Female Genital System
Part II:Endometrium and Myometrium
– Infectious
– Non-neoplastic lesions– Neoplasms
NORMAL STRUCTURE
The myometrium is the thick muscular wall of the uterus which is covered internally by uterine mucosa called the endometrium.The endometrium is relatively resistant to infection ,partly because of it’s excellent natural drainage & partly because it is difficult for an infection to become established during reproductive life in a tissue which is regularly shed .
Acute Endometritis
most commonly after an abortion especially if fragments of the placenta or membrane are retained in the uterus .A variety of organisms including streptococci ,staph. ,E.coli & pseudomonas .
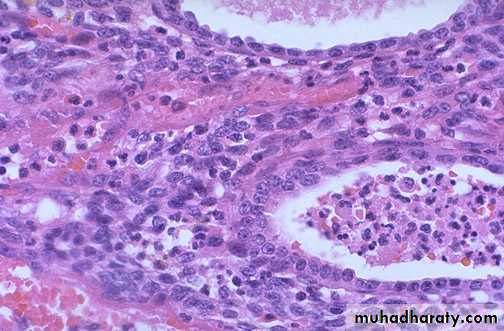
The inflamed endometrium is edematous & congested with polymorphnuclear cells infiltrate not only in stroma but also in the glands where small intra luminal abscesses are commonly seen.
There are scattered neutrophils in glands and stroma, indicative of acute endometritis
Chronic non-specific endometritis
may follow an acute endometritis but is more commonly chronic from the onset.chronic inflammatory cells infiltration with predominance of plasma cells ,some degree of fibroblastic & vascular proliferation may be present
Tuberculous Endometritis
It is nearly always secondary to tuberculous salpingitis .The disease is often accompanied by infertility
Continued menstrual shedding of the endometrium prevent the disease proceeding to the caseation
Tuberculous Endometritis
ENDOMETRIAL POLYPS
Definition : polypoid growth projecting into theuterine lumen
They are more common in the perimenopausal age group.
single or multiple, usually sessile and small but occasionally they are large and pedunculated.
They are essentially made up of mixture of endometrial glands and stroma.
The histologic pattern of the endometrial tissue in the polyp may resemble either functioning endometrium or hyperplastic endometrium of cystic hyperplasia type, the latter being more common.
Endometrial hyperplasia
Definition: exaggerated proliferation of glandular and stromal tissues.Presentation: prolonged, profuse and irregular uterine bleeding .
Etiology : abnormally high ,prolonged level of estrogenic stimulation with diminution or absence of progestational activity .
occurs most commonly around menopause or in association with persistent an ovulation in younger women
clinically significant because it is closely linked to endometrial carcinoma.
Causes:
Endometrial hyperplasia develops when estrogen and progesterone, are out of balance, and the endometrium is exposed to somewhat more estrogen than progesterone. This is called unopposed estrogen. Several things can cause this imbalance, including:• 1. High level of endogenous estrogen.
• - Obesity-Polycystic ovarian disease
(Stein Leventhal syndrome ).
-Functioning granulose cell tumors of the ovary.
-Excessive cortical function (cortical stromal hyperplasia ).
2. Exogenous estrogen
- Estrogen-only hormone replacement therapy (HRT)
Tamoxifen (Tamofen) given to treat breast cancer
Classification
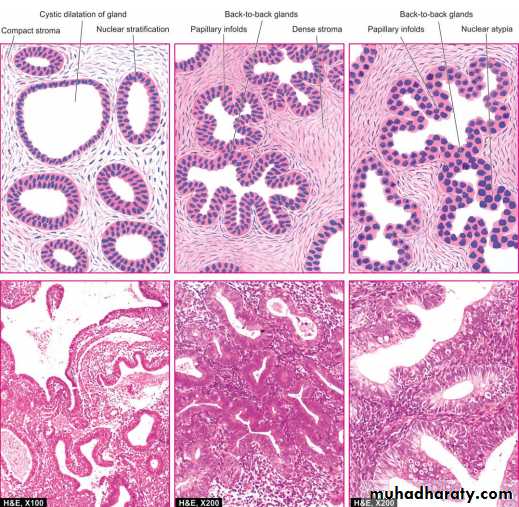
1. Simple hyperplasia without atypia (Cystic glandular hyperplasia).Simple patterns of increase in the gland-to-stroma ratio.
The glands show variation in size and shape and may be dilated but still stroma in between.
