Hemodynamic Disorders, Thrombosis, and Shock
The health of cells and tissues depends not only on an intact circulation to deliver oxygen and remove wastes but also on normal fluid homeostasis. Normal fluid homeostasis requires vessel wall integrity as well as maintenance of intravascular pressure and osmolarity within certain physiologic ranges.EDEMA (oedema )
Edema is water extravasation into interstitial spaces .Or abnormal and excessive accumulation of free fluid in the interstitial tissue spaces and serous cavities .
fluid collections in different body cavities are designated as
- (Pleural cavity ) hydrothorax.
- ( Pericardial cavity ) hydropericardium.
- (peritoneal cavity ) hydroperitoneum (which is also is called Ascites which is collection of fluids in peritoneal cavity ).
Anasarca is a severe and generalized edema with profound subcutaneous tissue swelling.
mechanism of inflammatory edema
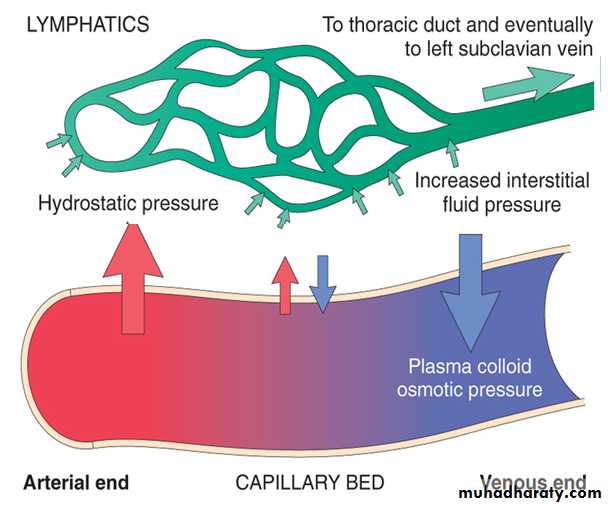
The movement of fluid between vascular and interstitial spaces is controlled mainly by the opposing effects of vascular hydrostatic pressure and plasma colloid osmotic pressure. Normally, the exit of fluid from the arteriolar end of the microcirculation into the interstitium is balanced by inflow at the venular end; the lymphatics drain a small residual amount of excess interstitial fluid . Either increased capillary pressure or diminished colloid osmotic pressure can result in increased interstitial fluid. As extravascular fluid accumulates in either case, the increased tissue hydrostatic and plasma osmotic pressures eventually achieve a new equilibrium, and water re-enters the venules .Excess interstitial edema fluid is removed by lymphatic drainage, ultimately returning to the bloodstream via the thoracic duct ; clearly, lymphatic obstruction (e.g., due to scarring or tumor) can also impair fluid drainage and cause edema.
Types of edema
1- inflammatory edema is a protein- rich exudate with a specific gravity that is usually greater than 1.020, occur due to increased vascular permeability .2-non inflammatory edema is typically a protein-poor transudate ; it has a specific gravity less than 1.012occur due to other reasons other than inflammation.
causes of non inflammatory edema
1- Increased Hydrostatic Pressure.
2- Reduced Plasma Osmotic Pressure (Hypoproteinemia).
3- Lymphatic Obstruction.
4- Sodium and Water Retention .
Factors affecting fluid transit across capillary walls. Capillary hydrostatic and osmotic forces are normally balanced so there littlie net net movement in to the interstitium .
1- Increased Hydrostatic Pressure.
Localized increases in intravascular pressure can result from impaired venous return; for example:-A- deep venous thrombosis in lower extremity can cause edema restricted to the distal portion of the affected leg.
B- portal hypertension caused by liver cirrhosis .this produce a transudate in the peritoneal cavity .
C- pressure of gravid uterus on the iliac veins produces congestion and edema of the lower limbs.
