Liver and biliary diseases
Introduction:Liver
- Liver is the largest & heaviest internal organ in the body (1500gm).
- Liver is the master of metabolism, it's involved with almost all the biochemical pathways that allow growth, fight disease, supply nutrients, provide energy & aid reproduction.
- Liver cells (hepatocyte) go thousands of complex biochemical reactions every second in order to perform these function.
In brief, you can't live without liver
Anatomy:
- The liver is located behind the lower ribs, right below diaphragm on right side of abdomen separated superiorly by falciform ligament & inferiorly by ligamentum teres.N.B. - Right lobe is much larger & has 2 additional lobes –(caudate & quadrate lobe).
Histology:
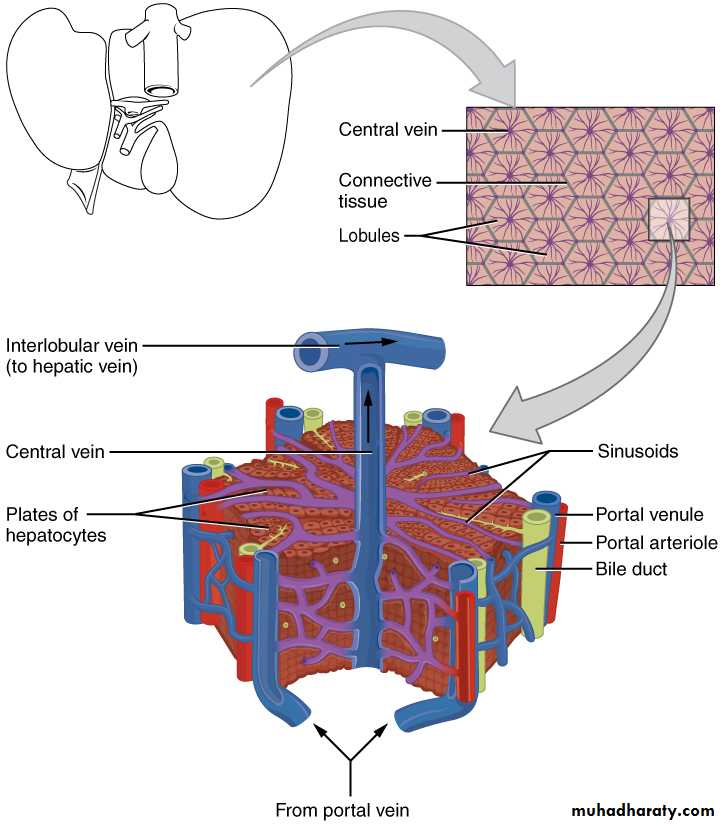
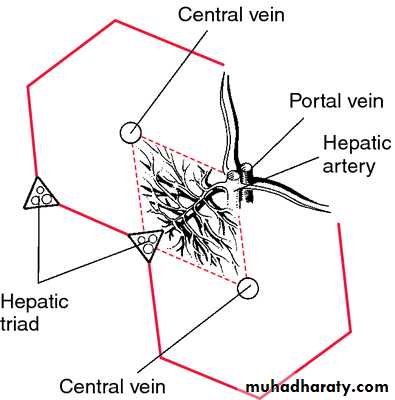
Hepatic lobule: is the basic unit for liver function:
The function unit of the liver is the hepatic acinus which is anatomically almost the reverse of the hepatic lobule.
N.B: The walls of the sinusoids consist of endothelial & macrophage cells known as "Kupffer cells"
- These kupffer cells phagocytose damaged & aging RBCs, bacteia, viruses & immune complexes
Blood Supply of i liver:
- Liver has double bl. Supply-hepatic artery carries1/3 of blood supply brining oxygenated blood from aorta.
-Portal vein 2/3 of blood supply brining blood from the
Intestine and spleen.
Venous drainage:
Drainage is via the hepatic veins into the inferior vena cava.
Liver function: -
The liver is the main industrial centre of the body.
- Liver is very important in metabolized protein, carbohydrate & fat metabolism.
- Making bile.
- Detoxification: filtering of i blood.
