1
Seizures in Childhood
Febrile seizure
It occurs between the age of 6 and 60 mo with a temperature of 38°C (100.4°F)
or higher, that are not the result of central nervous system infection or any
metabolic imbalance, and no history of prior afebrile seizures.
-A simple febrile seizure is a primary generalized, usually tonic–clonic,
attack associated with fever, lasting for a maximum of 15 min, and not
recurrent within a 24-hr period.
-A complex febrile seizure is more prolonged (>15 min), is focal, and/or
reoccurs within 24 hr.
-Febrile status epilepticus is a febrile seizure lasting longer than 30 min.
-Some use the term simple febrile seizure plus for those with recurrent febrile
seizures within 24 hr.
-Simple febrile seizures do not have an increased risk of mortality.
-Complex febrile seizures may have an approximately 2-fold long-term
increase in mortality, as compared to the general population, over the
subsequent 2 yr, probably secondary to coexisting pathology.
-There are no long-term adverse effects of having 1 or more simple febrile
seizures.
Although approximately 15% of children with epilepsy have had febrile
seizures, only 2-7% of children who experience febrile seizures proceed to
develop epilepsy later in life.
Risk factors for recurrence of febrile seizures
Major: (Age <1 year, Duration of fever <24 hr, and Fever 38-39C)
Minor: (Family history of febrile seizures, Family history of epilepsy,
Complex febrile seizure, Day care, Male gender, and Lower serum sodium
at time of presentation).
• No risk factors: recurrence risk 12%.
• 1 risk factor: recurrence risk 25-50%.
• 2 risk factors: recurrence risk 50-59%.
• 3 or more risk factors: recurrence risk 73-100%.
Risk factors for epilepsy:
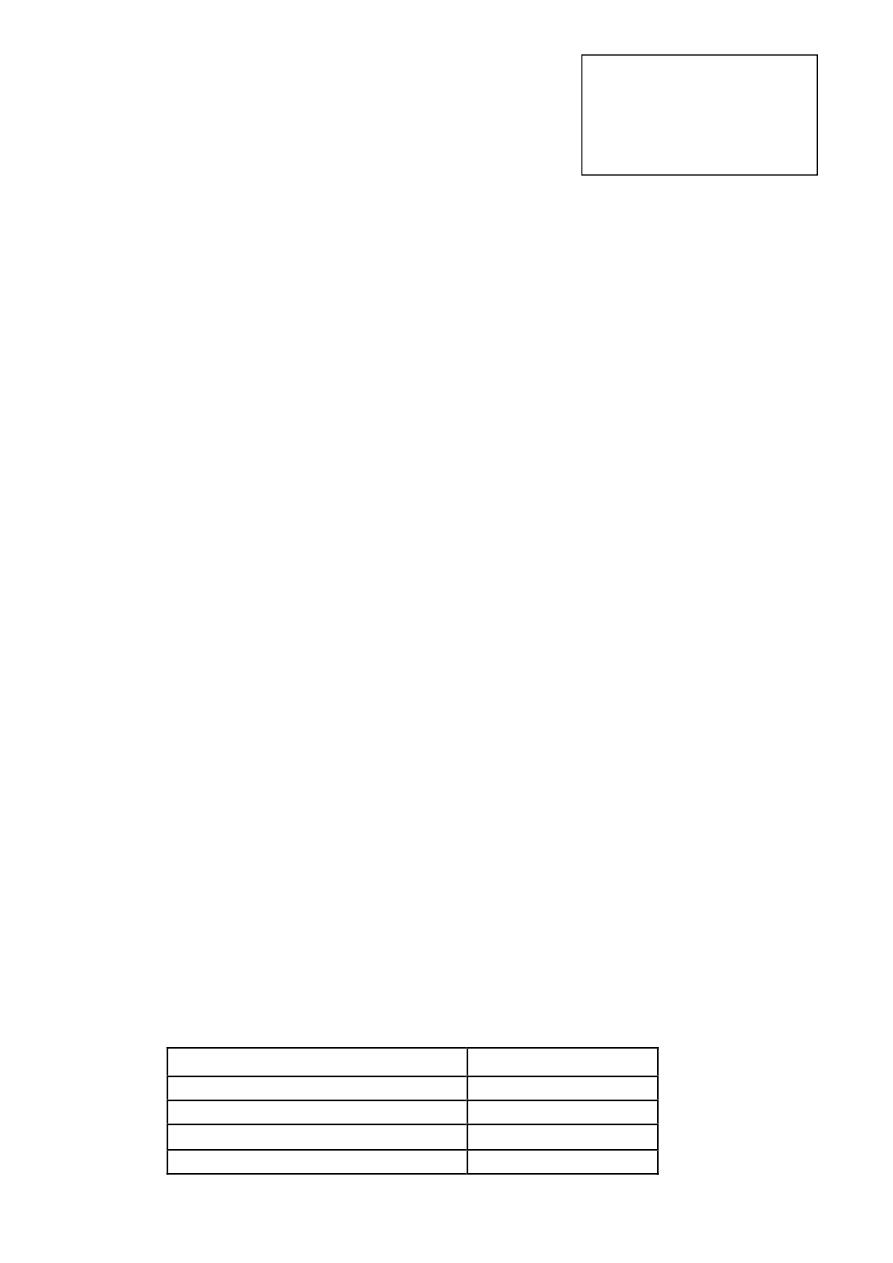
Risk Factor
Risk for Epilepsy
Simple febrile seizure
1%
Recurrent febrile seizures
4%
Complex febrile seizure
6%
Fever <1 hour before febrile seizure
11%
Pediatric neurology lecture
By Dr. Russul Feihan
Assist professor
Babylon medical college
Part 2

2
Family history of epilepsy
18%
Focal complex febrile seizure
29%
Neurodevelopmental abnormalities
33%
GENETIC FACTORS
The genetic contribution to the incidence of febrile seizures is manifested
by a positive family history for febrile seizures in many patients.
In some families, the disorder is inherited as an autosomal dominant trait.
However, in most cases the disorder appears to be polygenic.
EVALUATION:
Each child who presents with a febrile seizure requires a detailed history and a
