Polycystic Ovary Syndrome (PCOS) and Metabolic Syndrome
Alaa AL-NaserAssisted Professor of Obstetrics.Gynae
Thiqar medical college
specialist Obstetrician & Gyne
Bint AL-Huda teaching Hospital
Clinical teacher
Continuous medical education
PCOS
Most common endocrine/metabolic disorder effect women during their reproductive years.There is significant heterogeneity of presentation
Symptoms include ( menstrual irregularity, features of hyperandroginsm, fertility problem, obesity & psychological issues).
prevalence of PCOS varies 4% to as high as 26%.
(different clinic: infertility, gynaecology, dermatology, endocrine& dietician clinic)
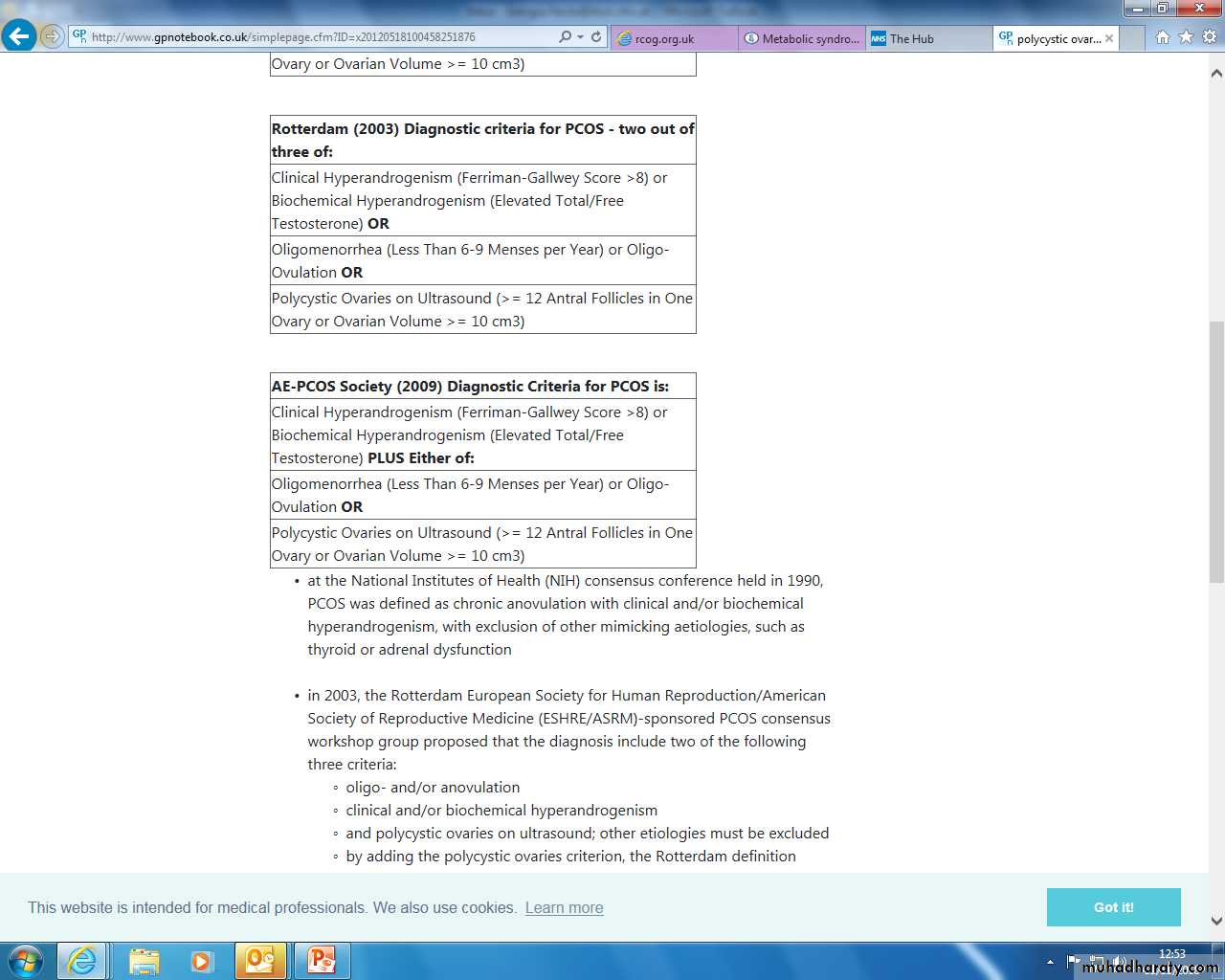
Diagnosis
Rotterdam consensus criteria:It is diagnosis of exclusion : thyroid disease, hyperprolactineamia, congenital adrenal hyperplasia, Cushing syndrome, androgen secreting tumour, hypothalamic pituitary ovarian dysfunction causing menstrual irregularity.