N.B: The liver has great reserve power, it using only a small amount of its full potential, it can loss 3 /4 its cells before it stopping function.
So, this great reserve power means that diseases that affect the liver show no symptoms in early stages, & this makes the prognosis worse.
N.B: Liver cells can regenerate themselves, this regenerative ability allows the diseased liver to return to normal function in some cases. Very few organs in the body have this ability.
So, the first lines in Many patients with (any liver diseases) are a symptomatic, for years, others may show generalized weakness, anorexia, malaise & weight loss.
investigation of hepatobiliary disease
Aims of investigations in patients with suspected liver diseaseDetect hepatic abnormality.
Measure the severity of liver damage.
Detect the structural effects on the liver.
Identify the specific causes.
Investigate possible complications
1) Detect hepatic abnormality
Liver function tests
Liver function tests (LFTs) include the measurement of serum bilirubin(direct and indirect) , aminotransferase(ALT and AST), alkaline phosphatase, gamma-glutamyl transferase(GGT) ,albumin and Prothrombin time (PT)
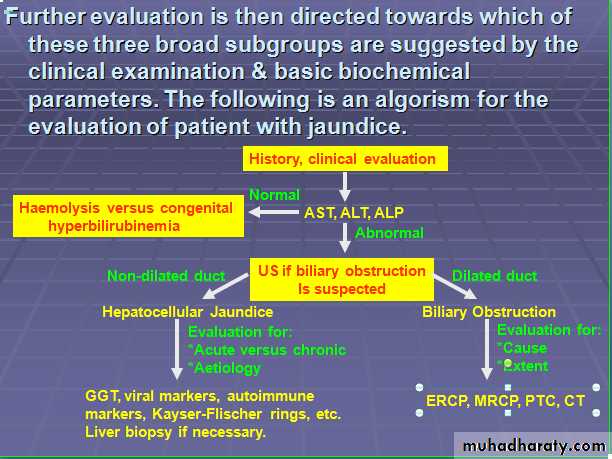
Bilirubin
hyperbilirubinemia results from the accumulation of bilirubin—a product of hem metabolism—in the body tissues and may be due to abnormalities in the formation, transport, metabolism, and excretion of bilirubin. Total serum bilirubin is normally 0.2–1.2 mg/dL (mean levels are higher in men than women and higher in whites and Hispanics than blacks), and jaundice may not be recognizable until levels are about 3 mg/dL. Unconjegated hyperbilirubinemia may result from overproduction of bilirubin while conjugated hyperbilirubinemia may result from impaired excretion of bilirubin from the liverAminotransferases
These enzymes (often referred to as transaminases) are present in hepatocytes and leak into the blood with liver cell damage. Two enzymes are measured:
Aspartate aminotransferase (AST) is primarily a mitochondrial enzyme (80%; 20% in cytoplasm) and is also present in heart, muscle, kidney and brain. High levels are seen in hepatic necrosis, myocardial infarction, muscle injury and congestive cardiac failure.
Alanine aminotransferase (ALT) is a cytosol enzyme, more specific to the liver so that a rise only occurs with liver disease. .
Alkaline phosphatase (ALP)
This is present in the canalicular and sinusoidal membranes of the liver, but is also present in many other tissues, such as bone, intestine and placentaALP enzymes in the liver are located in cell membranes of the hepatic sinusoids and the biliary canaliculi. Accordingly, levels rise with intrahepatic and extrahepatic biliary obstruction and with sinusoidal obstruction, as occurs in infiltrative liver disease
Gama-Glutamyl transpeptidase
This is a microsomal enzyme Mild elevation of the γ-GT is common even with a small alcohol consumption and does not necessarily indicate liver disease if the other liver biochemical tests are normal. In cholestasis the γ-GT rises in parallel with the ALP as it has a similar pathway of excretion.The pattern of a modest increase in aminotransferase activity and large increases in ALP and GGT activity favours biliary obstruction and is commonly described as 'cholestatic' or 'obstructive' .Isolated elevation of the serum GGT is relatively common, and may occur during ingestion of microsomal enzyme-inducing drugs including alcohol.