No cellular atypia.
rarely progress to adenocarcinoma ( 1% ).
2. Complex hyperplasia
• without atypia (Complex nonatypical hyperplasia). (3%)• with atypia (Complex atypical hyperplasia).
complex patterns of proliferating glands.
The glands are commonly back-toback and often have complex outlines due to branching structures.
Cells may or may not displaying nuclear atypia
- 23% to 48% of atypical hyperplasia can progress to carcinoma.
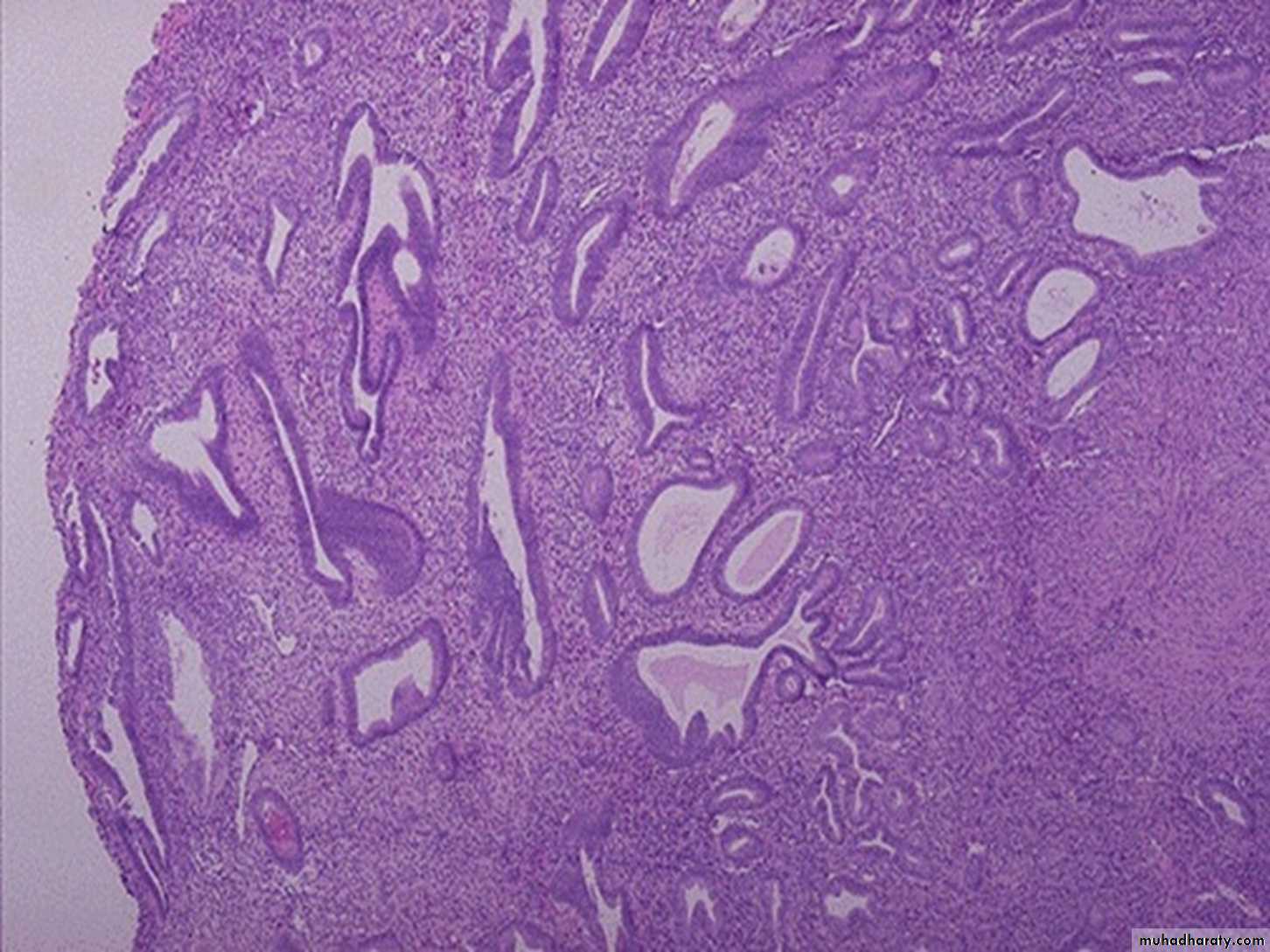
Simple hyperplasia without atypia
Complex hyperplasia with atypia
Why is endometrial hyperplasia concerning?Endometrial carcinoma
The most common invasive cancer of the female genital tract.ETIOLOGY A few factors associated with increased frequency of its development are as follows:
1. Chronic unopposed oestrogen excess
2. Obesity
3. Diabetes mellitus
4. Hypertension
5. Nulliparous state
6. Heredity.
Pathogenesis:
Clinicopathologic studies and molecular analyses support the classification of endometrial carcinoma into two broad categories referred to as type I and type IIType I (Endometrial) Carcinoma.
