Geriatrics -
Adel Gassab MohammedMD, CABMS, MSc of Medicine Specialist Endocrinologist, Thi-Qar Specialized Diabetes, Endocrine and Metabolism Center, Lecturer Diabetes, Endocrine and Metabolism Division, Department of Medicine, College of Medicine, University of Thi-Qar,
Ageing – the most inevitable stage of human life
Geriatrics-Definition:
The care of aged peopleSub-specialty of internal medicine
Prevention and treatment of age related disabilities
Performed by Geriatricians
I will never be an old man.
To me, old age is always 15 years older than I amGeriatric age
Age group is not defined precisely
WHO defines old age as
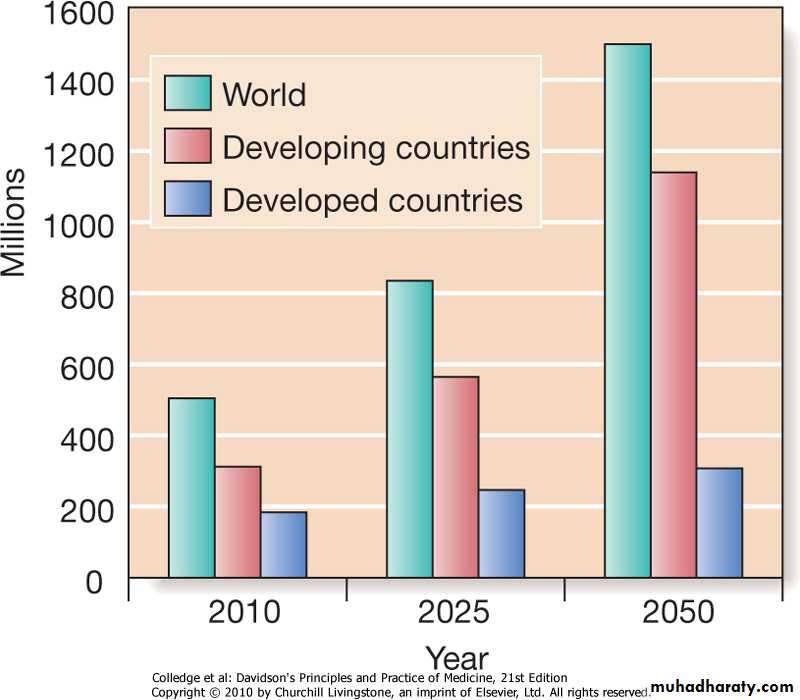
≥60 years ( developing countries) or ≥65 years (developed countries)Demography
The rate of population ageing is much faster in developing countryDownloaded from: StudentConsult (on 14 September 2012 09:44 AM)
© 2005 ElsevierGIANTS OF GERIATRICS (Isaacs 1970)
Presenting problems in geriatric medicineCharacteristics of presenting problems in old age
Many people (of all ages) accept ill health as a consequence of ageing and may tolerate symptoms for lengthy periods before seeking medical advice.
1. Late presentation
Infection may present with delirium and without clinical pointers to the organ system affected.
Stroke may present with falls rather than symptoms of focal weakness.
Myocardial infarction may present as weakness and fatigue, without the chest pain or dyspnoea.
Cognitive impairment may limit the patient’s ability to give a history of classical symptoms
2. Atypical presentation
Atypical presentations in frail elderly patients include:
‘failure to cope‘found on floor
confusion’ and
off feet.
3. Acute illness and changes in function
Presentations in older patients have a more diverse differential diagnosis because multiple pathology is so common. There are frequently a number of causes for any single problem, and adverse effects from medication often contribute• 4.Multiple pathology
Approach to presenting problems in old age
The approach to most presenting problems in old age can be summarised as follows:Obtain a collateral history. Find out the patient’s usual status (e.g. mobility, cognitive state) from a relative or carer.
Check all medication. Have there been any recent changes?
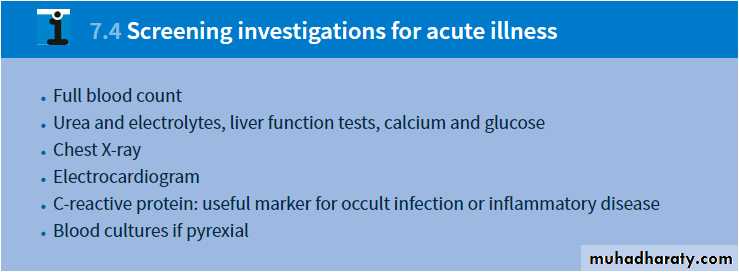
Search for and treat any acute illness.
