Cellular Events: Leukocyte Recruitment and Activation
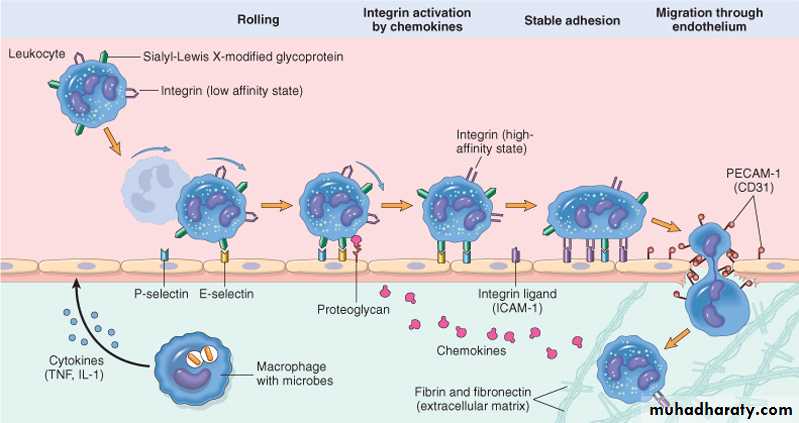
-Leukocyte Recruitmentthe sequence events in the recruitment of leukocytes from the vascular lumen to the extravascular space :consists of
1-margination, adhesion to endothelium, and rolling along the vessel wall.
2-firm adhesion to the endothelium.
3-transmigration between endothelial cells.
4-migration in interstitial tissues toward a chemotactic stimulus.
1
1-Margination and Rolling
As blood flows from capillaries into postcapillary venules ,the smaller red cells move faster than the larger white cells. As a result, leukocytes are pushed out of the central axial column and interact with lining endothelial cells. This process of leukocyte accumulation at the periphery of vessels is called margination. Subsequently, leukocytes tumble on the endothelial surface, transiently sticking along the way, a process called rolling.2
The weak and transient adhesions involved in rolling are mediated by the selectin family of adhesion molecules. Selectins are receptors expressed on leukocytes and endothelium.
The three members of this family are E-selectin (also called CD62E), expressed on endothelial cells; P-selectin (CD62P), present on endothelium and platelets; and L-selectin (CD62L), on the surface of most leukocytes.
The endothelial selectins are typically expressed at low levels or are not present at all on normal cells. They are up-regulated after stimulation by specific mediators. Therefore, binding of leukocytes is largely restricted to endothelium at sites of infection or tissue injury (where the mediators are produced).
3
2- firm Adhesion
firm adhesion to endothelial cells is mediated by integrins expressed on leukocyte cell surfaces interacting with their ligands on endothelial cells. integrins act as cell receptors for extracellular matrix . Integrins are normally expressed on leukocyte plasma membranes in a low-affinity form and do not adhere to their appropriate ligands until the leukocytes are activated by chemokines. Chemokines are chemoattractant cytokines that are secreted by many cells at sites of inflammation . other cytokines, notably TNF and IL-1 (also secreted at sites of infection and injury), activate endothelial cells to increase their expression of ligands for integrins.
3- Transmigration
leukocytes migrate through the vessel wall by squeezing between cells at intracellular junctions of endothelial cell . This extravasation of leukocytes called diapedesis.
4
4- Migration and chemotaxis
Migration of leukocytes is driven by chemokins produced in extravascular tissues, which stimulate movement of the leukocytes toward their chemical gradient. In addition, PECAM-1 (platelet endothelial cell adhesion molecule 1, also called CD31), a cellular adhesion molecule expressed on leukocytes and endothelial cells, mediates the binding events needed for leukocytes to traverse the endothelium. After passing through the endothelium, leukocytes cross vascular basement membranes by degrading them by secretion of collagenases.5
chemotaxis
After extravasating from the blood, leukocytes migrate toward sites of infection or injury along chemical gradient by a process called chemotaxisBoth exogenous and endogenous substances can be chemotactic for leukocytes, including
(1)bacterial products, particularly peptides
(2) cytokines, especially those of the chemokine family.