These are the most common type, accounting for approximately 80% of cases.
Most are well differentiated carcinoma.they typically arise in the setting of endometrial hyperplasia.
Type II Carcinoma.
These generally occur in women who are about 10 years older than those with type I carcinomasthey are poorly differentiated tumors and account for approximately 15% of cases of endometrial carcinoma.
They usually arise in the setting of endometrial atrophy
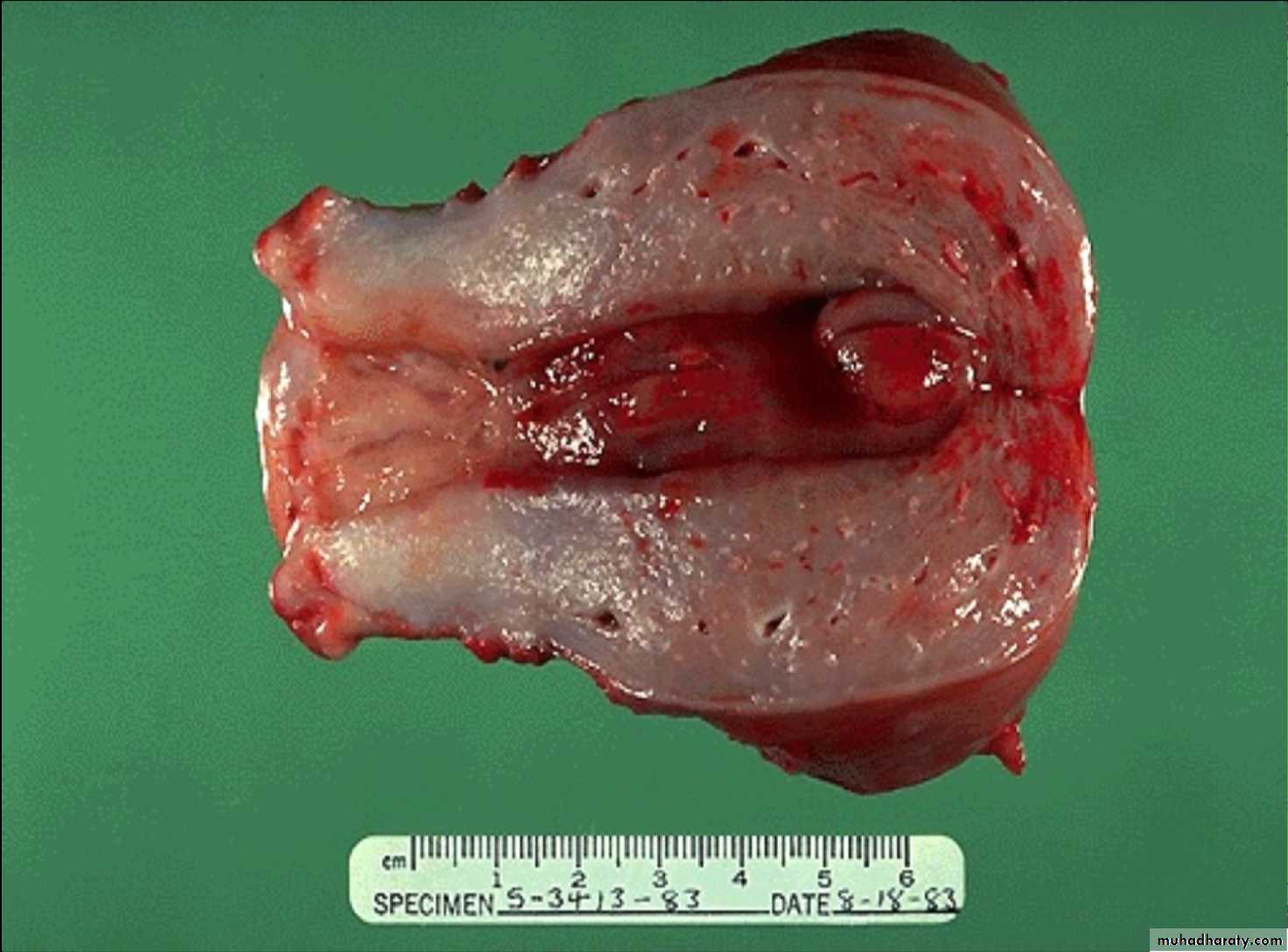
Uterus : well differentiated endometrial carcinoma
EndometriosisDefinition: presence of endometrial glands and stroma in abnormal locations outside the uterus.
