1
Thoracic Trauma
Introduction
Early deaths after thoracic trauma are caused by hypoxemia, hypovolaemia and
tamponade. The first steps in treating these patients should be to diagnose and treat
these problems as early as possible because they may be readily corrected. Young
patients have a large physiological reserve and serious injury may be overlooked until
this reserve is used up; then the situation is critical and may be irretrievable. The best
approach is to maintain a high index of suspicion and suspect the worst if life-
threatening conditions are to be anticipated and treated.
The basic principles of resuscitation are securing the airway and restoring the
circulating volume. Blood and secretions are removed from the oropharynx by suction.
If the patient is unable to maintain his or her airway then an oropharyngeal airway
followed by tracheal intubation (once a cervical spine injury is excluded) may be
necessary.
A thorough inspection of the chest wall includes noting the frequency and pattern of
breathing, external evidence of trauma and structural defects of the thorax.
Palpation will detect surgical emphysema, paradoxical movement and a stove-in chest.
Auscultation and percussion should reveal the existence of a pneumothorax (there is
decreased movement on the affected side with a hyperresonant percussion note, reduced
breath sounds in the axilla and shift of the trachea to the opposite side) which requires
emergency drainage.
Patients with injuries close to the trachea or esophagus should undergo endoscopy,
and patients with radiological clues suggestive of great vessels injury should undergo
arteriography.
Once the patient has been stabilized then radiographs of the chest should be taken
and further treatment decided on the basis of the patient’s condition and the
radiographic result.
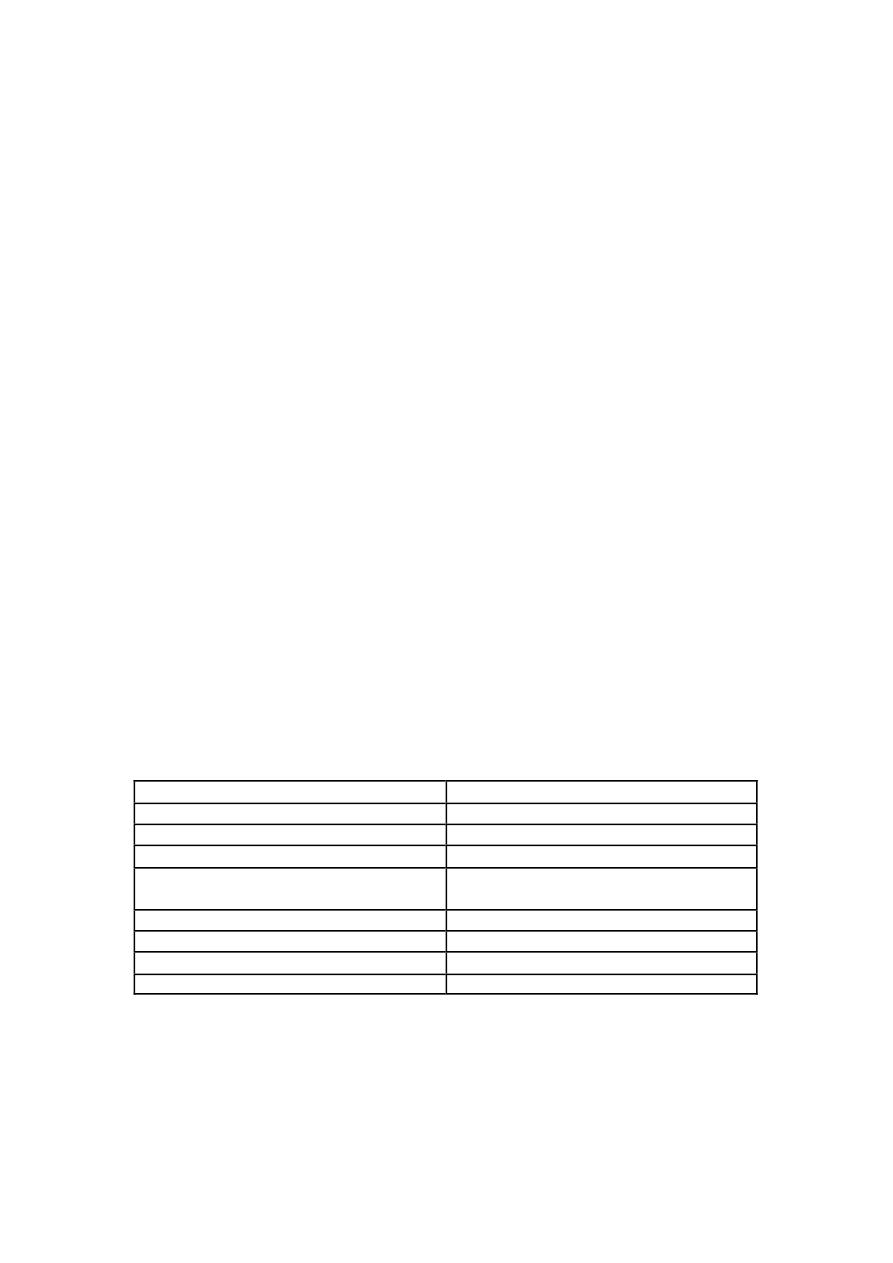
Table 1: Potentially acutely lethal injuries of the chest and their management
Tension pneumothorax
Tube thoracostomy
Massive intrathoracic hemorrhage
Tube thoracostomy, operative repair
Cardiac tamponade
Pericardocentesis, operative repair
Deceleration aortic injury
Operative repair
Massive flail chest with pulmonary
contusion
Intubation, pain control, fluid restriction
Upper and lower airway obstruction
Intubation, airway, bronchoscopy
Tracheobronchial rupture
Bronchoscopy, operative repair
Diaphragmatic rupture
Operative repair
Esophageal perforation
Operative repair
Blunt Trauma of the Chest

2
Rib Fractures
A simple rib fracture may be serious in elderly people or in those with chronic lung
disease who have little pulmonary reserve. Uncomplicated fractures require sufficient