Pathophysiology of PCOS
Gonadotropin secretion and action: change in GNRH pusitality preferred LH production so LH/FSH ratio ↑, LH + ovarian theca cell secrete androgen, FSH paucity prevent + of aromatase activity with in granulosa cell for conversion of androgen to estradiol.Insulin secretion and action: insulin resistance, compensatory hyperinsulinemia, decrease insulin sensetivity appears to be due to a postbinding abnormality in insulin receptor-mediated signal transduction. Insulin is a potent stimulant for androgen secretion by the ovary, and suppress SHBG.
Pathophysiology of pcos
Weight and energy regulation: obesity worsens insulin resistance, the severity of ovulatory and menstrual dysfunction, and pregnancy outcome, increasing prevalence of metabolic syndrome, glucose intolerance, cardiovascular risk factors, and sleep apnea.Androgen biosynthesis and action:ovarian hyperandrogenism. insulin resistance,genetic predisposition to hyperandrogenism .insulin and LH+ ovarian theca cell androgen production (testosterone, and androstendione 70-80%) and( DHEAS in 25-65%), in turn androsendione lead to increase level of esterone through periphral conversion of androgen to estrogen. esterone have feed back effect on anterior pituitary gland lead to increased level of prolactin hormone.
• Sex hormone binding globulin- women with PCOS display decrease level of SHBG which is suppressed by insulin and androgen, thus less circulating androgen is bound, and available to end organ, so total testosterone is normal level and patient clinically hyperandrognic.
Investigations
Basal (day 2-5) LH, FSH Normally premenopausal LH:FSH is 1:1. In PCOS it may be >2:1 or >3:1.FSH (2-8)
LH (2-10)
AMH: increased.
TFT TSH 0.5-5IU/L, prolactin less500mU/L and testosterone
The recommended baseline biochemical test for hyperandrogenism is free androgen index (total testosterone divided by sex hormone binding globulin [SHBG] x 100).
Total testosterone(0.5-1.8nmol/l), if >5 so measurement of other androgens.
FAI < 5
SHBG(16-119nmol/l)
17-hydroxyprogesterone should be measured in the follicular phase and will be raised in CAH.Serum is drawn in morning fasting patient≥ 200ng/dl.
ACTH stimulation test synthetic ACTH 250µg iv and serum 17-HP measured after 1 hr. if more than 1000ng/dl is dx. Of late onset of CAH.
• Fasting insulin less 30 Mu/l: not routinely measured insulin resistant assessed by GTT
• DHEAS is produced exclusively by the adrenal gland, serum above 700mg/dl, highly suggestive for the presence of adrenal neoplasm. Adrenal imaging with CT or MRI is indicated for any patient with increase this level.
• Serum cortisol
• Endometrial sampling Is recommended in women older than 35 with abnormal uterine bleeding or younger women with an ovulatory bleeding refractory to hormonal medication.