thorough general and neurologic examination
.
Investigations:
I.
Lumbar puncture (LP):
1- Should be performed for all infants younger than 6 mo of age who
present with fever and seizure, or if the child is ill appearing.
2- At any age if there are clinical signs or symptoms of concern.
3- It is an option in a child 6-12 mo of age who is deficient in
Haemophilus influenzae type b and Streptococcus pneumoniae
immunizations or for whom immunization status is unknown.
4- It is an option in children who have been pretreated with antibiotics.
II. EEG:
If an EEG is indicated, it is delayed after more than 2 wk have passed.
A- It should be restricted to cases in which epilepsy is highly suspected,
and, generally, it should be used to detect the type of epilepsy rather than
to predict its occurrence.
B- If the patient does not recover immediately from a seizure, then an EEG
can help distinguish between ongoing seizure activity and a prolonged
postictal period.
C- It can also be helpful in patients who present with febrile status
epilepticus
III. Blood studies: (serum electrolytes, Ca, PO4, Mg, and CBC)
are not
routinely recommended with a first simple febrile seizure
.
IV. Blood glucose should be determined only in children with prolonged
postictal obtundation or those with poor oral intake.
V.
CT or MRI: is indicated if the child is neurologically abnormal and in
patients with febrile status epilepticus.
3
Treatment:
1- Parent's emotional support.
2- Antiepileptic therapy is not recommended for children with one or more
simple febrile seizures.
3- If the seizure lasts for >5 min, then acute treatment with diazepam,
lorazepam, or midazolam is needed.
4- Rectal diazepam is given at the time of recurrence of febrile seizure
lasting >5 min. alternatively, buccal or intranasal midazolam may be
used and is often preferred by parents.
5- Intermittent oral diazepam can be given during febrile illnesses
(0.3 mg/kg every 8 hr). Intermittent oral nitrazepam, clobazam, and
clonazepam (0.1 mg/kg/day) have also been used.
6- Antipyretics do not reduce the risk of having a recurrent febrile
seizure, probably because the seizure often occurs as the temperature is
rising or falling.
7- Iron deficiency has been shown to be associated with an increased risk
of febrile seizures, and thus screening for that problem and treating it.
Status Epilepticus
Continuous seizure activity or recurrent seizure activity without regaining of
consciousness lasting for >30 min.