analgesia to encourage a normal respiratory pattern and effective coughing. Oral
analgesia may suffice but intercostal nerve blockade with local anesthesia may be very
helpful. Chest strapping or bed rest is no longer advised and early ambulation with
vigorous physiotherapy (and oral antibiotics if necessary) is encouraged. A chest
radiograph is always taken to exclude an underlying pneumothorax. It is useful to
confirm the skeletal injuries but routine chest radiography may miss rib fractures.
However, once a pneumothorax and major skeletal injuries are excluded, the
management is the same — the local control of chest pain.
.
Flail chest
This occurs when several adjacent ribs (more than four) are fractured in two
places either on one side of the chest or either side of the sternum. The flail segment
moves paradoxically. The net result is poor oxygenation from injury to the
underlying lung parenchyma and paradoxical movement of the flail segment. The
underlying lung injury with loss of alveolar function may result in deoxygenated
blood passing into the systemic circulation. This creates a right-to-left shunt and
prevents full saturation of arterial blood. In the absence of any other injuries and if
the segment is small and not embarrassing respiration, the patient may be nursed on
a high-dependency unit with regular blood gas analysis and good analgesia until the
flail segment stabilizes. In the more severe case, endotracheal intubation is required
with positive pressure ventilation for up to 3 weeks, until the fractures become less
mobile.
Crystalloid solutions should be restricted to less than 1000 ml daily. If volume
expansion is needed, colloid solutions should be given.
Indications for Endotracheal intubation are:
• Respiratory rate of 30-40/min.
• Arterial PO2 of 60 torr or less (on face mask O2 of 60%).
• Arterial PCO2 of 50 torr or more.
• Presence of associated injuries.
• Pre-existing chronic lung disease.
• Depressed consciousness.
• Shallow respirations.
When the lung is healed, the patient may be extubated, even if flailing persists.
Thoracotomy with fracture fixation is occasionally appropriate if:
1) there is an underlying lung injury to be treated at the same time.
2) Intubated patients with no possibility being weaned from the ventilator because
of large unstable flail segment.
.
Fractures of the sternum

3
The injury is very painful even in the mild cases where only the external plate of the
sternum is fractured. However, there is a real risk of underlying myocardial damage
(myocardial contusion) and lung damage (contusion), the patient should be observed in
hospital with constant electrocardiogram (ECG) monitoring, analgesia and serial
cardiac enzymes.
