1
Disorders of the conjunctiva
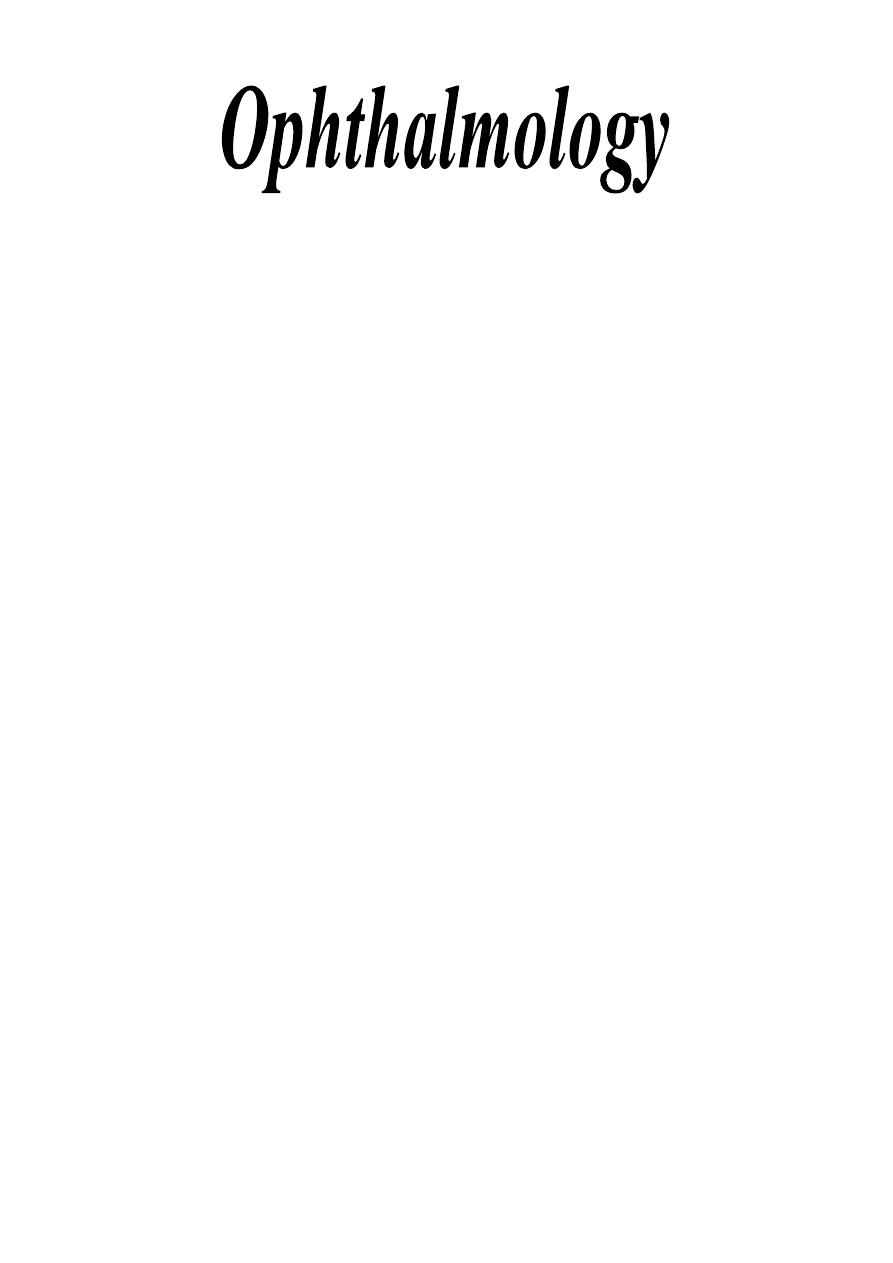
Applied anatomy:
Conjunctiva is a transparent layer. It consists of two layers:
1- Epithelium: 2-5 cell layers, basal cells are cuboidal and superficial cells are
flattened polyhydral.