(3) components of the complement system, particularly C5a.
(4) products of the lipoxygenase pathway of arachidonic acid (AA) metabolism.
6
The type of emigrating leukocyte varies with the age of the inflammatory response and with the type of stimulus. In most forms of acute inflammation, neutrophils predominate in the inflammatory infiltrate during the first 6 to 24 hours and are replaced by monocytes in 24 to 48 hours. after entering tissues, neutrophils are short-lived-they die by apoptosis and disappear within 24 to 48 hours-while monocytes survive longer.
7
The complex process of leukocyte migration through blood vessels, The leukocytes first roll, then become activated and adhere to endothelium, then transmigrate across the endothelium, pierce the basement membrane, and migrate toward chemoattractants emanating from the source of injury. Different molecules play predominant roles in different steps of this process - selectins in rolling; chemokines (usually displayed bound to proteoglycans) in activating the neutrophils t\ao increase avidity of integrins; integrins in firm adhesion; and CD31 (PECAM-1) in transmigration. ICAM-1, intercellular adhesion molecule 1; IL-1, interleukin 1; PECAM-1, platelet endothelial cell adhesion molecule 1; TNF, tumor necrosis factor.
8
Leukocyte Activation
Once leukocytes have been recruited to the site of infection or tissue necrosis, they must be activated to perform their functions. Stimuli for activation include microbes, products of necrotic cells, and several mediators .Leukocytes express on their surface different kinds of receptors that sense the presence of microbes. These include
-Toll-like receptors which recognize endotoxin and other bacterial and viral products.
-Seven-transmembrane G-protein-coupled receptors, which recognize certain bacterial peptides.
Phagocytosis
Phagocytosis of particles, an early step in the elimination of harmful substances . Production of substances that destroy phagocytosed microbes and remove dead tissues; these leukocyte products include lysosomal enzymes and reactive oxygen and nitrogen and arachidonic acid metabolites and cytokines.
9
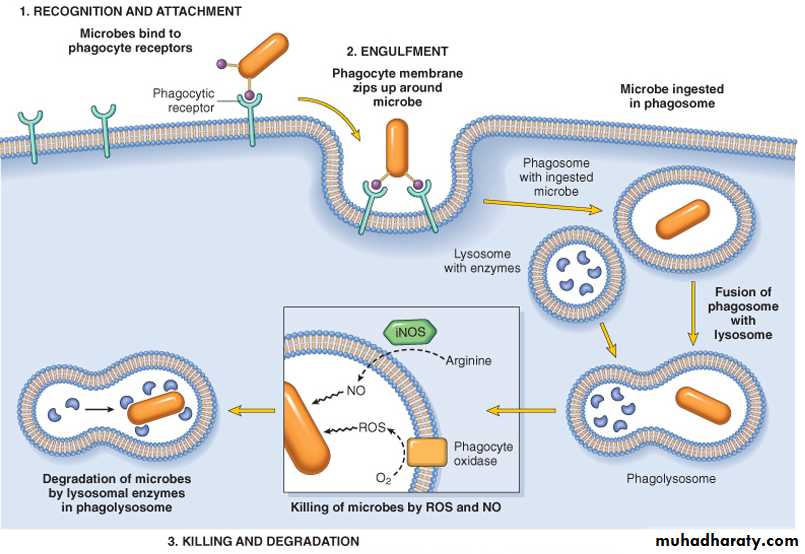
Phagocytosis consists of three distinct but interrelated steps :-
(1) recognition and attachment of the particle to the ingesting leukocyte.(2) engulfment, with subsequent formation of a phagocytic vacuole
(3) killing and degradation of the ingested material
10
(1) recognition and attachment of the particle to the ingesting leukocyte (opsonization)
Leukocytes bind and ingest most microorganisms and dead cells via specific surface receptors, which recognize either components of the microbes and dead cells, or host proteins (opsonins) , that coat microbes and target them for phagocytosis (a process called opsonization).