The ectopic tissue occurs most commonly in the ovaries ,fallopian tubes ,pouch of Douglas , uterine ligaments ,recto vaginal septum & the bowel . Occasionally foci of endometriosis are encountered in laparotomy scar , at the umbilicus or in the skin .
Histogenesis of endometriosis
The following 3 theories are described:1. Transplantation or regurgitation theory is based on the
assumption that ectopic endometrial tissue is transplanted
from the uterus to an abnormal location by way of fallopian
tubes due to regurgitation of menstrual blood.
2. Metaplastic theory ,endometrium could arise directly from coelomic epithelium .
3. Vascular or lymphatic dissemination explains the development of endometrial tissue at extra pelvic sites by these routes.
MORPHOLOGIC FEATURES
Grossly, typically, appear as blue or brownish-black underneath the surface of the sites mentioned. Often, these foci are surrounded by fibrous tissue resulting in adherence to adjacent structures.The ovary is the most common site of endometriosis and shows numerous cysts varying in diameter filled with old dark brown blood form ‘chocolate cysts’ of the ovary.
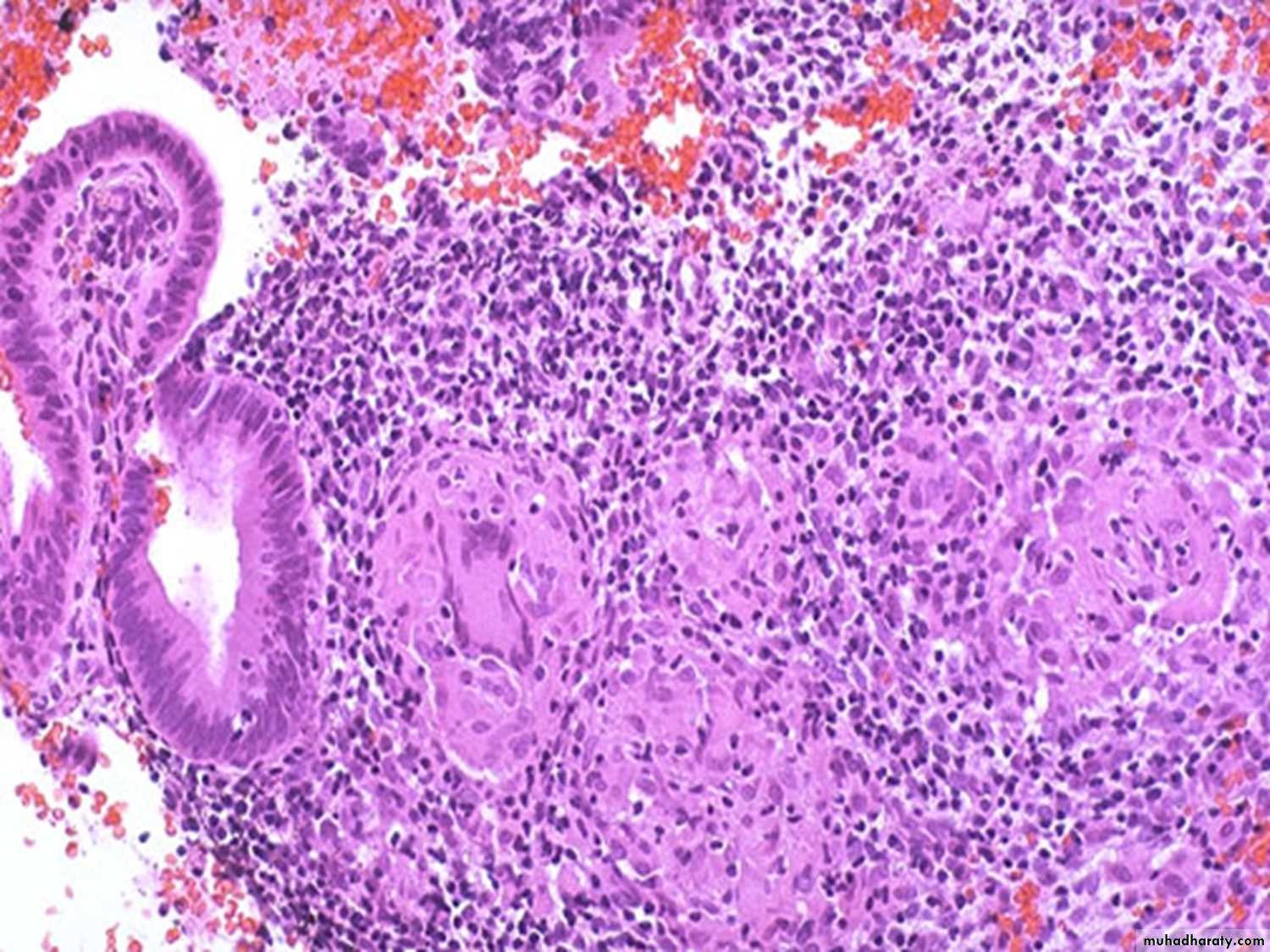
Histologically, the diagnosis is simple and rests on identification of foci of endometrial glands and stroma, old or new haemorrhages, haemosiderin-laden macrophages and surrounding zone of inflammation and fibrosis
Endometriosis : small cluster of endometrial glands and stroma with hemorrhage are seen at the left near the surface of the fallopian tube. The lumen of the tube is at the right.
Adenomyosis
Definition: the presence of endometrial tissue with in the myometrium , below the base of the endometrium.
The cause is unknown ,it occurs in approximately 15 to 20 % of the uteri. Adenomyosis causes expansion (enlargement ) of the uterine wall & may be visible on gross examination as numerous small cysts .
Microscopically
