Eczema & Dermatitis
Eczema is an inflammatory reactive pattern of skin to many and
different stimuli characterized by itching, redness, scaling and
clustered papulovesicles.
Eczema and dermatitis are synonymous terms. These are the
most common skin conditions seen in the dermatology clinics all
over the world with a prevalence of 10% in the general population.
Clinical features:
The clinical signs are similar in all types of eczema and vary
according to the duration of rash.
Acute eczema reaction:
1- Redness and swelling, usually with ill- defined margins.
2- Papules, vesicles and, more rarely, large blisters.
3- Exudation and cracking.
4- Scaling.
Chronic eczema reaction:
1- May show all the above features, but it is usually less
vesicular and exudative.
2- Lichenification, a dry leathery thickening and increased
skin markings, is secondary to rubbing and scratching.
3- Fissures and scratch marks.
4- Pigmentation changes (hypo- and hyper- ).
Histopathological features:
The hallmark of acute eczema is edema of the epidermis
(spongiosis) and of the chronic eczema is hyperkeratosis and
acanthosis. Upper dermal vasodilatation and perivascular
inflammatory cells infiltrate occur in all stages of eczema.
Classification:
A. Exogenous:
1- Irritant contact dermatitis.
2- Allergic contact dermatitis.
3- Photodermatitis.
Others
B. Endogenous:
1- Atopic dermatitis.
2- Seborrhoeic dermatitis.
3- Discoid eczema.
4- Asteatotic eczema.
5- Gravitational eczema.
6- Lichen simplex chronicus.
7- Pompholyx.
8- Pityriasis alba.
Others
Complications:
1- Heavy bacterial colonization and super infection.
2- Local superimposed allergic contact dermatitis.
3- Severe forms of eczema affect the quality of life.
Treatment:
1- Topical treatment:
Acute weeping eczema:
Bed rest.
Liquid applications (e.g. K+permanganate soaks).
Topical steroid lotions or creams.
Non sticky dressings and clothes.
Subacute eczema:
Steroid creams are the mainstay of treatment.
Chronic eczema:
Best is steroid in an ointment base.
2- Systemic treatment:
1- Antibiotic for bacterial superinfection,
2- Antihistamines for itching, and
3- Short courses of systemic steroids may be needed.
Topical steroids:
These are commonly classified into 4 classes of potency:
Class
Potency
Example
Class I
Super
potent
0.05% Clobetasol
propionate
Class II
Potent
0.1% Betamethasone
valerate
Class III
Moderate
0.025% Flucinolone acetonide
Class IV Weak
1-2.5% Hydrocortisone
The potency of steroid used and the duration depend on the type
of lesion, its severity and the type of patient, e.g:
• Nothing more than mild potency topical corticosteroid should be
used on: the face,
intertrigenous area, or
in infancy
except in specialized circumstances.
• Very potent steroid should not be used for long time. (>2 weeks).

Exogenous Dermatitis
These are mainly caused by exogenous (contact) factors:
1- Irritant contact dermatitis.
2- Allergic contact dermatitis.
3- Photodermatitis.
Others
Irritant Contact Dermatitis
Is an inflammatory reaction of the skin occurs from exposure to an
irritant for sufficient time and in sufficient concentration.
Immunological process is not involved and pervious sensitization is
not required for dermatitis occur.
Irritant is any substance capable of inducing cell damage if
applied for sufficient time and concentration. These may be weak
or strong irritants.
There is a wide range of susceptibility for weak irritants and
they usually cause chronic dermatitis after repeated exposures
while strong irritants produce acute reactions after brief exposure.
The main irritants are alkalis (detergents, soaps, bleaching
agents), acids, solvents, petroleum and dusts. Water can cause
irritant contact dermatitis.
Treatment is based on:
Avoidance of irritant (or protection from it)
The use of topical steroids and emollients.
Examples of Irritant Contact Dermatitis
1- House-wife dermatitis
A very common disease frequently seen among housewives (or
males in certain jobs) due to frequent washing. Water and
detergents cause the irritation. The eruption begins with dryness
and redness of fingers especially the tips, chapping is seen on the
back of hands, and erythematous hardening of the palms with
fissures develop. Allergic contact dermatitis may develop
secondarily.
2- Napkin eczema
Mainly affects infants and babies at the site of underwear due to
repeated and sustained exposure to urine and faeces. Elderly
incontinent people may be affected also. Glazed and sore

erythema affects the napkin area and usually spares the skin folds.
Bacterial or candida superinfection is common.
3- Lip licking dermatitis
Usually seen in young children due to frequent wetting of the lip by
licking. Repeated cycles of wetting and drying will eventually cause
chapping and then eczema.
Allergic Contact Dermatitis
An acquired sensitivity to various substances that produces an
inflammatory reaction in those (& only those) who have been
exposed to the allergen previously.
The mechanism is delayed type IV hypersensitivity reaction. First
exposure to the allergen is required to induce hypersensitivity but
no clinical reaction. The allergen is then carried by langerhans
cells to local lymph nodes where memory T-cells are produced.
This is called (the induction phase) and take about 3 weeks.
Second exposure to the same allergen will stimulate the memory
cells that induce lymphocytes proliferation and cytokine release,
producing the dermatitis. This is called (the elicitation phase).
Sensitization is systemic, persist indefinitely and desensitization is
seldom possible.
Common allergen are:
Nickel (jewelry),
Dichromate (cement,
leather),
PPD (hair dye),
Parabens (cosmetics),
Colophony (plaster),
Neomycin (topical antibiotic).