The most important opsonins are
1- Antibodies of the immunoglobulin G (IgG) class that bind to microbial surface antigens.
2- Breakdown products of the complement protein C3 .
3- plasma carbohydrate-binding lectins called collectins, which bind to microbial cell-wall sugar groups.
These opsonins either are present in the blood ready to coat microbes or are produced in response to the microbes.
11
2- engulfment
Binding of opsonized particles triggers engulfment; in addition, IgG binding to FcR and binding of complement products to C3 receptors induces cellular activation that enhances degradation of ingested microbes. In engulfment, pseudopods are extended around the object , eventually forming a phagocytic vacuole. The membrane of the vacuole then fuses with the membrane of a lysosomal granule, resulting in discharge of the granule's contents into the phagolysosome.12
3- Killing and Degradation of Microbes
The ultimate of the phagocytosis of microbes is killing and degradation of the ingested particles.The key steps in this reaction are the production of microbicidal substances within lysosomes and fusion of the lysosomes with phagosomes.
The most important microbicidal substances are reactive oxygen species (ROS) and lysosomal enzymes.
13
Phagocytosis of a particle (e.g., a bacterium) involves (1) attachment and binding of the particle to receptors on the leukocyte surface, (2) engulfment and fusion of the phagocytic vacuole with granules (lysosomes), and (3) destruction of the ingested particle. iNOS, Inducible nitric oxide synthase; NO, nitric oxide; ROS, reactive oxygen species.
14
Outcomes of Acute Inflammation
Outcomes of acute inflammation are depended on:-1-the nature and intensity of the injury,
2-the site and tissue affected,
3- the ability of the host to mount a response,
acute inflammation generally has one of four outcomes:-
1-Resolution .When the injury is limited or short-lived, when there has been no or minimal tissue damage, and when the tissue is capable of replacing any irreversibly injured cells, the usual outcome is restoration to histologic and functional normalcy.
15
2- Progression to chronic inflammation
may follow acute inflammation if1- the offending agent is not removed. In some instances, signs of chronic inflammation may be present at the onset of injury (e.g., in viral infections or immune responses to self-antigens).
2- Depending on continuing tissue injury, and capacity of the affected tissues to regrow, chronic inflammation may be followed by restoration of normal structure and function or may lead to scarring
16
3-Scarring or fibrosis
It means replacement destructed or injured tissue byfibrous connective tissue . This occur when large tissue destruction or if the inflammation occure in tissue that do not regenerate.
4- suppuration: means pus formation.
Pus : a perulent inflammatory exudate caused by pyogenic bacteria.
Pus is a mixture of :-
A- living and dead neutrophils.
B- bacteria.
C-cellular debris .
D-edema fluid .
Abscesses are focal collections of pus ,typically have central largely necrotic region rimmed by a layer of preserved neutrophils with surrounding zone of dilated vessels and fibroblast.
17
CHRONIC INFLAMMATION
Chronic inflammation is inflammation with prolonged duration (weeks to months to years) in which active inflammation, tissue injury, and healing proceed simultaneously. chronic inflammation is characterized by Infiltration with mononuclear cells including macrophages, lymphocytes, and plasma cells, Tissue destruction, largely induced by the products of the inflammatory cells, Repair, involving new vessel proliferation (angiogenesis) and fibrosis.
Acute inflammation may progress to chronic inflammation. This transition occurs when the acute response cannot be resolved, either because of the persistence of the injurious agent or because of interference with the normal process of healing.
18
causes of chronic inflammation
Chronic inflammation arises in the following settings:1- Persistent infections by microbes that are difficult to eradicate. These include mycobacteria , Treponema pallidum (causative organism of syphilis), and certain viruses and fungi, all of which tend to establish persistent infections .
2- Prolonged exposure to potentially toxic agents. Examples include non degradable exogenous materials such as inhaled particulate silica and talc .
3- Immune-mediated inflammatory diseases
- hypersensitivity diseases :- Diseases that are caused by excessive and inappropriate activation of the immune system. - autoimmune diseases:- immune reactions develop against the individual's own tissues .
