II- TRANPLANATION IMMUNEPATHOLOGY
The major barrier to transplantation of organs from one individual to another of the same species ( allografts) is immunologic rejection of the transplanted tissue . Rejection is a complex phenomenon involving both cell- and antibody-mediated hypersensitivity reactions directed against histocompatibility molecules which is the cell surface antigens that determine whether the transplanted tissue is recognized as foreign or not.Transplanted tissue can be categorized as :-
1- Allograft if the donor and recipient are genetically non identical and same species (ex .kidney transplant from one individual to an other).
2- syngeneic graft or isograft the donor and recipient are genetically identical
ex. transplantation between twins.
3- Autolograft the donor and recipient are the same person ex .skin graft.
4- Xenograft the donor and recipient are different in species ex. graft of Baboon heart to human.
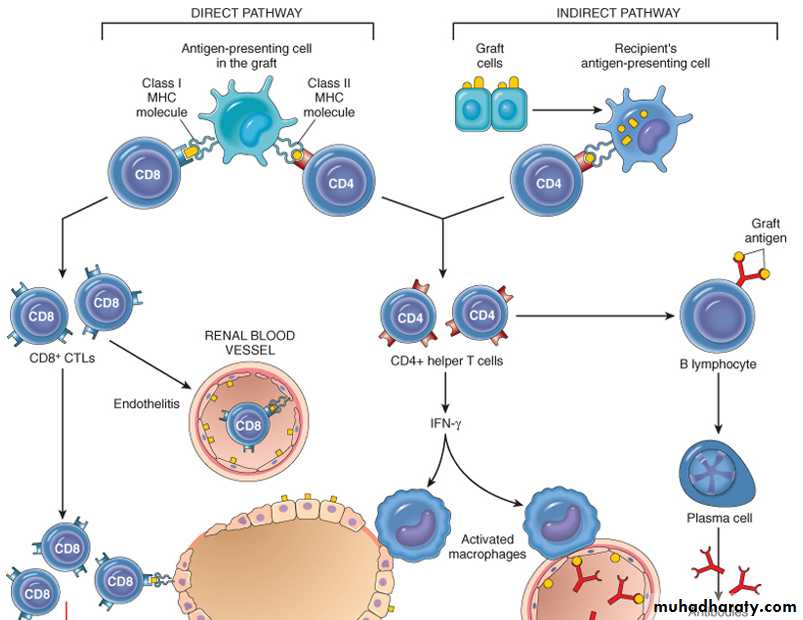
Immune Recognition of Allografts
Rejection of allografts is a response to MHC molecules, which are so polymorphic that no two individuals in an outbred population are likely to express exactly the same set of MHC molecules (except identical twins). There are two main mechanisms by which the host immune system recognizes and responds to the MHC molecules on the graft.1- Direct recognition. Donor APC migrate from the graft to secondary lymphoid tissue of recipient which carry donor class I and II MHC molecules . Host T cells directly recognize the allogeneic (foreign) MHC molecules that are expressed on graft cells. Because DCs in the graft express high levels of MHC , they are the most likely APCs in direct recognition. Host CD4+ helper T cells are triggered into proliferation and cytokine production by recognition of donor class II MHC molecules and drive the delay type hypersensitivity response. CD8+ T cells recognize class I MHC and differentiate into CTLs, which kill the cells in the graft.
2- Indirect recognition
- Host CD4+ T cells recognize donor MHC molecules after these molecules are picked up, processed, and presented by the host's own APCs. This is similar to the physiologic processing and presentation of other foreign (e.g., microbial) antigens. This form of recognition mainly activates DTH reaction.- Production of antibodies against graft alloantigens; if these antigens are proteins they are picked up by host B cells and presented to helper T cells, which then stimulate antibody responses.
Host Versus Graft Disease
If the transplanted graft bearing foreign MHC antigens ,the recipients immune system attack the donor cells of the transplanted organ .Rejection involves T Cell-Mediated Rejection and Antibody-Mediated Rejection .the initial target of the recipient is graft vasculature .There are three patterns of transplant rejection;-
1- Hyperacute Rejection. Occurs immediately (within minutes to hours) after transplantation, in kidney transplants as soon as blood flow from recipient to the donor organ begin ,it takes on cyanotic ,mottled appearance .