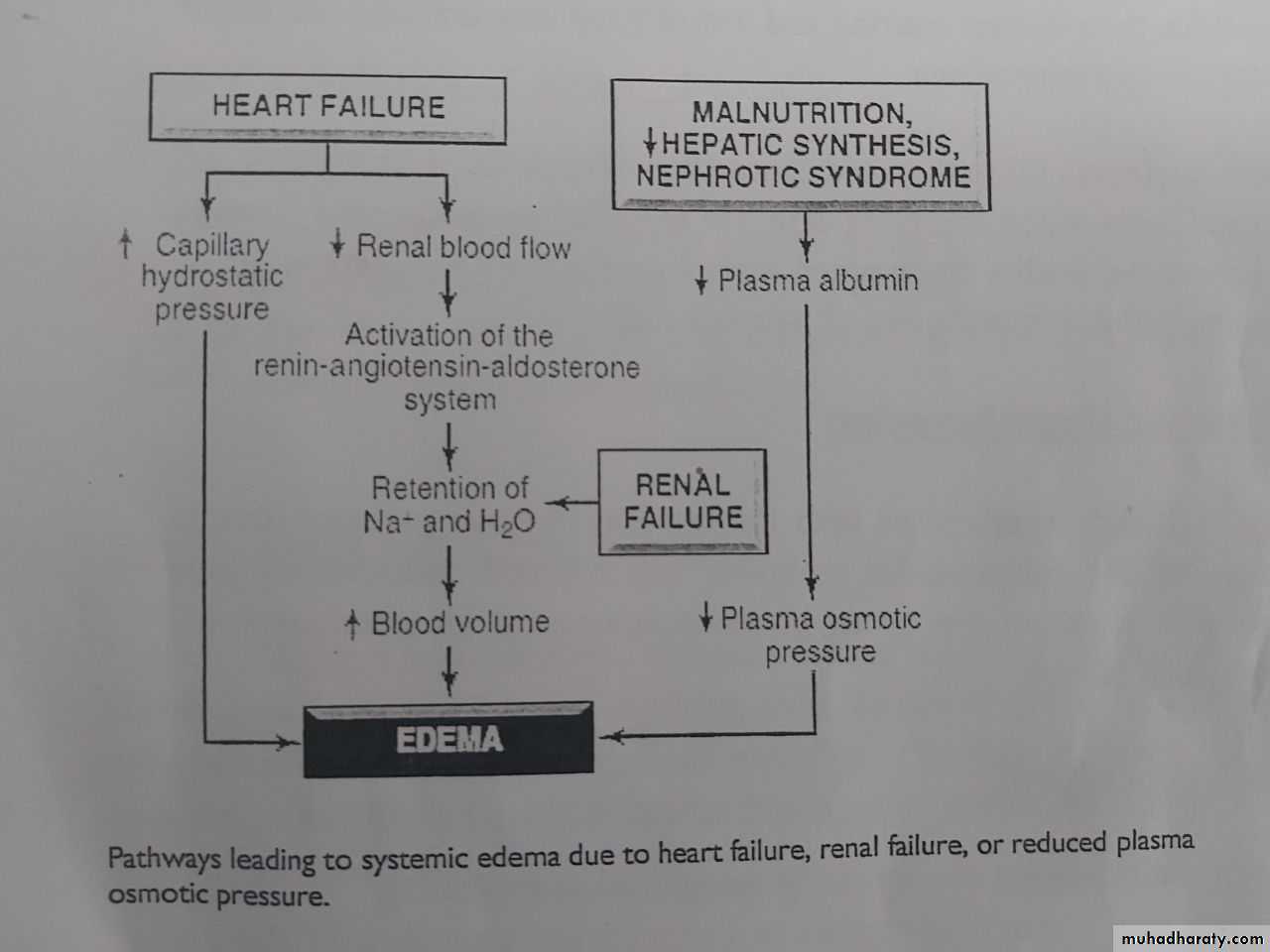
Generalized increases in venous pressure, with resultant systemic edema, occur most commonly in congestive heart failure in which reduced cardiac output translates into reduced renal perfusion .