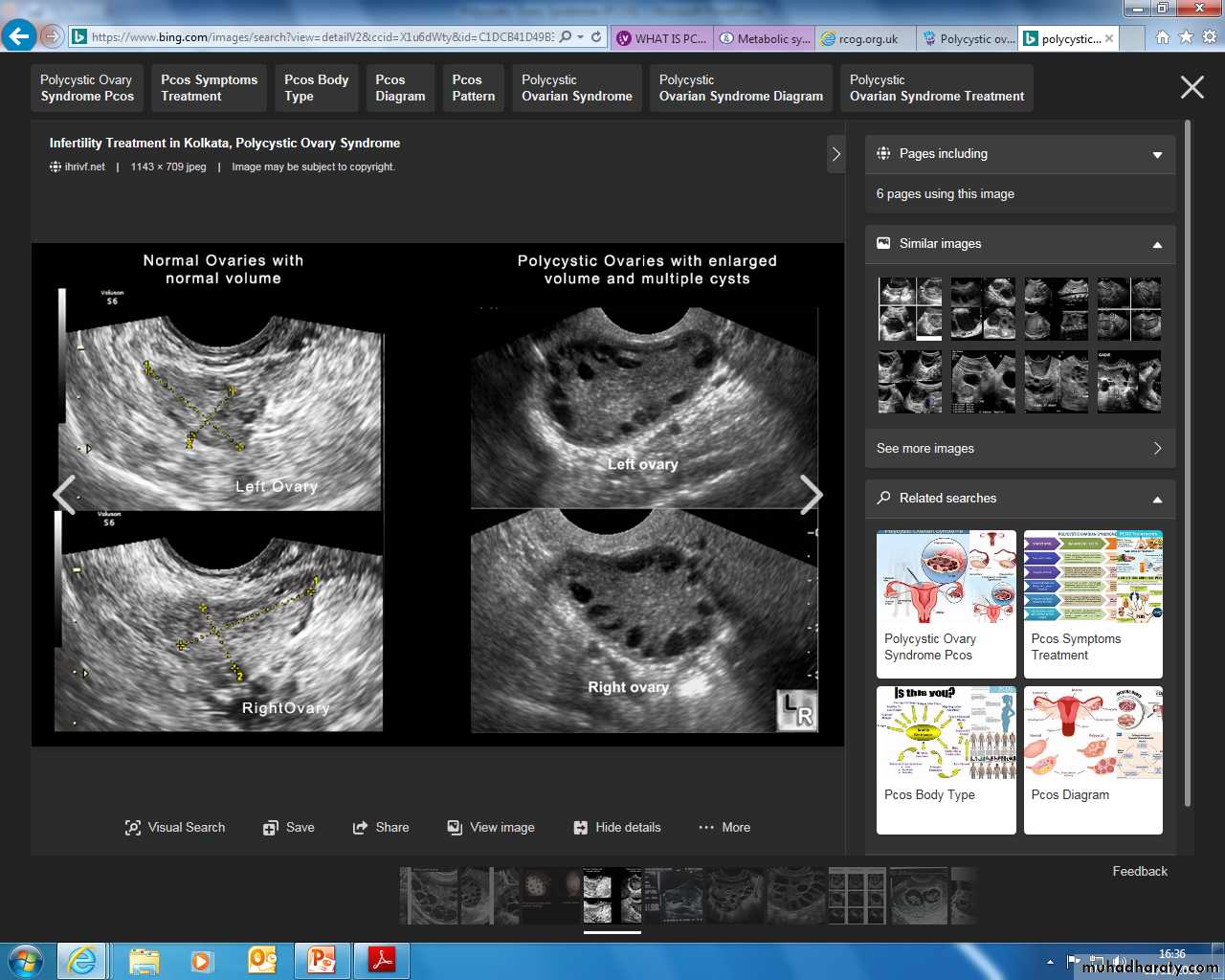
Imaging
Transvaginal ultrasound scan12 or more follicles
increased ovarian size (>10 cc): less sensitive than the follicle number criteria, but has a role when image resolution does not allow accurate follicle count, e.g. trans abdominal scanning, older equipment
Other morphological features include:
hyper echoic central stroma
peripheral location of follicles: which can give a string of pearl appearance
follicles of similar size measuring 2-9 mm
The presence of a single multifollicular ovary is sufficient to provide the sonographic criterion for PCOS
Ovaries may be normal
Management of pcospsychological support &quality of lifeHRQoL= multidimensional(cosmetic issue for excessive hair growth, weight issue, infertility that cause tension in families)obesityIt worsen both symptoms & endocrine profile (BMI>3o) caloric restriction & exercise (reduce glycemic load ;lower sugar content, more complex CHO & avoid fatty diet)30 minute brisk exercise/ day to maintain health.60-90 minute brisk exercise/day for weight lose.Bariatric surgery is indicated if: BMI>40BMI 30-35 with co-morbidities such diabetes.