Impending Status epilepticus: seizures between 5 and 30 min.
The most common type is convulsive status epilepticus (generalized tonic,
clonic, or tonic–clonic), but other types do occur, including nonconvulsive
status (complex partial, absence), myoclonic status, epilepsia partialis
continua, and neonatal status epilepticus.
Nonconvulsive status epilepticus: manifests as a confusional state, dementia,
hyperactivity with behavioral problems, fluctuating impairment of
consciousness, hallucinations, and psychotic symptoms.
Refractory status epilepticus: failure to respond to therapy, usually with at
least 2 medications.
Etiology:
• New-onset epilepsy of any type.
• Drug intoxication (tricyclic antidepressants).
• Drug and alcohol abuse.
• AEDs withdrawal or overdose.
• Hypoglycemia, hypocalcemia, hyponatremia, hypomagnesemia.
• Acute head trauma.
• Encephalitis, meningitis, ischemic stroke, intracranial hemorrhage.
• Pyridoxine, and folinic acid dependency.
• Inborn errors of metabolism (nonketotic hyperglycinemia) in neonates.

4
• Hypertensive encephalopathy, renal or hepatic encephalopathy.
• Brain tumors, brain malformations, and neurodegenerative disorders.
Management
v
Continuous attention to ABC (with continuous monitoring of vital
signs including ECG).
v
Determination and management of the underlying etiology (e.g.,
hypoglycemia).
v
Laboratory studies including glucose, sodium, calcium, or other
electrolytes, are ordered as routine practice.
v
Blood and spinal fluid cultures, toxic screens, and tests for inborn
errors of metabolism are often needed.
v
AED levels need to be determined in known epileptic children
already taking these drugs.
v
EEG is show several stages that consist of initial distinct
electrographic seizures (stage I) followed by waxing and waning
electrographic seizures (stage II), continuous electrographic
seizures (stage III; many patients start with this directly),
continuous ictal discharges punctuated by flat periods (stage IV),
and periodic epileptiform discharges on flat background (stage V).
The last 2 stages are often associated with subtle clinical
manifestations and with a lower chance of response to
medications
.
Physical and neurological examination: for any evidence of trauma,
papillodema., bulging anterior fontanel, lateralizing neurological signs
suggesting ↑ I.C.P., manifestation of sepsis or meningitis, retinal hemorrhage,
acidotic breathing and dehydration. evidence of metabolic diseases,
constriction or dilatation of pupils.
Drugs: should be given by intra venous route.
Phenytoin must not be given in glucose solution, because it is precipitated in it.
Diazepam : given directly in the vein (0.1-0.3 mg/kg ) with maximum dose of
10 mg at a rate not more than ( 2 mg / min )for max. of 3 doses. It can be used
rectally (0.3-0.5 mg/kg ) diluted in 3ml 0.9% NaCl. The drug has short half-life
and may cause hypotension and respiratory depression especially if given with
barbiturate. Its therapeutic serum level occurs within 5-10 min.
Lorazepam: is equally effective with long half- life and less respiratory
depression. Its sublingual, I.V and rectal dose ( 0.05 -0.1 mg/kg ).
If intravenous access is not available, buccal midazolam or intranasal
lorazepam can be used. In infants, a trial of pyridoxine is often warranted.
Fosphenytoin: The loading dose is usually 15-20 PE/kg. The maintenance dose
can be started right away or, more commonly, in 6 hr. The rate of infusion of
fosphenytoin and phenytoin must be not more than 0.5-1 mg/kg/min.

5
The subsequent medication is often phenobarbital, the loading dose in
neonates is usually 20 mg/kg, but in infants and children the dose is 5-
10 mg/kg .The dose is repeated if there is no adequate response.
Intravenous valproate as a third-line medication.
ü
After the second or third medication is given, and sometimes before that,
the patient might need to be intubated.
ü
All patients with, even the ones who respond, need to be admitted to the
ICU for completion of therapy and monitoring.
ü
For refractory cases, an intravenous bolus of midazolam, propofol,
pentobarbital, or thiopental is usually initially used.
For non-convulsive status epilepticus: trials of oral or sometimes parenteral
AEDs without resorting to barbiturate coma or overmedication that could result
in respiratory compromise.