The step deformity can be confirmed by lateral or oblique x-rays. Rupture of the
aorta and associated cervical spine injuries also need to be excluded. Most cases need
no specific treatment but paradoxical movement or instability of the chest may need
more active management.
Surgery is indicated for persistent pain and cosmesis.
.
Pleura.
If the visceral pleura is breached (most commonly by a rib fracture), pneumothorax
follows. Generation of positive pressure in the airways by coughing, straining, groaning
or positive pressure ventilation will result in tension pneumothorax. The pleural space
may also fill with blood as a result of injury anywhere in its vicinity. Remember that an
erect chest radiograph is the only sure way to confirm or exclude the diagnosis of
pneumothorax and hemothorax and should be obtained if at all possible.
*
Traumatic pneumothorax.
Blunt trauma to the chest wall may result in a lung laceration from a rib fracture. All
traumatic pneumothoraces require drainage through an underwater seal drain. If a
tension pneumothorax is suspected on clinical grounds, treatment is necessary before
radiographs can be taken. A chest tube or (if not available) wide bore needle introduced
into the affected hemithorax will release any air under tension and is life saving. A
second drain may be introduced basally to drain blood.
.
*
Traumatic hemothorax.
Drainage is essential because re-expansion of the lacerated lung compresses the torn
vessels and reduces further blood loss. Drainage will also allow the mediastinal
structures to return to the midline and relieve compression of the contralateral lung. If
left undrained, a dense fibrothorax will result with its morbid consequences i.e. trapped
lung syndrome, with the possibility of an added empyema; for that reason, clotted
hemothorax regarded as an indication for elective thoracotomy.
Lung parenchyma
After the chest wall, the lung is the most commonly injured intrathoracic organ,
manifestations of lung injury are pneumothorax, hemothorax, pulmonary contusion,
pulmonary hematoma, systemic air emboli, and ARDS.
The underlying lung is often injured in moderate-to-severe blunt thoracic trauma and
the area of contusion may be extensive. This usually resolves but lacerations with
persistent air leak may require exploration by thoracotomy. It is important to prevent
infection of the underlying lung by early mobilization with antibiotic cover, and to
prevent development of pulmonary edema by crystalloid fluid restriction.
Major airways
4
Injuries to major bronchi are infrequently seen as the patient rarely survives the insult
leading to major airway disruption. Injuries may be secondary to penetrating, blunt, or
iatrogenic trauma. There is usually a combination of surgical emphysema, hemoptysis,
pneumomediastinum and pneumothorax.
Symptoms usually develop immediately after penetrating trauma and there may be
some delay for up to one week in blunt trauma before atelectasis and pneumonia prompt
a detailed evaluation by bronchoscopy or bronchography.
Clinical clues suggestive of bronchial injury include:
• Unusually large and persistent air leak.
• Need for a second or third chest tube
• Incomplete expansion of a pneumothorax despite functioning chest tubes.
• Inability to keep lungs expanded.
• Refractory or recurrent lobar or whole lung atelectasis.
• CXR showing a pneumothorax with downward displacement of the hilum of
the lung.
Injury to the trachea requires considerable force and consequently less than a quarter
of patients survive to reach hospital. There is hoarseness, dyspnoea and surgical
emphysema.
Bronchoscopy or bronchography will be required to confirm the diagnosis. The exact
pattern of signs will depend on the site of the injury and whether or not the pleura has
been breached. The treatment is exploration and repair if possible.
The proximal one half to two thirds of the trachea is best approached via a low cervical
collar incision, whereas the distal third of the trachea, carina, and proximal right and
left mainstem bronchi should be approached through a right thoracotomy. Resection of
lung should be avoided.
Great Vesseles
The thoracic great vessels consist of the aorta and its major intrathoracic branches,
the pulmonary arteries and veins, the vena cavae, and the azygos vein. By far the most
lethal of these is the descending aortic injury , the site of the injury is the medial
descending aorta at the ligamentum arteriosum. Aortic transection is usually the result
of a major deceleration injury (road traffic accident or a fall from height) and the patient
often has other injuries.
In the last decade or so, the four most dramatic changes in the management of these
patients have been non operative management, delay of definitive treatment, use of
endovascular stenting for repair, and the increasing use of left sided bypass via
centrifugal pumps in the operating room. The open surgical approach is via a fourth
interspace left posterolateral thoracotomy.
