Dermatophytoses
Introduction
Dermatophytoses are fungal infections caused by three genera of fungi that have
the ability to invade and multiply within keratinized tissue (hair, skin and
nails):include
(1) Trichophyton
(2) Epidermophyton
(3) Microsporum
Epidemiology
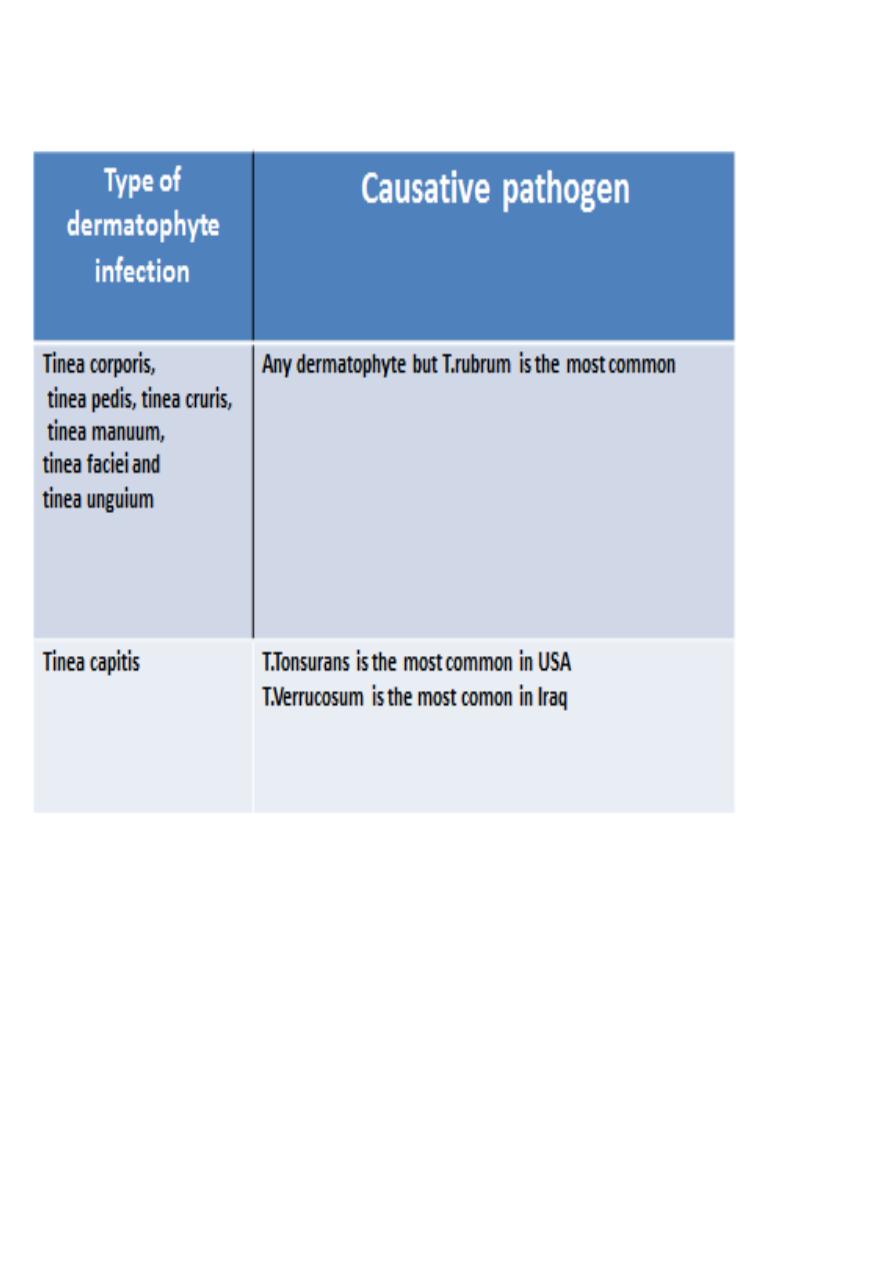
Trichophyton rubrum is the most common dermatophyte worldwide
Dermatophytoses occur most frequently in postpubertal hosts except tinea capitis
