FRACTURES OF THE FEMORAL NECK
Dr. Jamal Al-Saidy
M.B.Ch.B. .F.I.C.M.S
The femoral neck is the commonest site of fractures in the elderly,(age-related
osteoporosis).
The risk factors include bone-losing or bone-weakening disorders such as
osteomalacia, diabetes stroke (disuse), alcoholism and chronic debilitating
disease. In addition, old people often have weak muscles and poor balance
resulting in an increased tendency to fall.
Femoral neck fractures are also much less common in black (Negroid) peoples
than in whites and Asians.
OA is protective.
Mechanism of injury
The fracture usually results from a simple fall; however, in very osteoporotic
people, less force is required perhaps no more than catching a toe in the carpet
and twisting the hip into external rotation.
In younger individuals, the usual cause is a fall from a height or a blow sustained in
a road accident. These patients often have multiple injuries and in 20 per cent
there is an associated fracture of the femoral shaft.
Occasionally, stress fractures of the femoral neck occur in runners or military
personnel.
Pathological anatomy and classification
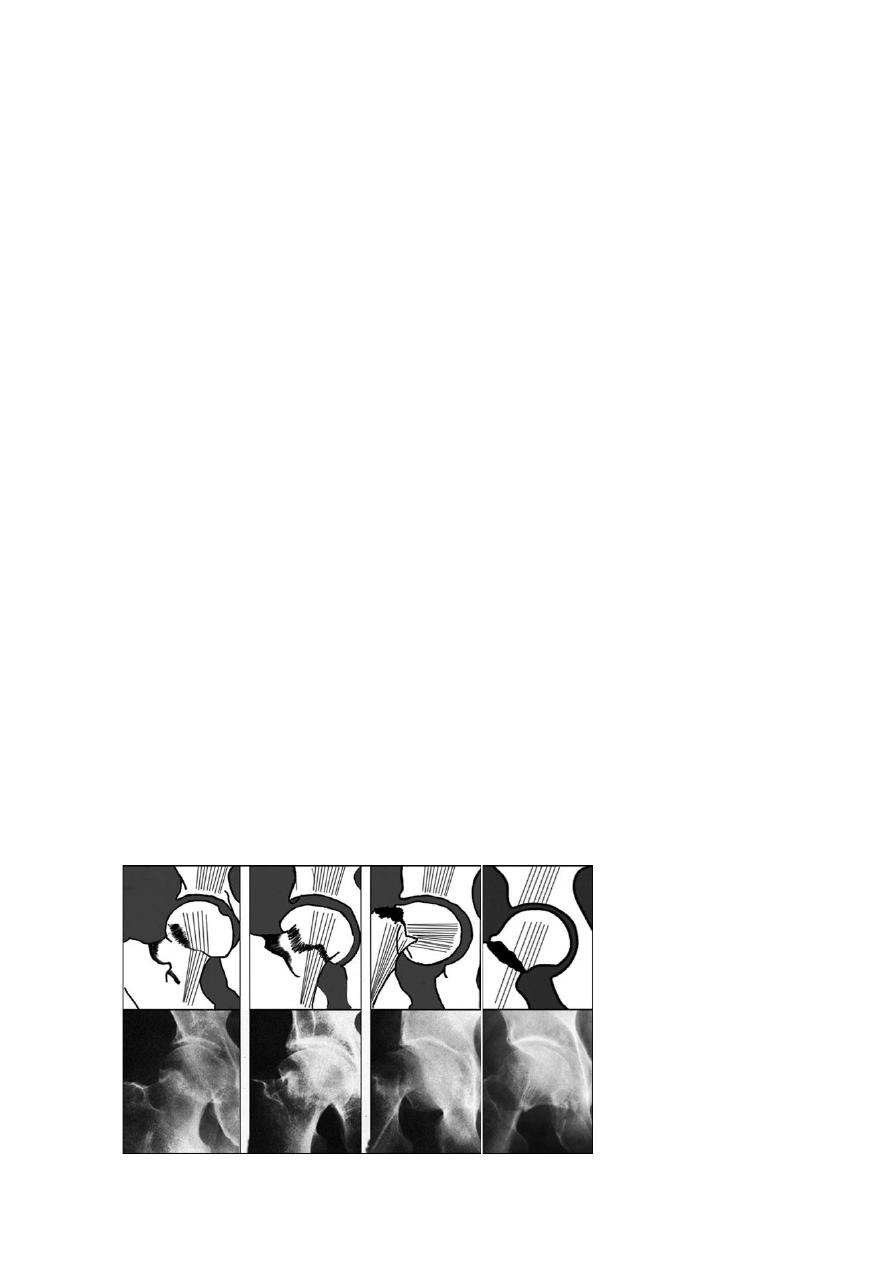
The most useful classification is that of Garden, which is based on the amount of
displacement apparent in the X-rays (Garden 1961). This is essentially a
radiographic classification:-
o Stage I is an incomplete impacted fracture, including the so-called abduction
fracture in which the femoral head is tilted into valgus in relation to the neck.
o Stage II is a complete but undisplaced fracture.
o Stage III is a complete fracture with moderate displacement.
o Stage IV is a severely displaced fracture.

The femoral head gets its blood supply from three sources:
(1) intramedullary vessels in the femoral nec
(2) ascending cervical branches of the medial and lateral circumflex
which run within the capsular retinaculum before entering the bone at the articular
margin of the femoral head.
(3) the vessels of the ligamentum teres.