2- Stroma (substantia propria): It is a richly vascularized connective tissue.
3- Mucin secretors: They are of three types:
a- Goblet cells.
b- Crypts of Henle: Found at upper part of tarsal plate.
c- Glands of Manz.
Function: Lubrication.
4- Accessory lacrimal glands:
a- Krause.
b- Wolfring.
They are found deep in stroma mainly at fornices.
* Plus these accessory lacrimal glands, there is the main lacrimal gland that
resides in the superotemporal orbit, partially within a shallow bony fossa in the
lateral angular process of the frontal bone (fossa glandula lacrimalis).
5- Clinical parts:
a- Palpebral: starts at the mucocutaneous junction, it is firmly adherent to
the tarsal plate.
b- Forniceal: loose, redundant part, it swells easily.
c- Bulbar: it covers the anterior surface of sclera.
dr.Imad H.
Sachit
CABO, FICO,
DO.
2
Clinical Evaluation of conjunctival inflammation:

3
Bacterial Conjunctivitis
1- Simple bacterial conjunctivitis:
It is a common disease, and usually it is self-limiting condition. Common
causative organisms are:
- Staphylococcus epidermidis.
- Staphylococcus aureus.
- Other like Strptococcus pneumoniae, H. influenzae.
Symptoms:
- Acute onset of redness.
- Grittiness
(
) . خشونة أو رمل بالعين
- Burning.
- Discharge.
- On morning, eyelids are stuck together due to accumulation of exudates
during the night.
- Both eyes are usually involved.
Signs:
- The eyelids are crusted and edematous (mild edema).
- Mucopurulent discharge.
- Beefy-red injection, maximally in the fornices.
- Membranes in severe cases.
- Corneal involvement is uncommon.
* Blurred vision may occur due to mucus not due to corneal involvement.
Treatment:
- Usually resolves within 10-14 days and laboratory tests are not routinely
performed.
- Bathe all discharge away.
-Topical drops (Antibiotics): Chloramphenicol, ciprofloxacin, ofloxacin,
gentamicin, neomycin, tobramycin.
- Antibiotic ointments: higher concentration for long period and we give it at
night because it causes blurred vision, we have chloramphenicol, gentamicin,
tetracyline, framycetin.
2- Adult gonococcal keratoconjunctivitis:
- Caused by: Gram-negative diplococcus Neisseria gonorrhoea.
- It is a rare condition.
Symptoms:
- Hyperacute presentation.
- Profuse and thick creamy (purulent) pus.
Signs:
- Eyelids are oedematous and tender.
- Discharge is profuse and purulent.

4
-Intense
hyperaemia
(conjunctival
injection),
chemosis
and
pseudomembranes format.
- Preauricular lymphadenopathy and sometimes suppuration of nodes.
- Keratitis may occur in severe cases.
Treatment:
- Hospitalization (we should admit this patient to hospital).
- Cultures.
- Eye irrigation with saline (frequent)
- Antibiotics:
i- Systemic antibiotics:
*cefotaxime 500mg * 4 i.v for 1 day incase of conjunctivitis only or for
3-5 days if it is associated with keratitis.
* Spectinomycin in penicillin-resistant cases.
ii- Topical Antibiotics:
* Gentamicin, or
* Bacitracin.
3- Neonatal Keratoconjunctivitis:
* Ophthalmia neonatorum is any infection of the eye within one month from
birth.
C.
trachomatis,
N.gonorrhoeae,
H,simplex,
staph,
strept,
topical
preparation(silver nitrate)
Treatment:
Chemical: no treatment
Mild: topical treatment
Moderate-Severe infection: Systemic and tropical.
Viral Conjunctivitis
1- Adenoviral keratoconjunctivitis:
- It is a highly contagious virus.
- Transmission is via respiratory or ocular secretion.