Management of PCOS
Menstrual irregularityLow dose of cocp artificial cycle regular endometrial shedding .lipid friendly cocp 3rd generation.
With drawl bleeding with progestogens for12 days every 1-3 months or insertion of mirena.
Un ovulatory cycle (unopposed E stimulation of endometrium hyperplasia, irregular V.B= ET>10 mm= shedding & sampling required
Hyper androgenism & hirsutism
Cosmetic & medical therapy
Cosmetic(electrolysis ,waxing, bleaching laser, photothermolysis)
Drug take≥ 6-9 months
Eflornithine (Vaniqua) topical treatment, inhibit enzyme in hair follicle.
Cocp (Dianette) reduce sebum excretion 2-3 months= clinical improvement of acne 4-6 months.
Spironalactone 25-100mg/day
Other anti androgen (ketoconazole, finastride, flutamide)
Infertility in PCOS
80-90%Weight loss before treatment for ovarian stimulation
LH high specially in slim so ↓conception &↑miscarriage
Antiestrogen CC first line therapy.
Gonadotropin therapy
Ovulation triggered with HCG
Surgical ovulation induction
Pregnancy outcomes increase miscarriage, gestational diabetes, PIH, PE, preterm birth, admission to NCU, mortality, multiple birth.
Long term consequences
Cardiovascular diseaseType 2 diabetes
Obesity
Metabolic syndrome
Endometrial Ca
Psychological distress
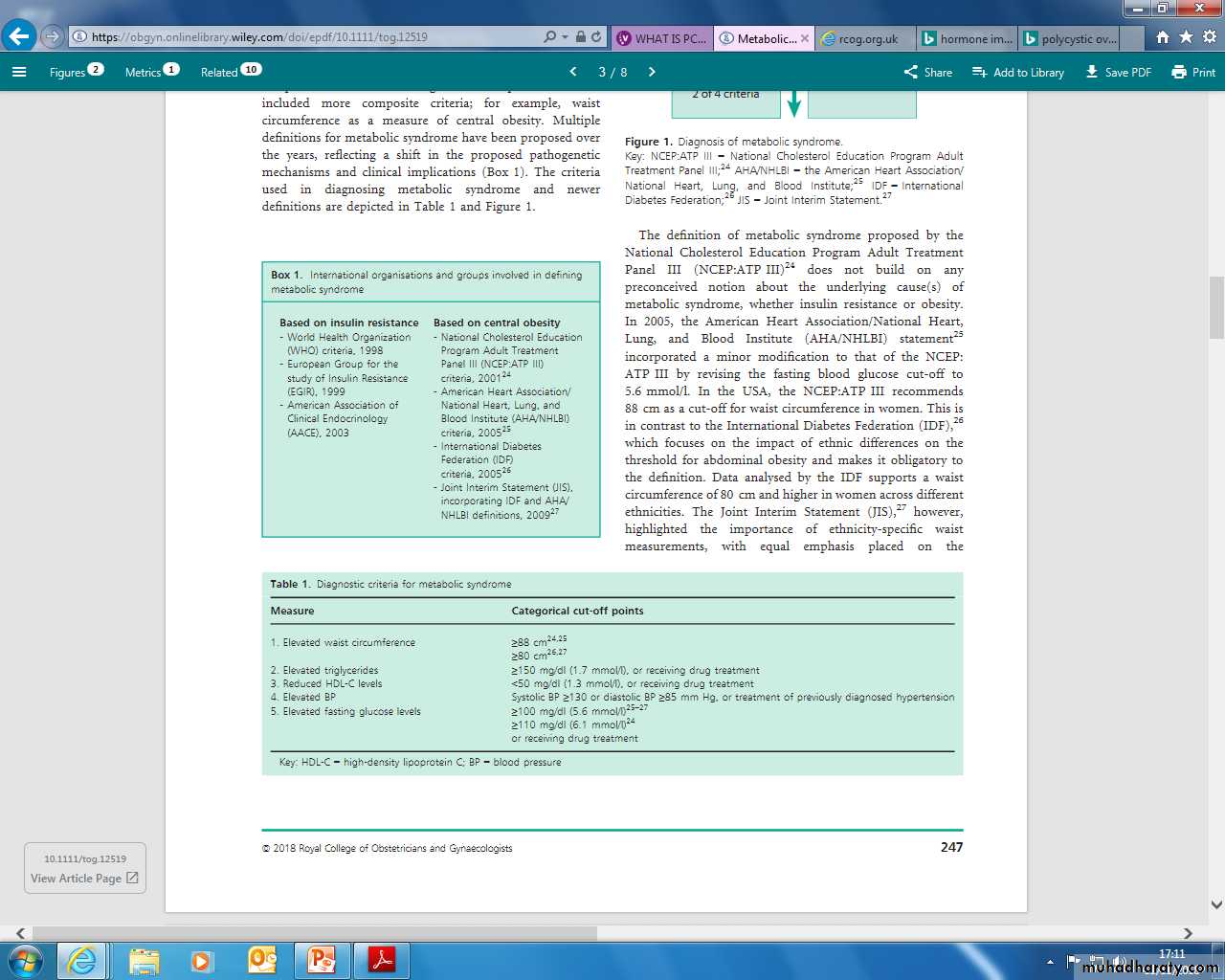
Metabolic syndrome
Up to 1/3 of women with PCOSk.k by insulin resistance. Obesity, atherogencdyslipidemia and hypertention. It↑ risk of CV disease,.
(myocardial infarction, left ventricular dysfunction and external carotid artery stiffness, atherosclerosis).
Metabolic syndrome
Insulin resistanceparadoxical insulin sensitivity patterns seen in different tissues (resistance in peripheral tissues and retained sensitivity in the ovarian cortex)
unclear whether the association is causal, propagative or merely co-existential