2- Acute Rejection occurs within days to weeks .Acute rejection is caused by both cellular and humeral immune mechanisms of transplantation .
3- Chronic Rejection occur (months to years) after transplantation. Manifested by vascular changes, interstitial fibrosis, and loss of renal parenchyma.
Graft Versus Host Disease
The cellular immune system of the transplanted graft (donor T cells) recognizes and attack the recipient MHC . occur mainly in :-1- Bone marrow transplant.
2- After transplantation of solid organs rich in lymphoid cells (e g. The liver).
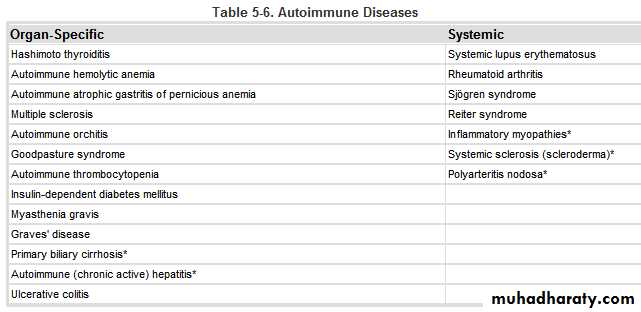
III- AUTOIMMUNE DISEASES
they are caused by inability of immune system to differentiate between self and non self antigens. Normally, there is high degree of immunological tolerance to self-antigens which prevent immune system from destroying the host. Autoimmune disorder are particular organ or cell type , or other affect multiple organs and systems.Immunological Tolerance
Immunological tolerance is unresponsiveness to an antigen during exposure of specific lymphocytes to that antigen.Self-tolerance refers to a lack of immune responsiveness to one's own tissue antigens. During the generation of billions of antigen receptors in developing T and B lymphocytes, it is not surprising that receptors are produced that can recognize self-antigens.
Several mechanisms prevent immune reactions against one's own antigens :-
1- Central tolerance. This refers to deletion or death of self-reactive T and B lymphocytes during their maturation in central lymphoid organs (i.e., in the thymus for T cells and in the bone marrow for B cells).
2- Peripheral tolerance is deletion of self-reactive T and B lymphocytes that escaped from central lymphoid organs . Self reactive B lymphocytes are deleted in spleen and lymph nodes . self-reactive T lymphocytes remain inactive or deleted so that they cannot recognize self antigens .
Several mechanisms in the peripheral tissues that silence such autoreactive T cells have been identified:
1- Anergy : its functional inactivation (rather than death) of lymphocytes induced by encounter with antigens.
2- Suppression of responses of T lymphocytes to self-antigens by regulatory T cells which secreting immunosuppressive cytokines (e.g., IL-10 and TGF-β) .
3- Activation-induced cell death: it involves apoptosis of mature lymphocytes as a result of self-antigen recognition.
4-Antigen sequestration : some antigens are hidden from the immune system because the tissues in which these antigens are located , do not communicate with blood and lymph . These organs called immune – privileged sites because its difficult to induce immune responses to antigens in these sites.
Mechanisms of Autoimmunity
The defect in self-tolerance and the development of autoimmunity are probably related to the inheritance of various susceptibility genes and changes in tissues, often induced by infections or injury, that alter the recognition of self-antigens.Genetic Factors in Autoimmunity
Genetic susceptibility play an important role in the development of autoimmune diseases.
Autoimmune diseases have a tendency to run in families, and there is a greater incidence of the same disease in monozygotic than in dizygotic twins . Several autoimmune diseases are linked with the HLA locus .
Role of Infections and Tissue Injury
A variety of microbes, including bacteria, mycoplasmas, and viruses, are considered as triggers for autoimmunity.Microbes may induce autoimmune reactions by several mechanisms:
Viruses and other microbes, particularly certain bacteria such as streptococci and Klebsiella organisms, may share cross-reacting epitopes with self-antigens, such that responses to the microbial antigen may attack self-tissues. This phenomenon is called molecular mimicry. It is the probable cause of a few diseases, like rheumatic heart disease, in which an immune response against streptococci cross-reacts with cardiac antigens.