Identify and reverse predisposing risk factors. These depend on the presenting problem.
HistorySlow down the pace.
Ensure the patient can hear.
Establish the speed of onset of the illness.
If the presentation is vague, carry out a systematic enquiry.
Obtain full details of:
-all drugs, especially any recent prescription changes
-past medical history, even from many years previously
usual function
-Can the patient walk normally?
-Has the patient noticed memory problems?
-Can the patient perform all household tasks?
Obtain a collateral history: confirm information with a relative or carer and the general practitioner, particularly if the patient is confused or communication is limited by deafness or speech disturbance.
Examinations
Thorough to identify all comorbidities.
Tailored to the patient’s stamina and ability to cooperate.
Include functional status:
-cognitive function
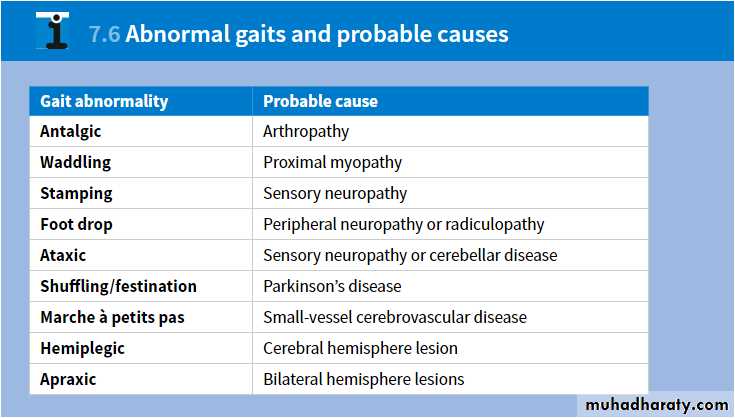
-gait and balance
-nutrition
-hearing and vision
Social assessment(Functional )
Home circumstancesLiving alone, with another or in a care home.
Activities of daily living (ADL)
Activity of daily living:
domestic ADL(DADL): shopping, cooking, housework
personal ADL(PADL): bathing, dressing, walking.
Informal help: relatives, friends, neighbours.
Formal social services: home help, meals on wheels.Frailty-Loss of an individuals ability to withstand minor stresses
Unintentional weight lossMuscle weakness
Exhaustion
Low physical activity
Slowed walking speed
A healthy person scores 0; a very frail person scores 5
Frailty scale:
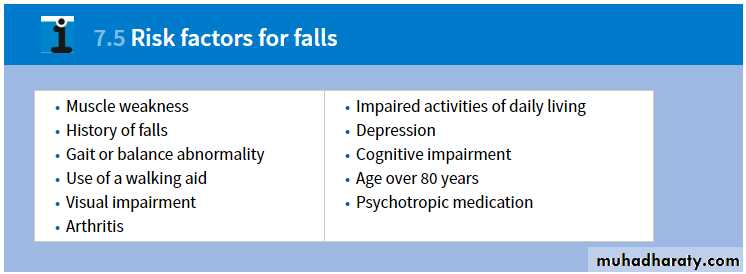
Falls
Around 30% of those over 65 years of age fall each year, this figure rising to more than 40% in those aged over 80. Although only 10–15% of falls result in serious injury, they are the cause of more than 90% of hip fractures in this age group, compounded by the rising prevalence of osteoporosisDizziness
Dizziness is very common, affecting at least 30% of those aged over 65 years in community surveys. Dizziness can be disabling in its own right and is also a risk factor for falls. Acute dizziness is relatively straightforward and common causes inclu
hypotension due to arrhythmia, myocardial infarction, gastrointestinal bleed or pulmonary embolism
onset of posterior fossa stroke
vestibular neuronitis.