which occurs mainly in prepubertal children
Men tend to more frequently have tinea cruris and tinea pedis than women
Pathogenesis
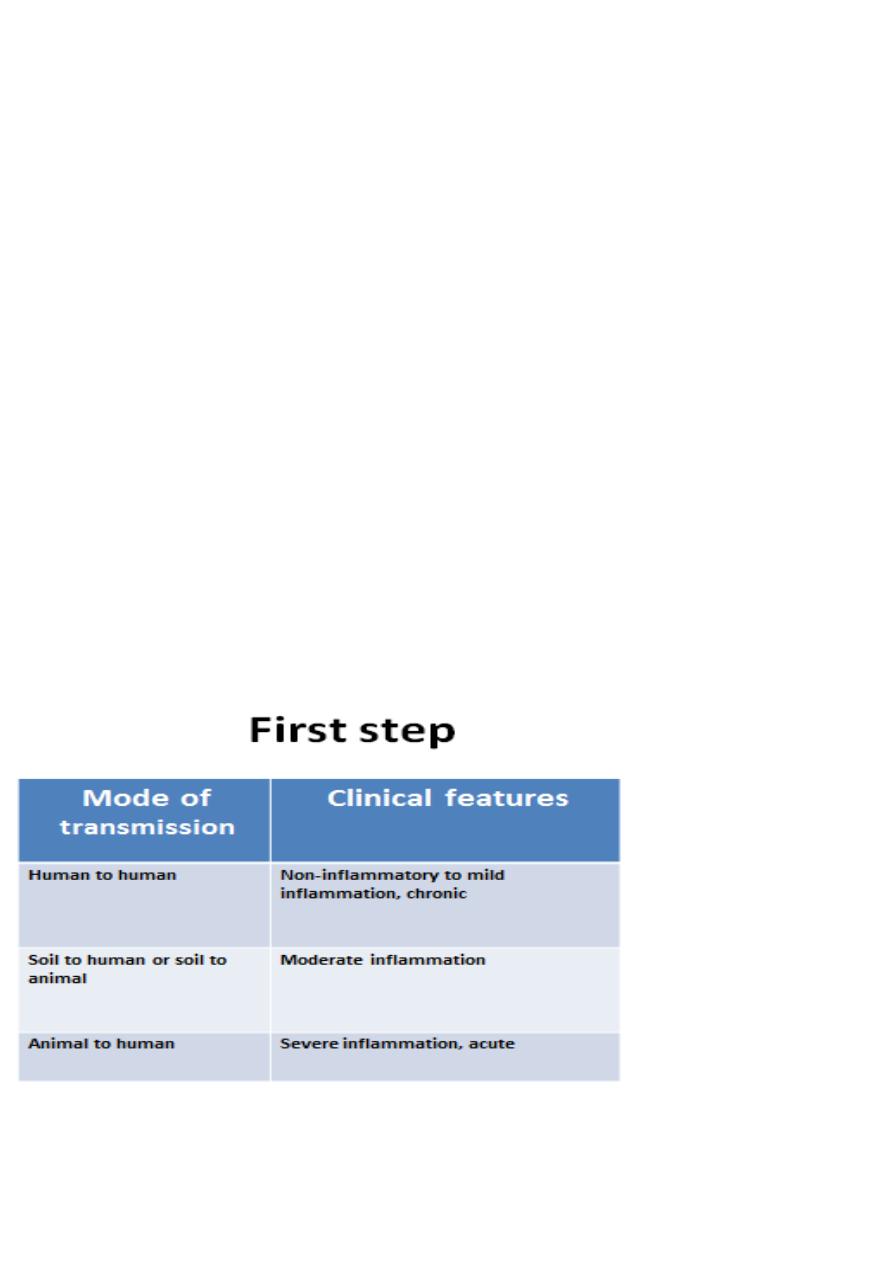
The first step
: fungus comes in contact with the skin via three sources
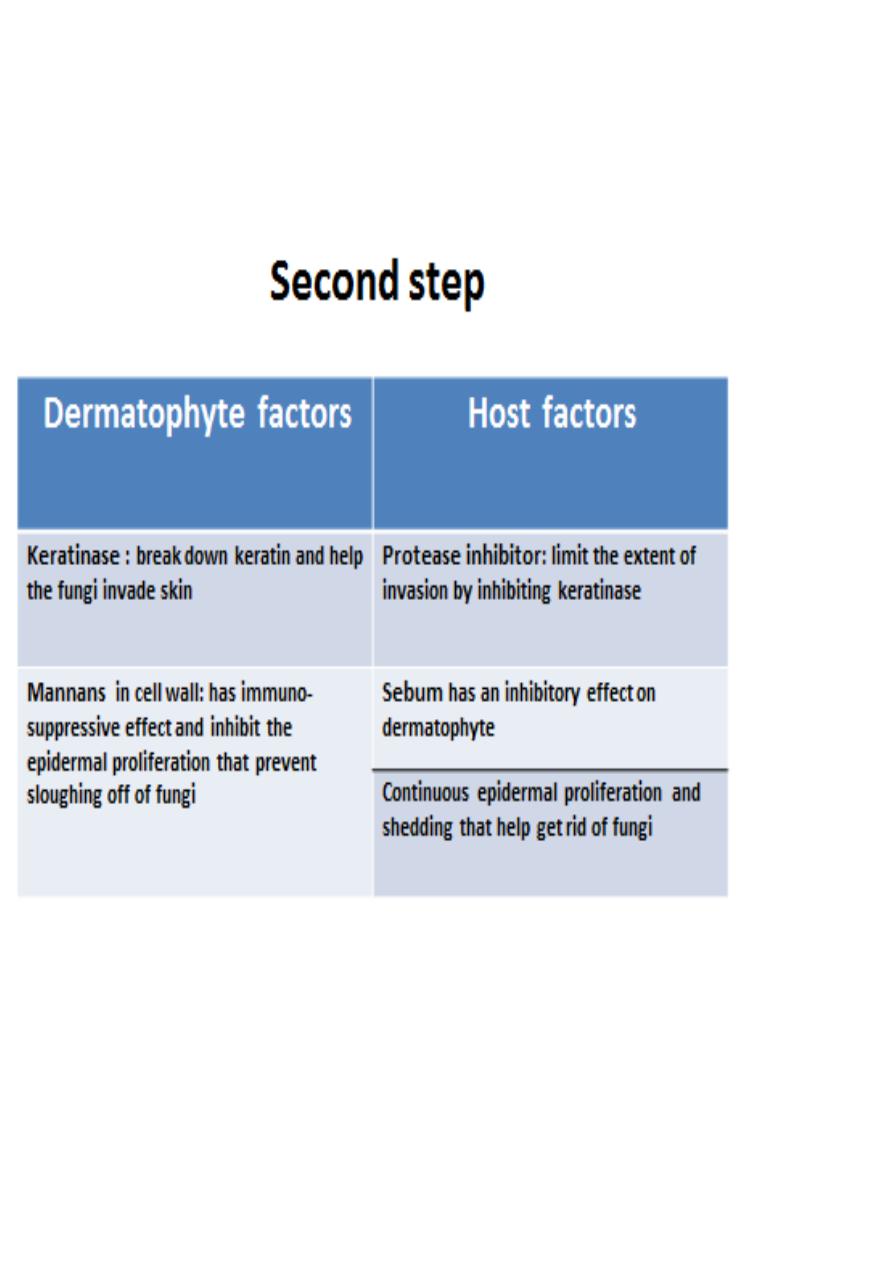
The second step
: how the fungus invade the skin

Clinical features
Tinea corporis
Infection of the skin of the trunk and extremities, excluding the hair, nails, palms,
soles and groin
Any dermatophyte can cause it but T. rubrum is the most common pathogen
Infection spreads centrifugally from the point of skin invasion resulting in a raised,
erythematous, scaly advancing border and a central clearance (annular or circinate
lesion)
Variants:
Tinea incognito: tinea lesion modified by topical steroids, may lack a raised scaly
active border.