Irregular nests of endometrial stroma ,with or without glands ,are arranged with in the myometrium with myometrial muscle reaction around it separated from the basalis by at least 2 to 3 mm.Benign tumors
Leiomyomas (fibroid)Origin: from the smooth muscle cells of the myometrium.
usually multiple extremely common & vary in size from tiny seeding less than 1 cm in diameter to huge masses which fill the abdomen .
Site: within the wall i.e. intramural , immediately below the endometrium a submucosal ,or lie just beneath the peritoneum to form a subserosal tumor .
Histologically:
The neoplasm are formed of interlacing bundles of smooth muscle fibers arranged in twists or whorls ,contain densely packed spindle cells with elongated nuclei .In some tumors show variable degree of degenerative changes which are due to the neoplasm outgrowing its blood supply & thus fibrosis , hyaline change ,calcification ,patchy necrosis or fatty change are common .Red degeneration occurs particularly but not only in pregnancy. Uterine leiomyomas under hormonal control ,they occur almost entirely during the reproductive years ,enlarge during pregnancy & in women on oral contraceptives & tend to regress after the menopause .
Small tumors are asymptomatic but large tumors can cause pressure effect with pelvic discomfort & frequency of micturition ,dysmenorrhoea & infertility .
Malignant change is rare .
- Leiomyomas are usually estrogen-sensitive. Would you expect tumor size to vary throughout a women’s lifetime?
- Do leiomyomas commonly transform into malignant neoplasms (leiomyosarcomas)?
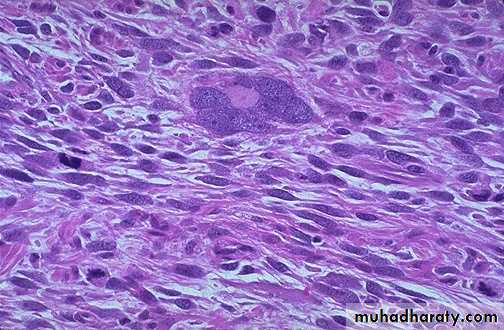
Malignant tumorsMyometrial leiomyosarcomas
rare ,arise from the myometrium .
They are less well demarcated in appearance than leiomyomas often show areas of haemorrhage or necrosis & are characterized histologically by their cellularity ,pleomorphism& mitotic activity ( i.e. 10 or more than 10 mitosis per 10 high power fields ).
leiomyosarcoma occur most commonly during the sixth decade & have a poor prognosis .