19
Chronic Inflammatory Cells
1- MacrophagesMacrophages, the dominant cells of chronic inflammation, are tissue cells derived from circulating blood monocytes after their emigration from the bloodstream. Macrophages are normally diffusely scattered in most connective tissues, Macrophages also found in organs and named according to the site which is present such as
- the liver (where they are called Kupffer cells).
- spleen and lymph nodes (called sinus histiocytes).
- central nervous system (microglial cells).
- lungs (alveolar macrophages).
Together these cells comprise the so-called mononuclear phagocyte system, also known by the older name of reticulo-endothelial system.
macrophages act as filters for particulate matter, microbes, and senescent cells, as well as acting as sentinels to alert the specific immune system (T and B lymphocytes) to injurious stimuli.
20
2- Lymphocytes
Lymphocytes are mobilized to the setting of any specific immune stimulus (i.e., infections) as well as non-immune-mediated inflammation (e.g., due to infarction or tissue trauma). Both T and B lymphocytes migrate into inflammatory sites using some of the same adhesion molecule pairs and chemokines that recruit other leukocytes.
3- Eosinophils are characteristically found in
- inflammatory sites around parasitic infections
- as part of immune reactions mediated by IgE, typically associated with allergies. Eosinophil granules contain major basic protein, a highly charged cationic protein that is toxic to parasites but also causes epithelial cell necrosis .
21
3- Mast cells are widely distributed in connective tissues . And participate in both acute and chronic inflammatory responses. In individuals prone to allergic reactions , mast cells are "armed" with IgE antibody specific for certain environmental antigens.
4- Plasma cells develop from activated B lymphocytes and produce antibodies directed either against persistent antigens in the inflammatory site .
In some strong chronic inflammatory reactions, the accumulation of lymphocytes, macrophages and plasma cells may assume the morphologic features of lymphoid organs, and appear as lymph nodes, may even contain well-formed germinal centers. This lymphoid organogenesis is often seen in the synovium of patients with rheumatoid arthritis.
22
Granulomatous inflammation is a distinctive pattern of chronic inflammation characterized by aggregates of activated macrophages that assume an epithelioid appearance.
Granulomas can form under three setting
1- persistent T-cell responses to certain microbes (such as Mycobacterium tuberculosis, T. pallidum, or fungi). In which T-cell-derived cytokines are responsible for chronic macrophage activation.
2- Granulomas may also develop in response to relatively inert foreign bodies (e.g., suture or splinter), forming so-called foreign body granulomas.
3- Granulomas also develop in some immune –mediated inflammatory diseases like crohn disease ,which is one type of infalmmatory bowel disease .
23
Morphology
Epithelioid cells is activated macrophages in epithelial –like appearance .they have have pink, granular cytoplasm with indistinct cell boundaries.
multinucleated giant cells : Found in granulomas. They consist of a large mass of cytoplasm and many nuclei, and they derive from the fusion of 20 or more macrophages.
Microscopically
The granulomas are formed by the aggregates of epithelioid macrophages that surrounded by a collar lymphocytes also multinucleated gaint cells are found in granuloma. Older granuloma have a rim of fibroblast and connective tissue .
24
Systemic manifestation of inflammation
Inflammatory response remain confined to localized area .in some cases local injury can result in promenant systemic manifestations as inflammatory mediator released in circulation .the most prominent Systemic manifestation of inflammation
1- acute phase response
Increase concentration of plasma proteins , increase erythrocytes sedmentation rate ,fever .
2- alteration in white blood cells count
Leukosytosis : increase leukocytes number .
Leukopnia: decrease leukocytes number
3- lymph adenitis
Localized acute or chronic inflammation lead to reaction in the lymph nodes that drain the affected area .this will result in painful palpable nodes.
4- sepsis and septic shock
Is systemic manifestations of inflammation due to presence of toxins in the blood result in induction of histamine in circulation ending with vasodilatation leading to septic shock.
25