Majocchi’s granuloma: is characterized by follicular papules or nodules, commonly
seen in women who have tinea pedis or onychomycosis and shave their legs.
Tinea cruris (Jock itch)
Infection of the inguinal region
This disease is more often seen in men than in women, since the scrotum provides
a warm and moist environment that encourages fungal growth
The inflicted patients are more likely to have tinea pedis and onychmycosis as a
source of dermatophytes(which are transmitted from these places to inguinal area)
Other predisposing factors include obesity and hyperhidrosis
Presented clinically similar to tinea corporis
The scrotum itself is generally spared, unlike candidiasis of groin
Tinea manuum
Infection of the palm and interdigital spaces
It is different from that of back of hands due to lack of sebaceous glands on the
palms
Often unilateral

It presents as a diffuse hyperkeratosis of the palms and digits with accentuation of
scales on creases that fails to respond to emollients
An important clinical clue is tinea unguium
Is often present in patients with tinea pedis (two feet and one hand syndrome)
Tinea pedis(Athlete's foot)
infection of the soles and interdigital spaces of the feet
The feet are the most common location for dermatophyte infections
More common in adults
Lack of sebaceous glands and moist environment due to occlusive shoes are
predisposing factors
Tinea pedis is uncommon in populations that do not wear shoes although the
barefoot people can acquire the fungus in public facilities i.e. gym
Clinical types:
(1)Moccasin: diffuse hyperkeratosis, scaling and erythema
(2)Interdigital : the most common type; erythema, maceration, fissures and
ulceration in web spaces
Tinea barbae
Involves the bearded areas of the face and neck in men
Two types:
(1) Deep type: produces nodules and kerion -like boggy swellings. Acquired from
animal.
(2)Superficial type: less inflammatory, characterized by folliculitis . Acquired from
contaminated razors in barber- shops. Now less common owing to use of
disposable instruments and use of disinfectant
In both types: the hairs are either easily plucked or lost.
Tinea faciei
Infection of face
Typical annular lesions are usually lacking and the lesions are photosensitive;
therefore, Frequently misdiagnosed

Tinea capitis
A common dermatophyte infection of the scalp in children, whereas adult infection
occurs infrequently
T. tonsurans is currently the most common cause of tinea capitis in the US while
T.verrucosum in Iraq
The “carrier state” of tinea capitis is contagious to others through hats, brushes,
towels or barber instruments
There are two clinical types:
(1)Non-inflammatory:
Gray patch: present as a dry scaly patch of alopecia
Black dots: caused by hair breakage near the surface
(2)Inflammatory:
Kerion: caused by M.canis, present as a boggy, purulent plaques with abscess
formation and associated alopecia, patient may become febrile with extensive
lymphadenopathy
Favus: caused by T. schoenleinii, the most severe type of dermatophyte hair
infection, present as , sulfur-yellow crusts composed of hyphae and skin debris
pierced by hairs (“scutula”)
Tinea unguium (dermatophytic onychomycosis)
Infection of the nail unit
Three clinical types:
(1)Distal/lateral subungual: most common
(2)Superficial white:
(3)Proximal subungual: seen frequently in immunocompromised hosts.