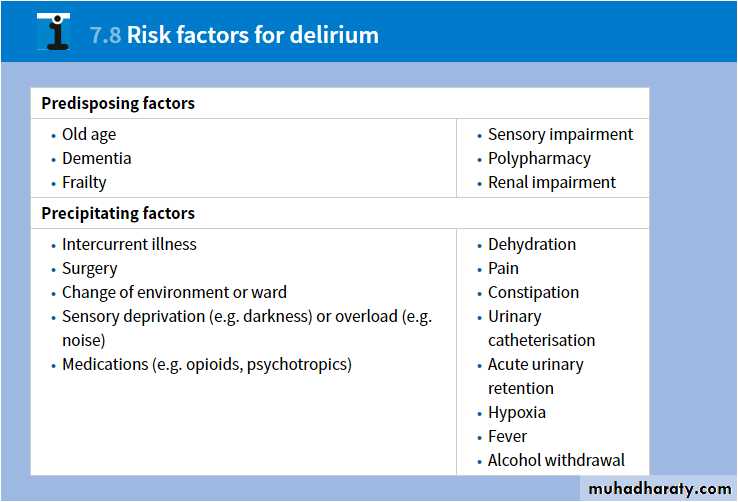
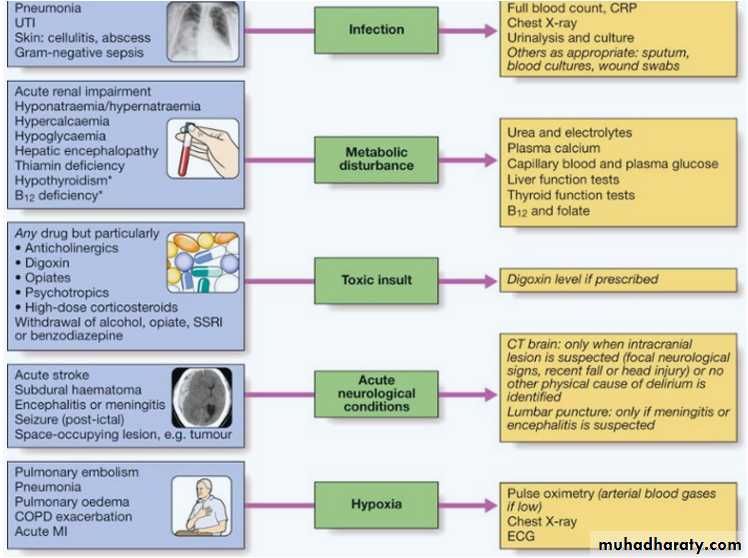
Delirium
Delirium is a syndrome of transient, reversible cognitive dysfunction. It is very common, affecting up to 30% of older hospital inpatients, either at admission or during their hospital stay.Common cause and investigations
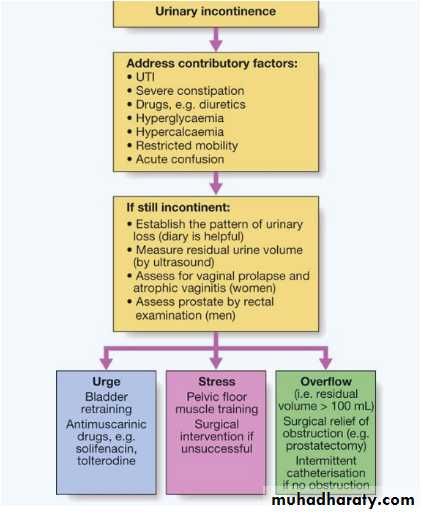
Urinary incontinence
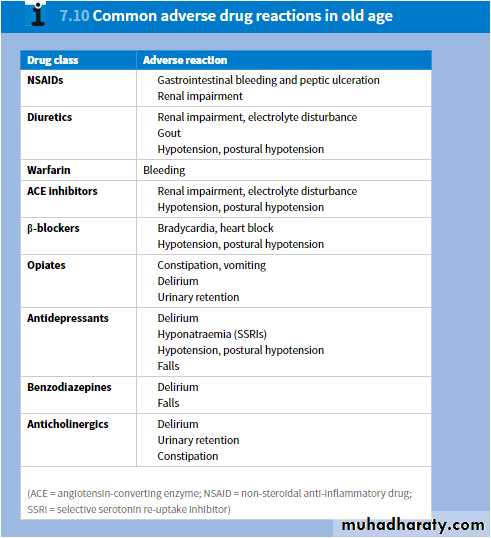
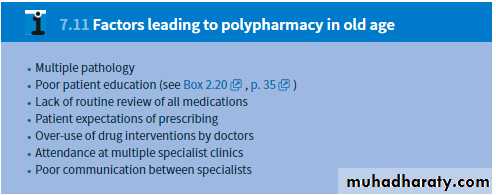
It occurs in all age groups but becomes more prevalent in old age, affecting about 15% of women and 10% of men aged over 65Drugs related Problems in geriatrics
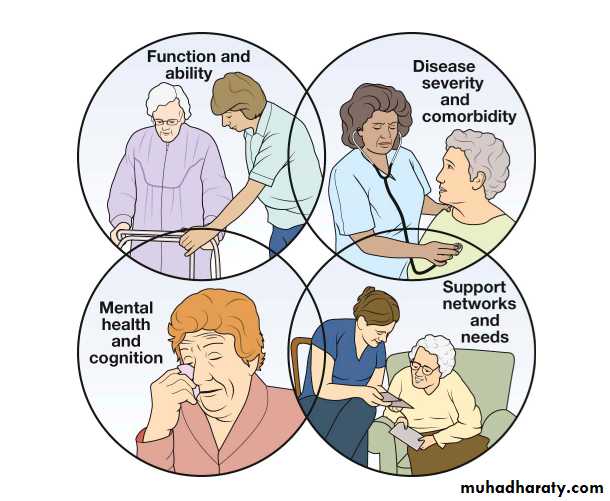
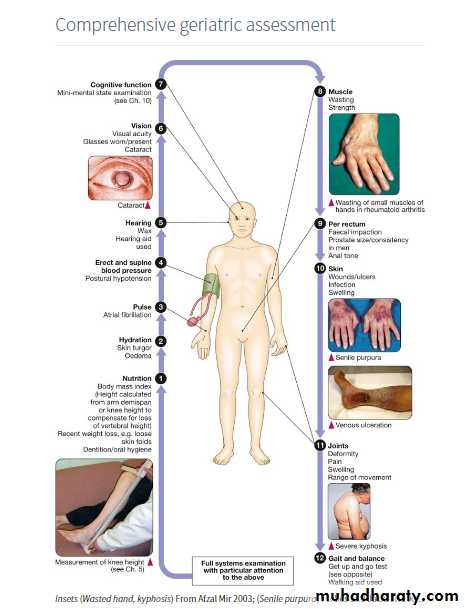
Adverse drug reactionsComprehensive Geriatric Assessment
• Multidisciplinary diagnostic and treatment process
• Medical, psychological and functional limitations• Coordinated plan to maximize health
• It differs from a standard medical evaluation by:
• Focus on elderly individual
• Emphasize on functional status & quality of life
• Multidisciplinary approach
CGA is defined as :