Renal hypoperfusion in turn triggers the renin – angiotensin -aldosterone axis, inducing sodium and water retention by the kidneys . This mechanism normally functions to increase intravascular volume and thereby improve cardiac output to restore normal renal perfusion. However, if the failing heart cannot increase cardiac output, the extra fluid load causes increased venous pressure and, eventually, edema .
2- Reduced Plasma Osmotic Pressure
Albumin is the serum protein most responsible for maintaining intravascular colloid osmotic pressure; reduced osmotic pressure occurs when:-1- albumin is inadequately synthesized or is lost from the circulation. An important cause of albumin loss is the nephrotic syndrome in which glomerular capillary walls become leaky; patients typically present with generalized edema.
2- albumin synthesis is reduced occurs in the diffuse liver diseases (e.g., liver cirrhosis).
3- protein malnutrition .
In each case, reduced plasma osmotic pressure leads to a net movement of fluid into the interstitial tissues resulting edema.
Pathways leading to systemic edema due to primary heart failure, primary renal failure, or reduced plasma osmotic pressure
3- Lymphatic Obstruction
Obstruction of lymphatic drainage and consequent lymphedema is usually localized; it can result from inflammatory or neoplastic obstruction. For example, the parasitic infection filariasis can cause extensive inguinal lymphatic and lymph node fibrosis. The resultant edema of the external genitalia and lower limbs . Cancer of the breast can be treated by resection and/or irradiation of the associated axillary lymph nodes; the resultant scarring and loss of lymphatic drainage can cause severe upper extremity edema.In breast carcinoma infiltration and obstruction of superficial lymphatics can also cause edema of the overlying skin, the so-called peau d'orange (orange peel) appearance. Such a finely pitted surface results from an accentuation of depressions in the skin at the site of hair follicles.
4- Sodium and Water Retention
Increased salt-with the obligate accompanying water-causes both increased hydrostatic pressure (due to expansion of the intravascular volume) and reduced vascular osmotic pressure. Salt retention can occur with any compromise of renal function, as in poststreptococcal glomerulonephritis and acute renal failure .Morphology of edema
Macroscopically edema is most easily recognized as swelling .Microscopically edema fluid is appear as a clearing and separation of the extracellular matrix elements with subtle cell swelling.
Although any organ or tissue in the body may be involved, edema is most commonly encountered in subcutaneous tissues, lungs, and brain .
Subcutaneous edema can be diffuse or more prominent in regions with high hydrostatic pressures ; the ultimate distribution depends on the underlying etiology. Even diffuse edema is usually more prominent in certain body areas as a result of the effects of gravity; a gravity-dependent distribution is referred to as dependent edema (e.g., involving the legs when standing, or involving the sacrum when recumbent). Finger pressure over significantly edematous subcutaneous tissue displaces the interstitial fluid and leaves a finger-shaped depression, so-called pitting edema.
Edema due to renal dysfunction or nephrotic syndrome is generally more severe than cardiac edema and affects all parts of the body equally.
Pulmonary edema is a common clinical problem most frequently seen in left ventricular failure. but it also occurs in renal failure, acute respiratory distress syndrome (ARDS pulmonary infections, and hypersensitivity reactions. The lungs typically weigh two to three times their normal weight, and sectioning reveals frothy, sometimes blood-tinged fluid, edema fluid, and extravasated red cells.
brain edema may be localized to sites of focal injury (e.g., infarct, abscesses or neoplasms) or may be generalized, as in encephalitis, hypertensive crises, or obstruction to the brain's venous outflow. Trauma may result in local or generalized edema, depending on the nature and extent of the injury.
Clinical Correlation of edema
depending on its location ,edema may have
1- Subcutaneous tissue edema in cardiac or renal failure is important primarily because it indicates underlying disease.
2- in the lung ,edema fluid will fill alveoli and can result in life threatening breathing difficulties .
3-Brain edema is serious and can be rapidly fatal.
HYPEREMIA AND CONGESTION
hyperemia and congestion both indicate a local increased volume of blood in a particular tissue.Hyperemia is an active process resulting from increased blood flow due to arteriolar dilation (e.g., at sites of inflammation or in skeletal muscle during exercise). The affected tissue is redder than normal because of engorgement with oxygenated blood.