Multiple nails on one or both hands or feet are usually affected
Affects women more often than men
Fingernail infections are considerably more common than toenail
Clinical features:

(1)Hyperkeratosis of nail bed
(2)Thickenening and yellowish discoloration of nail plate
(3)Onychlysis (seperation of nail plate from nail bed)
Diagnosis of dermatophytoses
Clinical examination (most important)
KOH examination of skin scraping (by blade), nail clipping (by nail clipper) or hair
plucking(by tweezer) under microscope after adding KOH to specimen to look for
hyphae
Wood’s lamp (ultraviolet light of 365 nm wavelength): Infected hairs show yellow-
green fluorescence in a dark room
Culture: 2-4 weeks
Biopsy: we see hyphae in stratum corneum
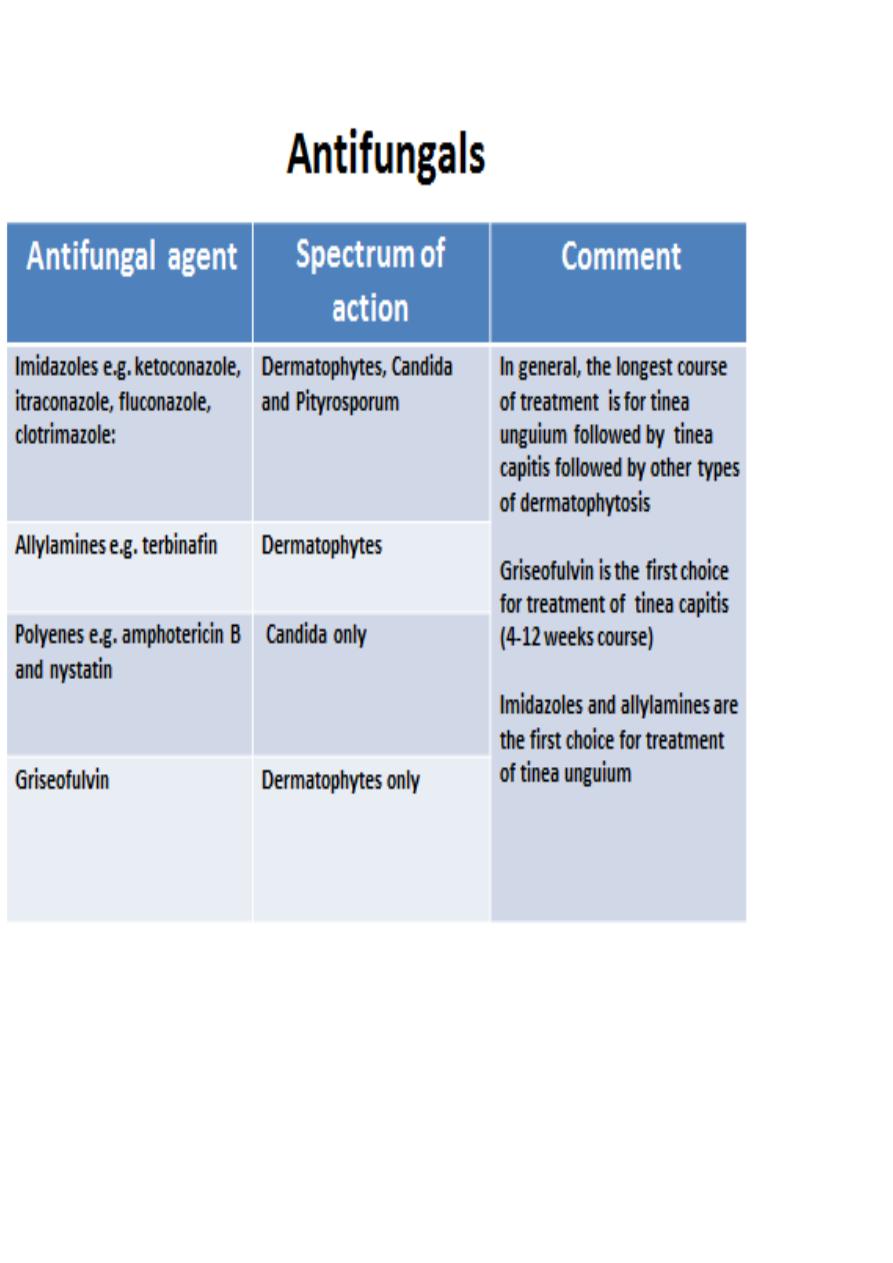
Treatment
Topical antifungals e.g. clotrimazole and ketoconazole are the first line treatment
Systemic antifungal: indications
(1)tinea manuum, ( 2) tinea pedis, (3)tinea capitis, (4) tinea barbae, (5)tinea
unguium and (6)when extensive area of skin is involved