Examples of autoimmune diseases
1-Systemic Lupus Erythematosus (SLE)
it affects principally the skin, kidneys, serosal membranes, joints, and heart. Immunologically , the disease is caused by autoantibodies, some of which are directed against nuclear antigens and formation of circulating immune complexes .
a large number of autoantibodies is produced that can damage tissues either directly or in the form of immune complex deposits.
the Autoantibodies in SLE are Antibodies have been identified against a host of nuclear and cytoplasmic components of the cell that are specific to neither organs nor species. Another group of antibodies is directed against surface antigens of blood cells, while yet another is reactive with proteins in complex with phospholipids (antiphospholipid antibodies.
Rheumatoid Arthritis (RA )
is a chronic inflammatory disease that affects mainly the joints, especially small joints, but can affect multiple tissues . The disease is caused by an autoimmune response against an unknown self antigen(s), which leads to T-cell reactions in the joint with production of cytokines that activate phagocytes that damage tissues and stimulate proliferation of synovial cells (synovitis). The cytokine TNF plays a central role . Antibodies may also contribute to the disease.IV- IMMUNE DEFICIENCY DISEASES
Immune deficiency diseases may be caused by inherited defects affecting immune system development, or they may result from secondary effects of other diseases (e.g., infection, malnutrition, aging, immunosuppression, autoimmunity, or chemotherapy). Clinically, patients with immune deficiency present with increased susceptibility to infections as well as to certain forms of cancer.There are two types of immune deficiency diseases:-
1- primary immune deficiencies.
2- secondary immune deficiency (Aquired Immunodeficiency Syndrome AIDS )
1- Primary Immune Deficiencies
(Congenital) Immune DeficiencyCaused by mutations in genes involved in lymphocyte maturation or function, or in innate immunity . They have increased susceptibility to infections in early life.
2- Secondary Immune Deficiencies
Immune deficiencies secondary to other diseases or therapies are much more common than the primary disorders. It occurs in patients with malnutrition, infection, cancer, renal disease, or sarcoidosis. the most common cases of immune deficiency are therapy-induced suppression of the bone marrow and lymphocyte function.
The most important example of Secondary Immune Deficiencies is Acquired Immunodeficiency Syndrome(AIDS)
Acquired Immunodeficiency Syndrome(AIDS)
AIDS is a retroviral disease caused by the human immunodeficiency virus (HIV). It is characterized by infection and depletion of CD4+ T lymphocytes, and by profound immunosuppression leading to opportunistic infections, secondary neoplasms, and neurologic manifestations.
the major routes of HIV infection are :-
1- Sexual contact.
2- Parenteral inoculation.
3- Passage of the virus from infected mothers to their newborns.
4- Random recipients of blood transfusion.
Pathogenesis
The two major targets of HIV infection are the immune system and the CNS.
Virus entry into cells:
Requires CD4 molecules which acts as a high-affinity receptor for the virus and co-receptors, which are receptors for chemokines ; involves binding and fusion of viral with the cell . The main cellular targets are CD4+ helper T cells, macrophages and DCs .
Viral replication:
provirus genome integrates into host cell DNA; viral gene expression is triggered by stimuli that activate infected cells (e.g., infectious microbes, cytokines produced during normal immune responses).Progression of infection:
acute infection of mucosal T cells and DCs ; viremia with dissemination of virus; latent infection of cells in lymphoid tissue; continuing viral replication and progressive loss of CD4+ T cells.
Mechanisms of immune deficiency:
Loss of CD4+ T cells is occur due to :
1- T-cell death during viral replication .
2- Apoptosis as a result of chronic stimulation .
3-Decreased thymic output.
4- Defective macrophage and DC functions .
5- Destruction of architecture of lymphoid tissues .
Clinical Features
The clinical manifestations of HIV infection range from a mild acute illness to severe disease. the typical adult patient with AIDS presents with fever, weight loss, diarrhea, generalized lymphadenopathy, multiple opportunistic infections, neurologic disease, and secondary neoplasms.