Atherogenic dyslipidaemia
* PCOS is associated with chronic low‐grade systemic inflammation, which mediates insulin resistance and accelerates atherogenesis
Insulin resistance
Free fatty acids
Fat tissue
LIVER
Very-low density lipoprotein (VLDL)
↑ triglycerides ↑ apolipoprotein B ↓ HDL
Obesity
HyperinsulinaemiaIncreased responsiveness of the ovarian theca to insulin
↑ Levels of free androgens
PCOS
dyslipidaemiaHypertension
potentiation of sympathetic outflow and the renin–angiotensin–aldosterone systemincreased levels of insulin and free fatty acids
vascular endothelial dysfunction also contributes to the development of hypertension
Consequences
Cardiovascular disease:
PCOS = double risk coronary heart disease and stroke
metabolic syndrome = 3 – 6 x more likely to develop CHD, with a 12% increase in mortality
Diabetes
PCOSbaseline normoglycaemia increased risk of developing impaired glucose tolerance (IGT)
up to 16% of women with PCOS convert to IGT / year
IGT have a 2% risk of progressing to diabetes type II / year
>6 years this risk maybe as high as 54%.
three‐fold increase in risk for gestational diabetes
Metabolic syndrome confers a five‐fold increase in risk for diabetes type II
Consequences
Cancer:PCOS Increased risk endometrial Ca (OR 2.89)
Metabolic syndrome associated with an increased risk of endometrial cancer (OR 1.6) and a higher incidence of pancreatic, postmenopausal breast and colorectal cancers (OR 1.5). Poorer cancer outcomes, increased recurrences and overall mortality.
Obstructive Sleep apnoea
PCOS is associated with up to a 30x higher risk, 9x increase in excessive daytime sleepinessInsulin resistance is a principal predictor for the risk of OSA. The presence of OSA in metabolic syndrome in turn worsens insulin resistance and cardiovascular outcomes.
