; Intraparenchymal branches of right division of portal vein (portal) -> retroperitoneal veins (systemic)
Hepatic and splenic flexures; Omental and colonic veins (portal) -> retroperitoneal veins (systemic)
Aetiology of portal hypertension
PresinusoidalSinistral/extrahepatic
Splenic vein thrombosis
Splenomegaly
Splenic arteriovenous fistula
Intrahepatic
Schistosomiasis
Congenital hepatic fibrosis
Nodular regenerative hyperplasia
Idiopathic portal fibrosis
Myeloproliferative disorder
Sarcoid
Graft-versus-host disease
Sinusoidal
Intrahepatic
Cirrhosis
Viral infection
Alcohol abuse
Primary biliary cirrhosis
Autoimmune hepatitis
Primary sclerosing cholangitis
Metabolic abnormality
Postsinusoidal
Intrahepatic
Vascular occlusive disease
Posthepatic
Budd-Chiari syndrome
Congestive heart failure
Inferior vena caval web
Constrictive pericarditis
Portal hypertension per se produces no symptoms, it is usually diagnosed following presentation with decompensated chronic liver disease and
encephalopathy, ascites or variceal bleeding.
Management of bleeding varices
General resuscitationMedical emergency
ICU
Two large pore peripheral canulae
Resuscitation, avoid fluid overload (why?)
Correction of coagulopathy; Vit K(10mg) i.v., tranexamic acid (1g i.v), FFP, platelet transfusion
Activation of major blood transfusion protocol
Drug therapy (terlipressin) splanchnic vasocinstriction
Prophylactic antibiotics
Endoscopy ; 50% PHT non variceal bleeding
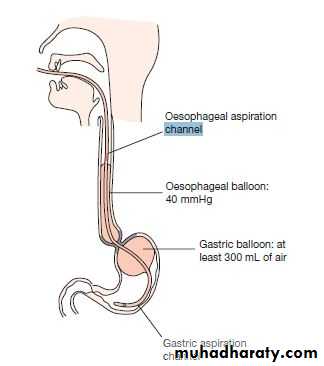
Sengstaken-Blakemore, temporary control; Once inserted, the gastric balloon is inflated with 300 mL of air and retracted to the gastric fundus, where the varices at the oesophagogastric junction are tamponaded by the subsequent inflation of the oesophageal balloon to a pressure of 40 mmHg. The balloons should be temporarily deflated after 12 hours to prevent pressure necrosis of the oesophagus.
Management of bleeding varices
Endoscopic treatment of varices
Endoscopic band ligation
Endoscopic sclerotherapy
Transjugular intrahepatic portosystemic stent shunts
the main treatment of variceal haemorrhage that has not responded to drug treatment and endoscopic therapy.Complications:
Liver capsule perfuration…. Intraperitoneal hemorrhage
Occlusion resulting in further variceal bleeding
Post shunt encephalopathy 40% of cases
TIPS stenosis (50% after one year)
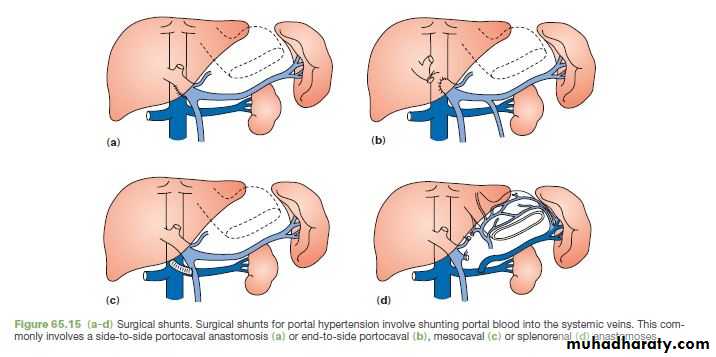
Surgical shunts for variceal haemorrhage
Surgical shunts are an effective method of preventing rebleeding from oesophageal or gastric varices, as they reduce the pressure in the portal circulation by diverting the blood into the low-pressure systemic circulation.
Long-term β-blocker therapy and chronic sclerotherapy or banding are the main alternatives.
Liver transplantation is the only therapy that will treat both portal hypertension and the underlying liver disease.
Ascites
Portal vein thrombosis is a common predisposing factor to the development of ascites in chronic liver disease. In patients without evidence of liver disease, malignancy is a common causeAspiration of the peritoneal fluid allows the measurement of protein content to determine whether the fluid is an exudate or transudate, an amylase estimation to exclude pancreatic ascites.
Cytology will determine the presence of malignant cells
Microscopy and culture will exclude primary bacterial and tuberculous peritonitis.
Treatment of ascites in chronic liver disease
Salt restrictionDiuretics
Abdominal paracentesis
TIPSS
Liver transplantation