DYSMENORRHEA
Definition is painful menstruation
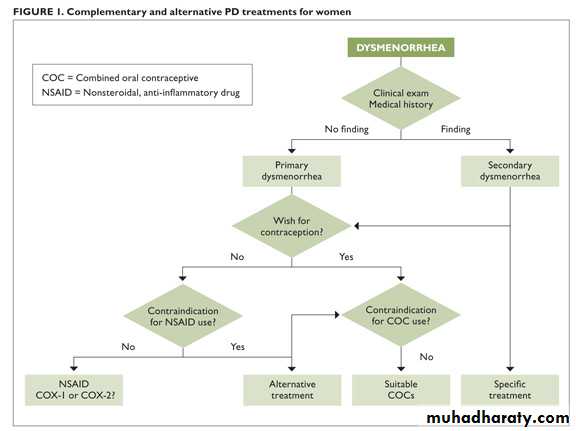
Classification :1. primary dysmenorrhea2.secondary dysmenorrhea
Epidemiology
. the age and parity are inversely related to the incidence of dysmenorrhea. family history
. stress increase incidence
. smoking . low body mass index
. early menarche . heavy menstrual loss
. exercise and high intake of fruit and vegetables reduce incidence
. psychological morbidity . sexual abuse
Causes
Primary dysmenorrhea. uterine myometrium hyperactivity
. excess prostaglandin production during menstruation –increase myometrium contraction –reduction uterine blood flow –increase ischemia and pain
. physiological
. ovulatory cycle is essential for development
Secondary dysmenorrhea
. underlying pathological causes. causes gynecological
. endometriosis . adenomyosis. uterine fibroid
. cervical stenosis and other obstructive causes
. pelvic venous congestion
. residual \trapped ovary syndrome
. pelvic adhesion . pelvic inflammatory disease
Gastrointestinal: irritable bowel syndrome
Chronic constipation
Urinary tract :bladder pain syndrome (interstitial cystitis )
Musculoskeletal :pelvic floor myalgia
Myofascial pain
Neurology :nerve entrapment
Symptoms and sign
Primary spasmodic dysmenorrhea:.is colicky cramping suprapubic pain that may radiate to the back and thigh
. associated with gastrointestinal and systemic symptoms.is usually begin few hours before or within the onset of menstruation
. continue for 8 to 72 hour
. typically, in young female
. onset within 6- 12 months after menarche
. cause significant morbidity and negative pelvic pathology
Secondary dysmenorrhea
. pain associated with identifiable pelvic pathology.is more sever before menstruation
. exacerbated by menstruation and continue throughout the cycle
. usually associated with deep dyspareunia
. usually more common in older woman
INVESTIGATION
Investigation of primary dysmenorrhea is unnecessary unless there are atypical symptoms or abnormal finding on pelvic examination
. ultrasound: endometriomata, PID sequelae, fibroid, congenital abnormalities
.STI screan including chlamydia swab. laparoscopy is usually reserved for woman with ultrasound abnormalities, medical treatment failure or those with concomitant subfertility
. hystrosalpingogram useful to identify intrauterine adhesion
.MRI
TREATMENT
In the majority nothing more than general advice, reassurance and empirical relief of painThe girl should realize that her complaint is likely to be short lived
NSAIDs :produce moderate or excellent pain relief
More effective than paracetamolSelection according to cost and patient preference (naproxen ,mefenamic acid ,diclofenac ……)
Limited by its side effect
May be used in combination with another drug like codeine and paracetamol
Calcium channel blocker
Oral contraception
For inhibition of ovulationLNG-IUS
Effective for pain and as contraceptionGnRH analogues
Act through induce hypo estrogen stateLimited use
Relive the symptom if waiting for hysterectomy or as a form of assessment as to the benefits of hysterectomy
Heat :effective as NSIAD in relieving pain
Life style changes.low fat ,vegetable diet may improve the symptoms
.exercise may improve symptoms by improving blood flow to the pelvis
.vitamin B1 and magnesium
Treatment of underlying pathology in case of secondary dysmenorrhea
Therapeutic laparoscopy :diagnosis and management of endometriosis adhesion and PID.hysterectomy is now rare
. laproscopic uterine nerve ablation is not currently recommended.injection of pelvic plexus with anesthetic agent
.dilation of the cervix
Self-assessment
Q1: how can you clinically differentiate between primary and secondary dysmenorrheaQ2:what types of birth control methods help control dysmenorrhea ?
Q3: what is the surgery done to treat dysmenorrhea
Q4 :what alternative treatment help ease dysmenorrhea (non medical)
..