Patient selection criteria for CGA:
High risk elderly patient-frail or chronically ill
Medical co-morbidities, heart failure or cancer
Specific geriatric condition such as
dementia,
falls
functional disabilities
Psychosocial disorders such as
depression or
isolation
Major component of CGA
DOMAINS OF Comprehensive Geriatric AssessmentAdditional components :
Nutrition/weight changeUrinary continence
Sexual function
Vision/hearing
Dentition
Living situation
Spirituality
Subspecialties
Cardiogeriatricsgeriatric psychiatry
geriatric rehabilitation
geriatric rheumatology, etc.
• Orthogeriatric
• Geriatric Cardiothoracic Surgery• Geriatric urology, etc.
• Surgical
• Other
• Geriatric intensive-care unit
• Geriatric nursing
• Geriatric nutrition, etc.
Medicine
Rehabilitation
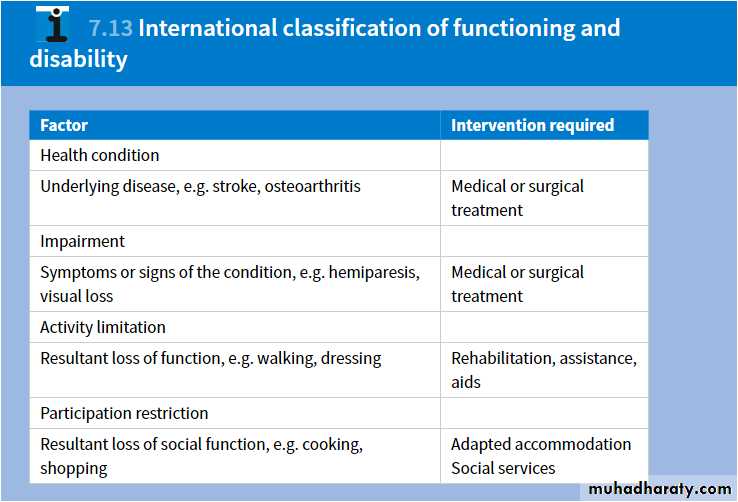
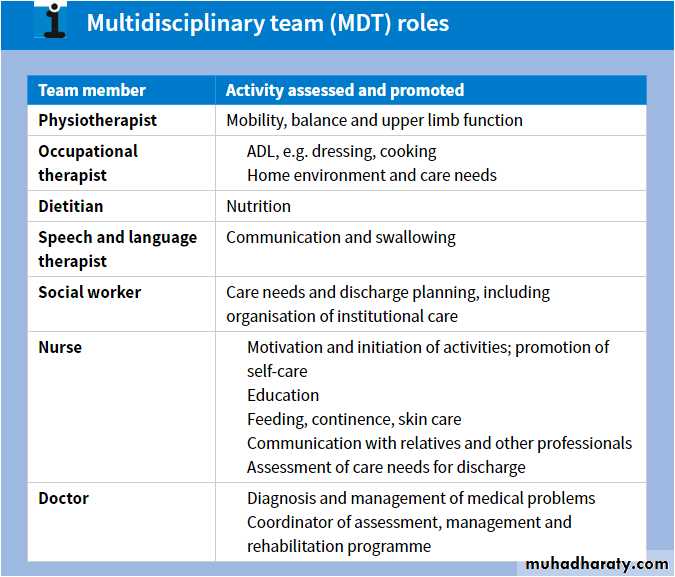
Rehabilitation aims to improve the ability of people of all ages to perform day-to-day activities, and to restore their physical, mental and social capabilities as far as possible.The rehabilitation process
Assessment.