Examples of Allergic Contact Dermatitis :
1- Earlobes dermatitis: due to nickel-containing ear ring. Similar
reaction can occur on the wrists, and/or fingers of nickel-sensitized
individuals..
2- Cement dermatitis: due to dichromate found in cement.
3- Eyelid dermatitis: may be caused by nail varnish, preservatives
in local medications, or it could be air born ACD.
4- Lipstick dermatitis, hair dye dermatitis, shoes dermatitis.
Diagnosis:
Is confirm by (Patch Test), which depend on type IV cell mediated
hypersensitivity reaction. The test is don by applying the suspected
allergens on the back of the patient under occlusive aluminum
discs or patches for 48 hrs, the removed. Positive reactions
produces erythema, papules and vesicles at the site of the allergen
disc or patch.
Treatment :
Same as in irritant contact dermatitis.
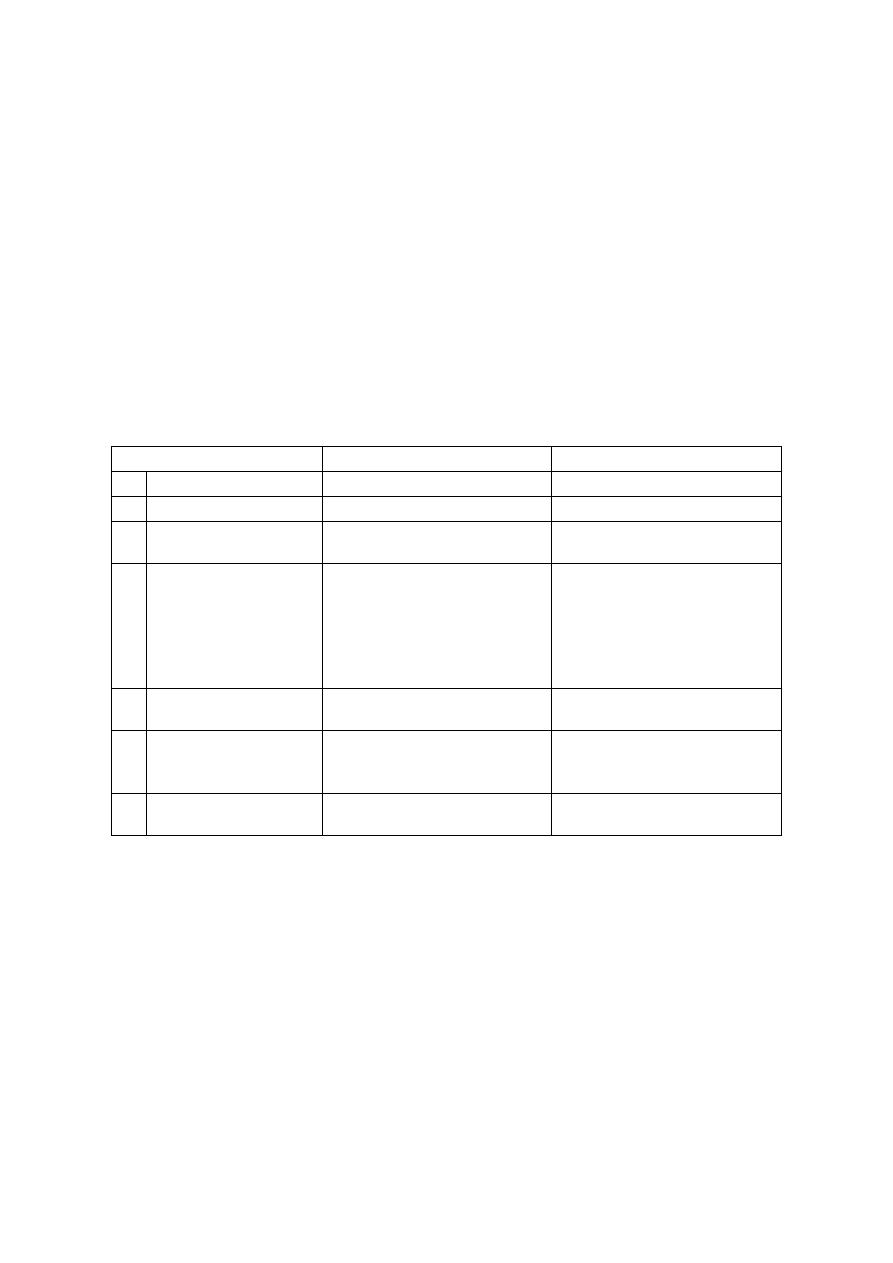
Main differences between two types of contact dermatitis
Feature
Irritant CD
Allergic CD
1
Cause :
Irritant.
Allergen.
2
Previous exposure: Not required.
Essential.
3
Affected sites:
Sites of direct contact with
little extension.
Sites
of
contact
and
distant sites.
4
Timing:
Rapid onset (4-12 hours)
after contact.
Lesions develop at first
exposure
Onset generally after 24
hours
or
longer
after
exposure.
No
lesions
after
first
exposure.
5
Mechanism:
Direct
effect
(non
immunological).
Type IV hypersensitivity
reaction (immunological).
6
Susceptibility:
Everyone susceptible in
varying
degrees
to
appropriate concentration.
Only
some
patients
susceptible.
7
Patch test
No role
Helpful
to
confirm
diagnosis.