- Dissemination is by contaminated towels or equipments.
- Incubation period is 4-10 days; it is an occupational hazard of
ophthalmologists (due to contamination of the hands).
Clinically there are two ocular syndromes:
a- Pharyngoconjunctival fever (PCF):
- Caused by serotypes 3 & 7.
- Typically affects children and causes URT infection (systemic
manifestations as pharyngitis, fever and pre-auricular lymphadenopathy).
- Keratitis develops in about 30%.

5
b- Epidemic keratoconjunctivitis (EKC):
- Caused by serotypes 8 & 19.
- Usually not associated with systemic symptoms.
- Keratitis occurs in about 80%, so it is more serious due to affection of
visual acuity.
Conjunctivitis:
Presentation: acute onset of watery discharge, redness, discomfort and
photophobia, both eyes are affected in 60% of cases.
Signs:
- Eyelids are oedematous.
- Watery discharge.
- Mild chemosis to moderate.
- Follicular reaction.
- Subconjunctival haemorrhages.
- Pseudomembranes.
- Lymphadenopathy is tender.
Keratitis:
Stage I: Within 7 days of onset, diffuse epithelial keratitis .
Stage II: after 7 days, focal (patchy multiple foci)sub epithelial keratitis.
Stage III: anterior stromal infilterate
If they are untreated, they may persist for months or years.
Treatment:
a- Avoid transmission following examination of patients:
- Washing of hands.
- Meticulous disinfection of ophthalmologic instruments.
b- Medications:
i- For conjunctivitis:
- Spontaneous resolution occurs within 2 weeks.
- Antiviral agents are ineffective (has no role).
- Topical steroids are indicated only in very severe inflammation.
ii- For keratitis:
- topical steroids, which are indicated only if the eye is uncomfortable or
there is diminishing of the visual acuity by stage II, III lesions, all that
after exclusion of Herpes simplex infection.
Note:
Steroids do not shorten the natural course of the disease but suppress
the inflammation and relief symptoms.
2- Herpes simplex conjunctivitis:
Conjunctivitis may occur in patients with primary Herpes simplex infection.

6
- when the person catches the infection for the first time it is primary, after
treatment, the virus get dormant in the trigeminal nerve ganglia, for any reason
if the person get immune-compromised, then secondary infection is developed.
Signs:
- The eyelids and periorbital skin show unilateral herpetic vesicles, which
may be associated with oedema.
- Watery discharge.
- Ipsilateral follicular reaction.
- Lymphadenopathy is tender.
- Keratitis, Herpes simplex infection is very severe and it can lead to
dendritic ulcer of the cornea.
- No subconjunctival haemorrhage.
Treatment: Antiviral agent (as Acyclovir "Zovirax™") for 21 days to prevent
keratitis.
3- Molluscum contagiosum conjunctivitis:
- It is an oncogenic virus that produces characteristic lesions on the skin and
less commonly on the mucus membranes (e.g. conjunctiva).
- It spread by close contact.
- Typically affects adolescent children and young adults.
- Also it is common in the patients with AIDS (i.e. immune-compromised).
Signs:
- Small, pale, waxy and umbilicated nodule in the eyelid margin.
- Follicular conjunctival reaction.
- In longstanding cases, there is associated epithelial keratitis
Treatment:
Destruction of lesions by shave excision (surgical shaving), cryotherapy or
cauterization.
Chlamydial Conjunctivitis
1- Adult chlamydial keratoconjunctivitis:
It is a sexually transmitted disease caused by the obligate intracellular
bacterium Chlamydia trachomatis (serotypes D, E, F, G, H, I, J & K).
- Patients are usually young and at least 50% have a concomitant genital
infection (cervicitis in ♀ or urethritis in ♂).
Mode of transmission:
- Autoinoculated from genital secretions.
- Eye to eye spread is rare.
Incubation period: 1 week.