Pattern
AST/ALTGGT
ALP
Biliary obstruction
↑
↑↑
↑↑↑
Hepatitis
↑↑↑
↑
↑
Alcohol/enzyme-inducing drugs
N/↑
↑↑
N
'Hepatitic' and 'cholestatic'/'obstructive' LFTs
Haematological tests
Routine haematological investigations are often abnormal in patients with liver diseases and can give a clue to the underlying diagnosis:A normochromic normocytic anaemia may reflect recent gastrointestinal haemorrhage, where as chronic blood loss is characterised by a hypochromic microcytic anaemia secondary to iron deficiency. A high erythrocyte mean cell volume (macrocytosis) is associated with alcohol misuse, but target cells in any jaundiced patient also result in a macrocytosis.
Leucopenia may complicate portal hypertension and hypersplenism, whereas leucocytosis may occur with cholangitis, alcoholic hepatitis and hepatic abscesses. Atypical lymphocytes are seen in infectious mononucleosis, which may be complicated by an acute hepatitis.
Thrombocytopenia is common in cirrhosis and is due to reduced platelet production, and increased breakdown because of hypersplenism. Thrombocytosis is unusual in patients with liver disease but may occur in those with active gastrointestinal haemorrhage and, rarely, in association with hepatocellular carcinoma
2)-Measure the severity of liver damage.
Serum albuminThis is a marker of synthetic function and is a valuable guide to the severity of chronic liver disease. A falling serum albumin in liver disease is a bad prognostic sign. In acute liver disease initial albumin levels may be normal.
Prothrombin time (PT)
This is also a marker of synthetic function. Because of its short half-life, it is a sensitive indicator of both acute and chronic liver disease. Vitamin K deficiency should be excluded as the cause of a prolonged PT by giving an intravenous bolus (10 mg) of vitamin K. Vitamin K deficiency commonly occurs in biliary obstruction, as the low intestinal concentration of bile salts results in poor absorption of vitamin K
bilirubin
The degree of elevation of bilirubin also reflects the degree of liver damage.
3)-Detect the structural effects on the liver.
Imaging techniquesUltrasound examination
This is a non-invasive, safe and relatively cheap technique. The normal liver appears as a relatively homogeneous structure. The gall bladder, common bile duct, pancreas, portal vein and other structures in the abdomen can be visualized. Abdominal ultrasound is useful in:
lymph node enlargement
a jaundiced patient detect whether intra- or extra biliary duct dilation .
hepatomegaly/splenomegaly .
the detection of gallstones .
focal liver disease - lesions > 1 cm.
general parenchymal liver disease .
assessing portal and hepatic vein patency.
It is good at identifying liver abnormalities such as cysts and tumours and pancreatic masses
and fluid collections,
but visualization of the lower common bileduct and pancreas is often hindered by overlying bowel gas.
Computed tomography (CT) examination
This technique is complementary to ultrasound, which should usually be performed first. It provides excellent visualization of the liver, pancreas, spleen, lymph nodes and lesions in the porta hepatis. CT allows assessment of the size, shape and density of the liver and can characterize focal lesions in terms of their vascularity.Magnetic resonance imaging (MRI)
MRI produces cross-sectional images in any plane within the body. MRI is probably the most sensitive investigation of focal liver disease.. Contrast agents such as intravenous gadolinium allow further characterization of lesions, and are suitable for those with iodine allergy and provide angiography and venography of the splanchnic circulation.Magnetic resonance cholangiopancreatography (MRCP)
This technique involves the manipulation of a volume of data acquired by MRI. A heavily T2-weighted sequence enhances visualization of the 'water-filled' bile ducts and pancreatic ducts to produce high-quality images of ductal anatomy. This non-invasive technique is replacing diagnostic (but not therapeutic) ERCP .Plain X-rays of the abdomen
Plain radiography has a limited role in the investigation ofhepatobiliary disease. Chest radiography may show small
amounts of subphrenic gas, abnormalities of diaphragmatic
contour, and related pulmonary disease, including metastases
These are rarely requested but may show:
gallstones - 10% contain enough calcium to be seen
air in the biliary tree owing to its recent instrumentation, surgery or to a fistula between the intestine and the gall bladder
pancreatic calcification
rarely, calcification of the gall bladder (porcelain gall bladder).