.
Diaphragm
Blunt diaphragmatic rupture occurs mainly from high speed motor vehicle crashes.
This injury can be classified into three clinical phases, acute, latent, and obstructive
phases. The acute phase begins with the original trauma and ends with the apparent
recovery from other injuries. In the latent or interval phase symptoms are variable and
non specific and are suggestive of other disorders such as peptic ulcer, gall bladder
disorders, partial bowel obstruction and chronic obstructive pulmonary disease.
The obstructive phase may occur at any time.
5
Plain chest films are the initial screening tests of choice.
The surgical approach to repair acute diaphragmatic injury depends on mechanism of
injury, condition of the patient and the time of presentation.
In the acute phase the laparotomy approach is preferred, while thoracic approach is
preferred in the latent and obstructive phases because of possible adhesions between
herniated abdominal viscera and thoracic organs, however, thoracotomy approach
should be used for all right sided diaphragmatic defects regardless of the timing after
initial injury.
Management of blunt chest trauma (in general)
Most chest injuries where the heart is not injured are managed conservatively with
underwater seal drainage, oxygen and physiotherapy to help the patient to expectorate
while the underlying lung parenchyma heals. In about 10 per cent of cases a
thoracotomy is required.
The indications for tube thoracostomy:
It can be a life saving procedure and/or monitoring system for cases with continued
blood loss, and the general indications are:
1) Pneumothorax
2) Tension pneumothorax
3) Hemothorax
4) Penetrating wound below the nipples and without hemopneumothorax, for
whom an exploratory laparatomy is planned.
5) ARDS patients on ventilator with high PEEP (bilateral).
6) Extensive subcutaneous emphysema (bilateral).
The indications for thoracotomy following blunt thoracic trauma are the
following:
A) urgent
• For those rapidly deteriorating because of exsanguinating hemorrhage or from
tamponade.
B) emergent
1) drainage of more than 1500 ml of blood during time of chest tube insertion.
2) continued brisk bleeding (>100 mI/15 minutes).
3) continued bleeding of >200 ml/hour for 3 or more hours.
4) rupture of the bronchus, aorta, esophagus.
5) cardiac tamponade.
C) elective
1) Traumatic diaphragmatic hernia.
2) Traumatic false aneurysm.
3) Delayed post-traumatic squelae of penetrating cardiac injuries (valvular and
septal defects).
4) Stenosis of trachea or main stem bronchus.
5) Evacuation of clotted hemothorax.
Penetrating Injury of the Chest

6
In some aspects, penetrating thoracic injury is simpler to be dealt with than blunt
trauma because the wound is visible and the structures at risk can be quickly assessed.
A defect in the chest wall through to the pleura is a ‘sucking wound’. The underlying
lung collapses and air moves in and out of the thorax with each breath. Emergency
treatment involves sealing the wound and intercostal drainage. Definitive treatment
may then follow. It is important to establish the path or track of bullet and stab wounds
in the chest as there may be damage to the heart, great vessels, and the diaphragm and
abdominal viscera in addition to the lung injury.
Bullet wounds create a cavitating defect in the tissues that they pass through. The
tissue damage may be very extensive with high-velocity missiles, and entry and exit
wounds should be noted. Lung tissue is more compliant than the bone and muscles that
comprise the limbs, and enthusiastic resection along the track can be avoided in most
cases. Tetanus prophylaxis and high-dose antibiotics (to cover anaerobic organisms)
should be given. Bullets lodged in the lung do not require removal if they are not
causing any problems.
.
Penetrating wounds of the heart
This is usually the result of a stabbing or shooting incident, but can also be
iatrogenic from central line placement, cardiac catheterization and endomyocardial
biopsy. Cardiac tamponade may occur rapidly even with small amounts of blood in the
pericardium and the condition is recognized by low blood pressure, tachycardia, a high
central venous pressure, pulsus paradoxus and faint heart sound.
Emergency treatment includes aspiration of the pericardium by advancing a wide-
bore needle to the left of the xiphisternum towards the heart. This may hold the situation
until surgical repair is performed.