The intramedullary supply is always interrupted by the fracture; the retinacular
vessels, also, may be kinked or torn if the fracture is displaced. In elderly people,
the remaining supply in the ligamentum teres is at best fairly meagre and, in 20 per
cent of cases, nonexistent. Hence the high incidence of avascular necrosis in
displaced femoral neck fractures.
Transcervical fractures are, by definition, intracapsular. They have a poor capacity
for healing because: by tearing the retinacular vessels and the injury deprives the
head of its main blood supply.
Fracture femoral neck has poor healing potential because it is intraarticular,
therefore:-
Flimsy periosteum
Capsular vessels torn by
#
Intracapsular haematoma tamponade effect
Synovial fluid haematoma will not clot
Clinical features
There is usually a history of a fall, followed by pain in the hip.
If the fracture is displaced, the patient lies with the limb in lateral rotation and the
leg looks short
.
With an impacted fracture the patient may still be able to walk.
Debilitated or mentally handicapped patients may not complain at all
– even with
bilateral fractures
.Femoral neck fractures in young adults result from road traffic accidents or falls
from heights and are often associated with multiple injuries.
A good rule is that young adults with severe injuries
– whether they complain of hip
pain or not should always be examined for an associated femoral neck fracture.
May be missed in the following and so the MRI or a bone scan for proved the
diagnosis :-
-- Stress
#
-- Impacted
#
-- Garden`s II
#
-- Debilitated pt.
-- Multiple #s
X-ray
Two questions must be answered: is there a fracture, and is it displaced?
Usually the break is obvious, but an impacted fracture can be missed.
This assessment is important because impacted or undisplaced fractures do well
after internal fixation, whereas displaced fractures have a high rate of non-union
and avascular necrosis.
Treatment
Initial treatment consists of pain-relieving measures and simple splintage of the
limb.

A case for non-operative treatment of undisplaced (Garden Stages I and II)
fractures can be made in treating patients with advanced dementia and little
discomfort.
For all others, operative treatment is almost mandatory.
Displaced fractures will not unite without internal fixation, and in any case elderly
people should be got up and kept active without delay if pulmonary complications
and bed sores are to be prevented.
Impacted fractures can be left to unite, but there is always a risk that they may
become displaced, even while lying in bed, so fixation is safer.
Another indication for non-operative management is an impacted Garden I fracture
that is an ‘old’ injury, where the diagnosis is made only after the patient has
been walking about for several weeks without deleterious effect on the fracture
position.
When should the operation be performed? In young patients operation is urgent;
interruption of the blood supply will produce irreversible cellular changes after 12
hours and, to prevent this, an accurate reduction and stable internal fixation is
needed as soon as possible.
In older patients, also, the longer the delay, the greater is the likelihood of
complications.
Internal fixation:-
Notwithstanding the advances in joint replacement, for most patients the
principles of treatment are as of old: accurate reduction, secure internal
fixation and early activity.
Maneuver of closed reduction:- with the patient under anaesthesia, the
fracture is disimpacted by applying traction with the hip held in 45
degrees of flexion and slight abduction; the limb is then slowly brought
into extension and finally internally rotated.
If a stage III or IV fracture cannot be reduced closed, and the patient is
under 60 years of age, open reduction through an anterolateral
approach is advisable.
However, in older patients (and certainly in those over 70), prosthetic
replacement is preferable
Once the fracture is reduced, it is held with cannulated screws or a
sliding screw and side-plate which attaches to the femoral shaft. A
lateral incision is used to expose the upper femur.
From the first day patients should sit up in bed or in a chair. They are
taught breathing exercises, and encouraged to help themselves and to
begin walking (with crutches or a walker) as soon as possible.
Prosthetic replacement:-
This procedure carries a longer operating time, greater blood loss and
a higher infection rate than internal fixation.
Prosthetic replacement is always preferable for stage III and IV
fractures particularly in the elderly.
Hip prostheses used for femoral neck fractures are usually of the
femoral part only (hemiarthroplasty) and may be inserted with or
without cement.
Total hip replacement for femoral neck fractures may be indicated: (1)
if treatment has been delayed for some weeks and acetabular damage
is suspected, or (2) in patients with metastatic disease or Paget’s
disease.
Postoperatively, breathing exercises and early mobilization are
important.
Complications
General complications
o deep vein thrombosis
o pulmonary embolism
o pneumonia
o bed sores
the mortality rate in elderly patients may be as high as 20 per cent at 4 months after
injury. Among the survivors over 80 years, about half fail to resume independent walking.
Avascular necrosis:
o Ischaemic necrosis of the femoral head occurs in about 30 per cent of
patients with displaced fractures and 10 per cent of those with undisplaced
fractures.
o A few weeks later, an isotope bone scan may show diminished vascularity.
o X-ray changes may not become apparent for months or even years.
o In patients over 45 years, treatment is by total joint replacement.
o In younger patients, the choice of treatment is controversial (Realignment
or rotational osteotomy, Arthrodesis) but in practice it is seldom carried out.
Non-union
o More than 30 per cent of all femoral neck fractures fail to unite, and the risk
is particularly high in those that are severely displaced. There are many
causes: poor blood supply, imperfect reduction, inadequate fixation, and
the tardy healing that is characteristic of intra-articular fractures. The
patient complains of pain, shortening of the limb and difficulty with walking.
The x-ray shows the sorry outcome.
Osteoarthritis
o Avascular necrosis or femoral head collapse may lead, after several years,
to secondary osteoarthritis of the hip. If there is marked loss of joint
movement and widespread damage to the articular surface, total joint
replacement will be needed.
THANK YOU
Dr. Jamal Al-Saidy
M.B.Ch.B. .F.I.C.M.S