Presentation:
Subacute onset of unilateral or bilateral mucopurulent discharge.
Signs:

7
- Eyelids are lightly oedematous.
- Mucopurulent discharge.
- Conjunctival reaction: At first, there is papillary hypertrophy then large
follicles are formed at the inferior fornix but may involve upper tarsal
conjunctiva.
- Lymphadenopathy (not tender).
- Keratitis is uncommon.
- Conjunctival scarring + Pannus (neovascular or fibrovascular membrane
involving superficial part of cornea, i.e. affects the cornea not the
conjunctiva).
Treatment:
a- Topical therapy: Tetracycline ointment *4 for 6 weeks.
b- Systemic therapy: One of the following:
i- Doxycycline: 100mg *1 for 1-2 weeks.
ii- Tetracycline: 250mg *4 for 6 weeks.
iii- Erythromycin: 250mg *4 for 6 weeks.
2- Neonatal chlamydial conjunctivitis:
- The most common cause of neonatal conjunctivitis.
- topical tetracycline & systemic erythromycine
3- Trachoma:
- It is an infection caused by serotypes A, B, B
a
and C of Chlamydia
trachomatis.
- It is a disease of underprivileged populations with poor conditions of
hygiene (low socioeconomic status).
Transmission:
Common fly is the major vector, currently trachoma is the leading cause of
preventable blindness in the world.
Presentation: is usually during childhood.
Signs:
- Follicular reaction associated with diffuse papillary reaction but under age
of 2 years, the papillary reaction is predominant.
- Chronic conjunctival inflammation causes conjunctival scarring that
involves the entire conjunctiva but most prominent on the upper tarsus.
- Progressive conjunctival scarring: if it is severe lead to:
* Destruction of lids.
* Trichiasis: Misdirection of eyelashes towards the cornea causing
rubbing of cornea.
* Dry eyes, due to destruction of goblet cells and lacrimal ducts.
- End-stage trachoma:

8
* Corneal ulceration .
World Health Organization (WHO) grading:
TF: Trachoma follicles (5 or more follicles in the superior tarsal conjunctiva).
TI: Trachomatous intense inflammation diffusely involving the tarsal
conjunctiva.
TS: Trachomatous conjunctival scarring.
TT: Trachomatous trichiasis touching the cornea.
CO: Corneal opacity.
Treatment of trachoma:
-indicated for stages I & II (TF & TI), as there is no benefit from treating
stages III, IV &V as there is no active organism (and even the medications
used or applied may cause scarring).
- Preventive measures: strict personal hygiene, especially washing the face
of young children .
- Single dose of Azithromycin plus systemic erythromycin.
Allergic conjunctivitis
1- Allergic rhinoconjunctivitis (acute allergic conjunctivitis):
- The most common type of eye allergy.
- It is a hypersensitivity reaction (type I) to a specific airborne antigens.
-Usually there is associating nasal symptoms (so it is called rhinoconjunctivits)
that is thought to be a result of one or more of the following fact:
a- Direct effect of the allergen on the nasal mucosa and conjunctiva.
b- We have nasolacrimal drainage, so the excessive tears produced are
drained to the nose.
c- As both of them (the conjunctiva and nasal mucosa) are supplied by
pterygopalatine ganglia, so the stimulation of one of them will leads to
stimulation of the other.
- There are two types:
a- Seasonal allergic rhinoconjunctivitis:
- Acute onset of "hay fever" symptoms.
- The most common allergens are pollens.
- Usually occurs during summer.
b- Perennial allergic rhinoconjunctivitis:
- less severe and less prevalent than seasonal allergic rhinoconjunctivitis
- Usual allergens are house-dust mites or animal dander.
- Symptoms occurs throughout the year.

9
Presentation:
Acute, transient attacks of slightly red, itchy and watery eyes associated with
sneezing and a water nasal discharge.
Signs:
- Mild to moderate lids oedema
- Periorbital oedema in severe cases.