Prolonged non-convulsive complex partial status epilepticus can last for as
much as 4-12 weeks, with patients manifesting psychotic symptoms and
confusional states. These cases can be resistant to therapy. Some of these cases
appear to improve with the use of steroids or IVIG .
Potential therapies under study for convulsive status epilepticus include
induction of acidosis (e.g., by hypercapnia), and ketogenic diet.
Conditions that mimic seizures
These conditions share features with epilepsy and may be associated with
altered level of consciousness, tonic or clonic movement or cyanosis.
Benign paroxysmal vertigo: Typically develops in toddlers. It remits by
5 years of age. The attack develops suddenly associated with ataxia causing the
child to fall or refuse to walk or sit. Horizontal nystagmus may occur during
the attack. The child appears frightened and pale, nausea and vomiting may be
prominent, consciousness and verbalization aren’t disturbed. The attack last
(secs – mins) and the frequency vary from daily to monthly; vertigo is
verbalized by older child. Those children are susceptible to motion sickness
and migraine, negative neurological exam. MRI and EEG are normal, but
caloric testing, can show abnormal vestibular function.
Treatment: Diphenhydramine (5 mg / Kg / 24 h) → max 300 mg /day (orally,
I.M., I. V., rectally)
Night terrors : are common especially in boys between (5-7) y. they occur in
(1- 3%) of children and usually short – lived, it start suddenly usually between
midnight and 2:00 A.M when the child screams and appears frightened with
dilated pupils, tachycardia and hyper ventilation ,there is little or no
verbalization and is unaware of surrounding ,sleep follows in few min and
there is total amnesia the following morning. 1/3 of them experience
somnambulism.
Treatment: Short course of diazepam may be considered for protracted cases.
6
Breath – Holding spells : there are 2 major types:-
Cyanotic spells : It is the more common type. Upsetting or scolding an infant
provokes it. The attack preceded by brief shrill cry followed by forced
expiration and apnea and rapid onset of generalized cyanosis and loss of
consciousness which may be associated with repeated generalized clonic jerks ,
opisthotonus and bradycardia. Interictal EEG is normal. It is rare before 6m of
age peaked at 2y and abate by 5y of age.
Treatment: Support and reassurance of the parents. Placing the child safely in
bed and refusing to cuddle, play or hold the child when recovery is complete
because that will reinforce the child behavior.
Pallid spells: It is typically initiated by a painful experience or sudden startle,
the child stop breathing, rapidly loss consciousness , becomes pale and hypo
tonic and may have tonic seizure , normal inter ictal EEG. The attack can be
induced spontaneously by ocular compression that produce oculo cardiac reflex
, but don’t attempts to do that.
Treatment : Conservative, trial of oral atropine sulfate 0.01 mg /kg/day in
divided doses with maximum dose of 0.4 mg which will increase the H.R by
blocking the vagus nerve.( in refractory cases).
Vagal syncope: Vasovagal (neurocardiogenic) is usually triggered by
dehydration, heat, standing for a long time without movement. There is
initially pallor and sweating followed by blurring of vision, dizziness, nausea,
and then gradual collapse with loss of consciousness. Urinary incontinence in
10% and a brief period of convulsive jerks occur in 50%. Postictal confusion
can also occur. Abdominal pain, a common aura in temporal lobe epilepsy,
occurs in vasovagal syncope. Most children with vasovagal syncope have an
affected first-degree relative. EEG is normal and the tilt test has been used for
diagnostic purposes.
Management:
• Avoidance of precipitating factors (maintenance of hydration, avoidance
of standing still, rising slowly from sitting, first aid measures, raise legs,
positioning).
• Treatment of any accompanying or underlying medical conditions
(anemia, adrenal insufficiency, cardiac, etc.).
• β-blockers or flurohydrocortisone therapy may be needed .
Pseudo seizures :- Typically occur between (10 -18) y of age, more frequent
in females . It occurs in many patients with past history of epilepsy . No
cyanosis, normal reaction of pupils to light , no loss of sphincter control , no
tongue biting . The patients are likely to have neurotic personality , no effect
for anticonvulsant . EEG shows excess muscle artifact but normal back ground.