Goal-setting.
Intervention.
Re-assessment.
Multidisciplinary team working
Research
The Hospital Elder Life Program(HELP)Designed to prevent delirium and functional decline in the hospitalized patient setting
40% incidence of delirium can be prevented
Replicated in over 63 hospitals across the world
Acute Geriatrics-based Ward (AGW)
AGW shortened the length of hospital stay andMay have cut down need for long-term institutional living
Geriatric-based versus general wards for older acute medical patients: a randomized comparison of outcomes and use of resources
Biology and genetics of ageing
Ageing can be defined as a progressive accumulation through life of random molecular defects that build up within tissues and cells.(Are) we (Are) able to slow or even stop the body's clock—at least for a little while ?
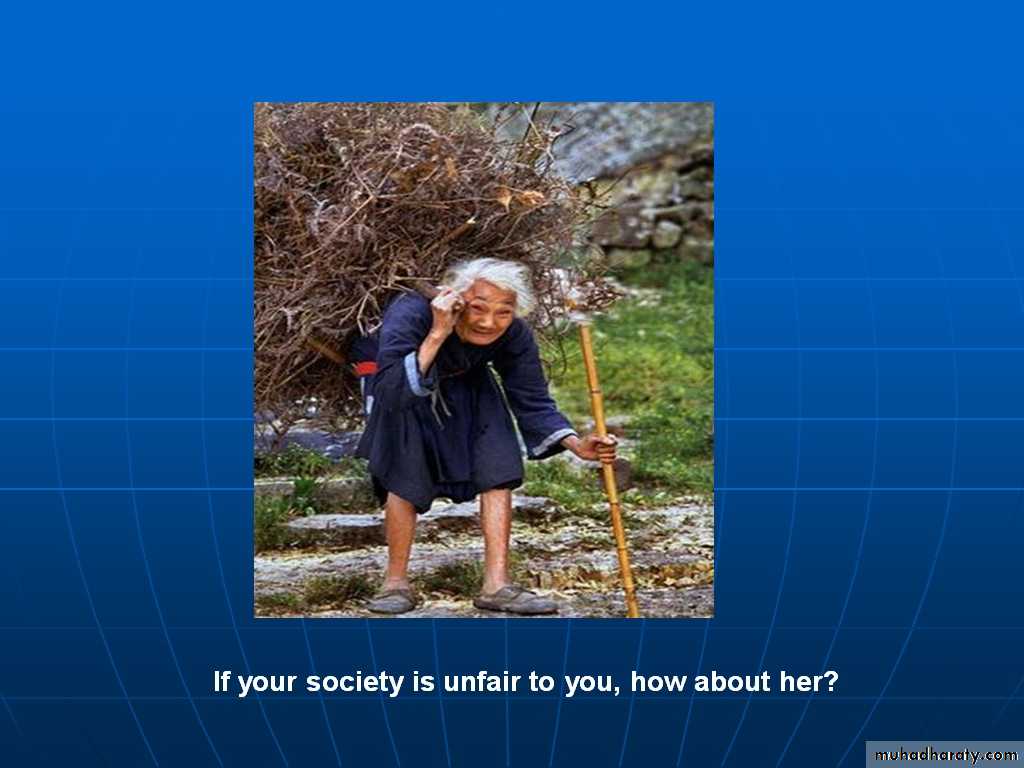
Please stand by him……………….
This frail elderly person needs your hands along with the stick