- Milky or pinkish appearance of conjunctiva as a result of oedema and
injection.
- Mild papillary reaction in the upper tarsal conjunctiva.
Treatment:
Either topical mast cell stabilizer e.g. nedocromil & lodoxamide, or topical
antihistamine e.g. levocabastine & azelastine.
* Only in very rare and severe cases we need topical steroids.
2- Vernal keratoconjunctivitis (spring catarrh):
- It is a recurrent, bilateral, external, ocular inflammation affecting children
and young adults.
- More common in male than females.
- Vernal keratoconjunctivitis is an allergic disorder in which IgE and cell-
mediated immune mechanisms play an important role (hypersensitivity
reactions type I & IV).
- Atopic patients often develop asthma and eczema in infancy.
- The onset of vernal keratoconjunctivitis is usually after the age of 5 years (5-
8y) and the condition eventually resolves around puberty, only rarely
persisting beyond the age of 25 years.
- As its name suggests (seasonal basis), the peak incidence of symptoms occur
between April and August but many patients have year-round disease.
- The condition is more common in warm, dry climate and less frequently in
colder climates.
Clinical features:
The main symptoms are:
- Intense ocular itching.
- Lacrimation.
- Photophobia.
- Foreign body sensation.
- Burning.
- Thick mucus discharge.
- Ptosis also occurs (it is a mechanical ptosis as it occurs due to chronic
inflammation and oedema that causes heaviness and increased weight of the
eyelid).
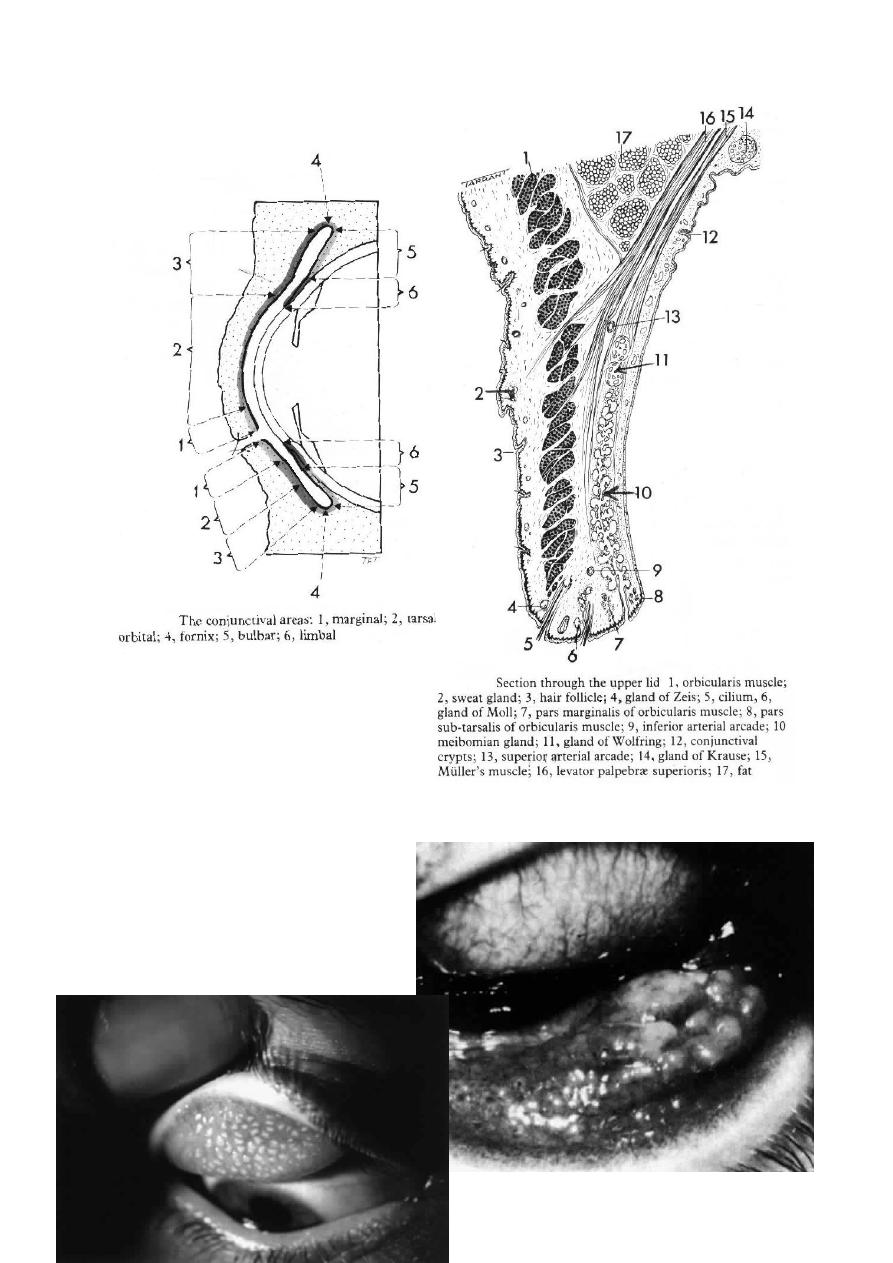
There are three main types (according to anatomical distribution of vernal
disease):
10
a- Palpebral, b- Limbal and c- mixed.
Signs:
For conjunctivitis:
* For palpebral vernal keratoconjunctivitis, signs in chronological order:
- Conjunctivitis hyperaemia.
- Diffuse papillary hypertrophy mostly on the superior tarsus (tarsal
conjunctiva).
- Enlarged of papillae ends in flat-topped polygonal appearance
(cobblestones).
* For limbal vernal keratoconjunctivitis:
- It is characterized by mucoid nodules that have a
smooth round surface.