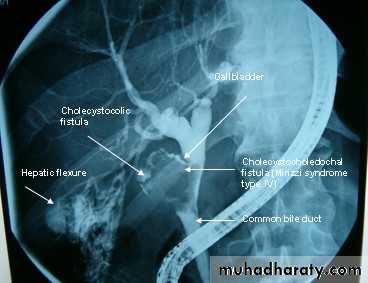
Cholecystogram
Cholecytogram is an x-ray procedure used to help evaluation the gallbladder where special diet is consumed prior to the test and contrast tablets are also swallowed to help visualize by x-ray. This test is used to help in diagnosing disorders of liver and gallbladder, including gallstones and tumors. This test is rarely required as it has been almost universally replaced by ultrasound but may be useful as a test of gall bladder function.Radionuclide imaging - scintiscanning
In a technetium-99m (99mTc) colloid scan, the colloid is injected intravenously to be taken up by the reticuloendothelial cells of the liver and spleen so detect any filling defects indicat abnormal liver tissues (tumor ,abscess or cyst).But In chronic liver disease there is poor intake in the liver and most of the colloid is taken up in the spleen and bone marrow. Ultrasound has largely replaced this technique.
Endoscopy
Upper GI endoscopy is used for the diagnosis and treatment of varices, for the detection of portal hypertensive gastropathy, and for associated lesions such as peptic ulcers.Endoscopic ultrasound (EUS)
In this technique, a small high-frequency ultrasound probe is mounted on the tip of an endoscope and placed by direct vision into the duodenum. The close proximity of the probe to the pancreas and biliary tree permits high-resolution ultrasound imaging.
1)-It allows accurate staging of small, potentially operable, pancreatic tumours and
2)- offers a less-invasive method for bile duct imaging.
3)- It has a high accuracy in detection of small neuroendocrine tumours of the pancreas.
4)- EUS-guided fine-needle aspiration of tumours provides.
Percutaneous transhepatic cholangiography (PTC)
Under a local anaesthetic, a fine flexible needle is passed into the liver. Contrast is injected slowly until a biliary radicle is identified. Now this test rarly used due to high risks of bleeding, cholangitis and septicemia.Endoscopic retrograde cholangiopancreato-
graphy (ERCP)This technique is used to outline the biliary and pancreatic ducts. It involves the passage of an endoscope into the second part of the duodenum and cannulation of the ampulla. Contrast is injected into biliary systems and the patient is screened radio logically. diagnostic and therapeutic procedures can be carried out: like biliary stone removal , CBD stenting or biopsy taken.
4)-Identify the specific cause
Diagnosis Initial test AdditionalChronic hepatitis B HBsAg HBeAg, HBeAb
Chronic hepatitis C HCV antibody HCV-RNA
Primary biliary cirrhosis AMA Liver biopsy
Primary sclerosing MRCP ANCA
cholangitis
Autoimmune hepatitis ASMA, ANA, LKM, Liver biopsy
immunoglobulin
Haemochromatosis Transferrin saturation, HFE gene test
ferritin
Wilson's disease Caeruloplasmin 24-hr urinary copper
α1-antitrypsin α1-antitrypsin level α1-antitrypsin genotype
Drug-induced liver disease LFTs Liver biopsy
Coeliac disease Endomysial antibody Small bowel biopsy
5)-Investigation of complications of hepatic cirrhosis.
hepatic encephalopathyinvestigation for any precipitating cause.
Psychometric test.
Electroencephalogram (EEG).
Sensory evoked potentials.
Portal hypertension
Upper GI endoscopy
Barium swallow and meal.
Liver ultrasound.
Abdominal CT.
Wedged hepatic venous pressure.
Venography of hepatic veins
Ascites
Ascetic fluid sampling.
Liver ultrasound.
Laproscopy.
Renal failure Urine analysis.
Renal ultrasound.
Central venous pressure recording.Renal biopsy.
Hepatocelluler CA
Alpha_fetoprotein.
Liver ultrasound.
Abdominal CT.
Hepatic angiogram.
Laproscopy.