Consequences
Psychological
PCOS depression increased incidence (OR 4.03) and increased severity of symptoms (independent of BMI)
Metabolic syndrome is associated with depression, mainly with neurovegetative features such as fatigue
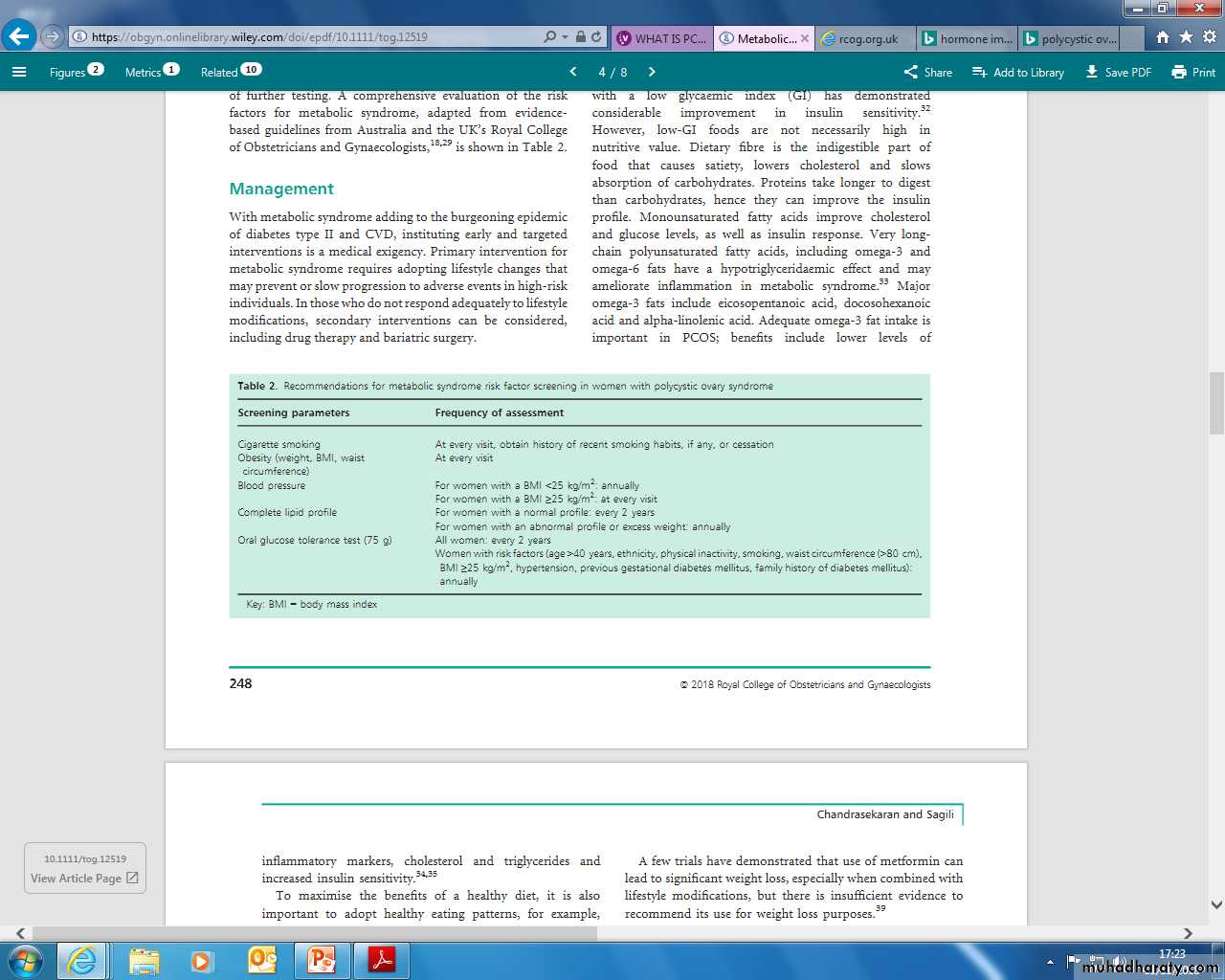
Management
Primary intervention for metabolic syndrome requires adopting lifestyle changes that may prevent or slow progression to adverse eventssecondary interventions can be considered, including drug therapy and bariatric surgery
Screening
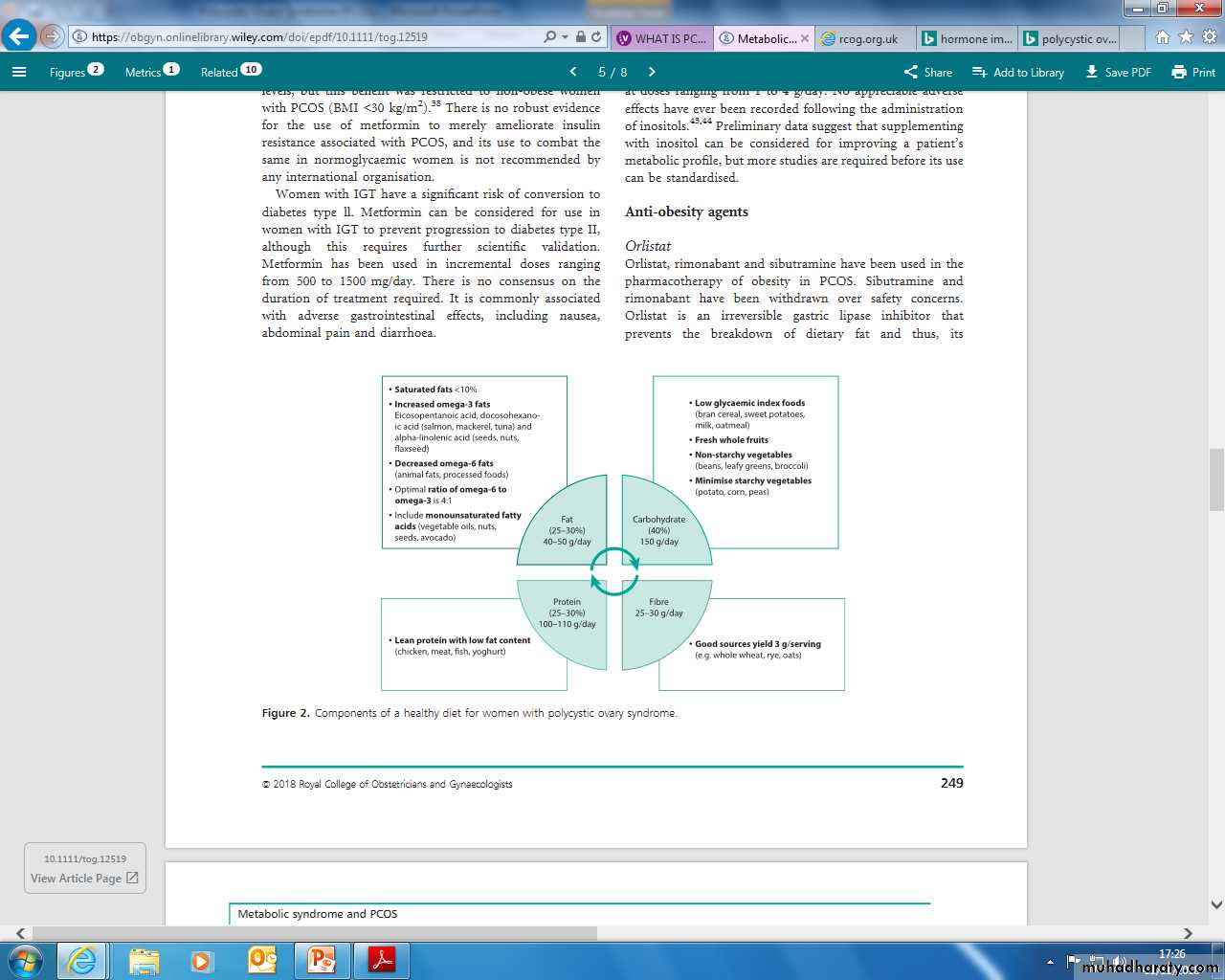
Lifestyle
Exercise and weight lossaim to lose 5–10% of their body weight in the first year after diagnosis for improved clinical outcomes
metabolically active visceral fat
insulin resistance + optimised lipid profile
psychological benefits such as reduced anxiety and depression
Pharmacological
Insulin sensitising agents:Metformin
Inositol
Anti-obesity agents:
OrlistatLiraglutide
• Although PCOS is treatable & the symptoms can be managed, but can not be cured.
• Long term consequence.
Any Questions?
References:
An evidence based text for MRCOGMetabolic syndrome in women with polycystic ovary syndrome https://doi.org/10.1111/tog.12519
Green Top guideline
RCOG (2016) Long-term consequences of polycystic ovary syndrome.
https://www.verity-pcos.org.uk/