Complications of thoracic trauma
Pulmonary
1. Atelectasis
2. Acute respiratory distress syndrome
3. Pneumonia
4. Infarction
5. Lung abscess
6. Arteriovenous fistula
7. Bronchial stenosis
8. Tracheoesophageal fistula
Pleural space
1. Empyema
2. Bronchopleural fistula
3. Organized hemothorax
4. Chylothorax
5. Fibrothorax
6. Diaphragmatic hernias
Vascular
1. Thromboembolism
2. Air embolism
3. Pseudoaneurysm
4. Great vessel fistula

7
Chest wall
1. Hernias
2. Persistent pain
Mediastinum
1. Mediastinitis
2. pericarditis
Esophageal rupture
. Esophageal perforation is unusual but catastrophic event. Mortality rate is still high
and can reach up to 20%.
Etiology
1) Iatrogenic (51%)
• instrumentation (esophagoscope, pneumatic dilation, bougienage, NG
tube, ET tube and sclerotherapy).
• operative injury (mediastinoscopy, thyroidectomy, leiomyoma
enucleation, gastric vagotomy…..etc).
2) trauma (20%) penetrating ,blunt, and blast effect.
3) spontaneous (barogenic) rupture 15% follow sudden and drastic increase in intra
abdominal pressure, most commonly following vomiting.
4) Rare causes e.g. tumor, Barrett's ulcer, and viral infection.
Clinical features
Depend on cause, location, and duration since perforation: Pain, dyspnoea,
dysphagia, and fever are found in different combinations.
Mackler`s triad: it is the combination of vomiting, lower thoracic pain, and
subcutaneous emphysema which occur during spontaneous rupture.
Diagnosis
Should be suspected in any case with history of instrumentation and suspicious
symptoms.
• Plain CXR
• Contrast studies: it is the standard measure to document the perforation and
it's location.
• Esophagogastrodoudenoscopy and CT scan as adjunct measures.
Therapy
Principles are:
1) Debridement of infected and necrotic tissues.
2) Elimination of distal obstruction(if present).
3) Secure closure of the perforation( re-enforced primary repair of perforation).
4) Drainage.
5) Establishment of enteral access.
6) Antibiotic therapy.
Treatment options are:

8
A) Non operative therapy, when the leak is minimal and there are no signs of sepsis:
by keeping the patient fasting, broad spectrum AB for 14 days, drainage of pleural
effusions, and total parenteral nutrition.
If the patient condition didn't improve after 24 h, surgical intervention should be
strongly considered.
B) Operative therapy
Absolute criteria for operation are:
1) pneumothorax
2) pneumoperitonium
3) extensive mediastinal emphysema
4) sepsis
5) shock
6) respiratory failure
7) failure of non operative therapy (abscess, empyema)
aspirated foreign bodies
This is a regrettably common occurrence in small children and is often marked by a
choking incident which then apparently passes. Surprisingly large objects can be
inhaled and become lodged in the wider caliber and more vertically placed right main
bronchus. If not removed, an obstructive emphysema may result but, if there is total
occlusion of the bronchus, the air distally will be absorbed and the secretions may
become infected.
There are three possible presentations:
1).asymptomatic
2) wheezing (from airway narrowing) with a persistent cough and signs of obstructive
emphysema.
3) pyrexia with a productive cough from pulmonary suppuration.
A chest radiograph is vital as the object may be radiopaque, or to visualize the
possible complications caused by the foreign body e.g. atelectasis, hyperinflation…etc.
Often it is not radio-opaque or is obscured by the cardiac shadow or the inflammatory
response.
Bronchoscopy is required by an experienced operator with an experienced anesthetist
to administer the anesthetic. The procedure may be very difficult if there is a severe
inflammatory reaction. The rigid bronchoscope is best for retrieving inhaled foreign
bodies. Failure to remove the object may necessitate a bronchotomy through a formal
thoracotomy. If the object has caused chronic lung damage it may be necessary to
remove the affected lobe.
Foreign bodies can be classified into organic (like seeds, tiny food particles….etc.)
which require medical stabilization before bronchoscopy can be done safely, and non
organic foreign bodies (usually radiopaque metallic objects).
Clinical suspicion of foreign body inhalation (in the absence of suggestive history)
should be aroused after failure of medical treatment after one week of admission and
optimum treatment of chest infection.