- Discrete white superficial spots (Trantas dots);
which are composed of collections of inflammatory
predominantly eosinophils, are found scattered
around the limbus.
* For mixed vernal keratoconjunctivitis:
- There is papillary reactions and Trantas dots.
For keratitis:
- Punctate keratopathy (epithelial erosions, micro erosions), it is the earliest
finding.
- Macro erosions (result of continued epithelial loss, i.e. small ulcers).
- Plaque (macro erosions coated by layers of mucus which cannot be wetted by
tears and resists epithelization).
- Subepithelial scarring (sign of previous severe corneal involvement), it
occurs due persistent inflammation that prevents healing).
- Pseudogerontoxon, which resembles as arcus senilis. It is seen in the outline
of previously inflamed limbus (occurs if the epithelial scarring and
opacification are in periphery the limbus).
Treatment:
1- Topical steroids: (its use is mandatory)
- As the patients will not heal by any drug, so we use weak steroids as
fluorometholone rather than dexamethasone, betamethasone or prednisolone
as weak ones are of less penetration to cause increase in IOP or to cause
cataract as the strong steroids.
- Short course.
- Potent steroid, long course causes increase in intraocular pressure and
cataract, so the patient get blind due to use of topical steroids, especially seen
in those jumping from one doctor to another as no one can cure them.
2- Mast cell stabilizers:
nedocromil 0.1% drops *2 daily
or lodoxomide 0.1% drops *4 daily.

11
or sodium cromoglycate 2% *4 daily
They are not effective as steroids in controlling acute exacerbation (as their
actions starts when all mediators released are used, so their action delays for
few days).
3- Acetylcyseine 5% drops *4 daily, as treatment of early plaque formation
(mucolytic).
4- Topical cyclosporin A: used in steroids resistant cases.
5- Debridement: of early mucus plaques
6- Supratarsal injection of steroids: it is very effective in patients with severe
disease unresponsive to conventional therapy.
Dr.IMAD H. SACHIT
CABO , FICO , DO.

12