Congestion is a passive process resulting from impaired venous return out of a tissue. It may occur systemically, as in cardiac failure, or it may be local, resulting from an isolated venous obstruction. The tissue has a blue-red color (cyanosis), especially as worsening congestion leads to accumulation of deoxygenated hemoglobin in the affected tissues
Congestion of capillary beds is closely related to the development of edema, so that congestion and edema commonly occur together.
MORPHOLOGY
Macroscopically the cut surfaces of hyperemic or congested tissues are hemorrhagic and wet.Microscopically,
Acute pulmonary congestion is characterized by alveolar capillaries engorged with blood; there may also be associated alveolar septal edema and/or focal minute intra-alveolar hemorrhage.
Chronic pulmonary congestion the septa become thickened and fibrotic, and the alveolar spaces may contain numerous hemosiderin-laden macrophages ("heart failure cells").
Acute hepatic congestion the central vein and sinusoids are distended with blood, and there may even be central hepatocyte degeneration; the periportal hepatocytes, better oxygenated because of their proximity to hepatic arterioles, undergo less severe hypoxia and may develop only fatty change.
Chronic passive congestion of the liver the central regions of the hepatic lobules are grossly red-brown and slightly depressed (because of a loss of cells) and are accentuated against the surrounding zones of uncongested tan, sometimes fatty, liver ("nutmeg liver ). Microscopically, there is centrilobular necrosis with hepatocyte drop-out, hemorrhage, and hemosiderin-laden macrophages
Liver with chronic passive congestion and hemorrhagic necrosis. A, Central areas are red and slightly depressed compared with the surrounding tan viable parenchyma, forming a "nutmeg liver" (so called because it resembles the alternating of light and dark seen when a whole nutmeg is cut).
HEMORRHAGE
Hemorrhage is extravasation of blood from vessels into the extravascular space .Causes
1- Hemorrhage most often caused by trauma.
2- Chronic congestion will result in capillary rupture.
3- Coagulation disorder.
4- Vascular injury, including trauma , atherosclerosis , inflammatory or neoplastic erosion of the vessel wall.
Types of hemorrhage
Hemorrhage can be external or can be confined within a tissue.1- Hematomas : accumulated hemorrhage can be confined within a tissue, can be relatively insignificant (e.g., a bruise) or can involve so much bleeding as to cause death (e.g., a massive retroperitoneal hematoma resulting from rupture of a dissecting aortic artery.
2- Petechiae : minute (1- to 2-mm) hemorrhages into skin, mucous membranes, or serosal surfaces and typically associated with locally increased intravascular pressure, low platelet counts (thrombocytopenia), defective platelet function, or clotting factor deficiencies.
3- Purpura : slightly larger (3- to 5-mm) hemorrhages can be associated with many of the same disorders that cause petechiae ; in addition, purpura can occur with trauma, vascular inflammation (vasculitis).
4-Ecchymoses : larger (1- to 2-cm) subcutaneous hematomas (bruises) . The erythrocytes in these local hemorrhages are phagocytosed and degraded by macrophages; the hemoglobin (red-blue color) is enzymatically converted into bilirubin (blue-green color) and eventually into hemosiderin (golden-brown), accounting for the characteristic color changes in a hematoma.
5- Large accumulations of blood in one or another of the body cavities are called hemothorax ( in pleura ) , hemopericardium (in pericardium , hemoperitoneum( in peritonium ), or hemarthrosis (in joints).
Clinical significance of hemorrhage
1-Rapid removal of as much as 20% of the blood volume or slow losses of even larger amounts may have little impact in healthy adults.2-Greater losses, however, can cause hemorrhagic (hypovolemic) shock .
3- The site of hemorrhage is also important; bleeding that would be trivial in the subcutaneous tissues may cause death if located in the brain.
4- Chronic or recurrent external blood loss (e.g., a peptic ulcer or menstrual bleeding) causes a net loss of iron, frequently culminating in an iron deficiency anemia.