ACUTE KIDNEY INJURY
defined as any of the following (Not Graded):
•
Increase in SERUM CREATININE by X0.3 mg/dl within 48
hours; or
•
Increase in SCr to X1.5 times baseline, which is known or
presumed to have occurred within the prior 7 days; or
•
Urine volume 0.5 ml/kg/h for 6 hours.
•
IF u FIND ANY OF THESE U NEED THEN TO GO FOR
STAGING OF THE KIDNEY INJURY
•
IF THE PATIENT HAS A MEDICAL RECORDS THAT POINT TO
A PREVIOUS KIDNEY AFFECTION ( CHRONIC KIDNEY
DISEASE AND NOW THERE IS MORE ELEVATION IN THE
READINGS WE WILL SAY ITS AN ACUTE ON CHRONIC
INSULT

Acute Kidney Injury stages (RIFLE CRITERIA)
R= risk S.Creatinine >1.5 times normal or GFR
decreased > 25%
I= injury S. Creatinine >2 times normal or GFR
reduction > 50%
F failure stage S. creatinine > 3 times normal or GFR
reduction > 75% or serum creatinine >= 4 mg /dl.
L= loss of function 4 weeks of failure stage.
E= end stage 3 months of failure.

AKIN criteria for AKI
•
Stage 1 Uop < 0.5 ml/kg/h………..6 hours
•
Stage 2 Uop < 0.5ml/kg/h…………12 hours
•
Stage 3 Uop <0.3ml/kg/hour for24 hours or
anuric for 12 hours.
•
Usually patients are asymptomatic but they may
present as renal failure features
Acute renal failure
•
Sudden and usually reversible loss of renal function developing over days
to weeks and usually accompanied by reduced urinary output.
•
Causes:
I.
Prerenal : the disease process acts before the kidney and leads to
reduction in blood perfusion to the kidney( heart failure, bleeding overt
or concealed as in pregnant uterus or femur fracture or large muscle
trauma or crush injury, burn, inflammatory skin disease with oozing of
large amount of fluid, dehydration, septic shock, renal artery stenosis or
occlusion by thrombus, polycythemia, hepatic cirrhosis= hepatorenal
syndrome, nephrotic syndrome due to depleted vascular
compartment.) if these hemodinamically mediated causes are not
corrected they will lead to acute tubular necrosis
II. Renal ( the disease process within the kidney )
1. In glomerulus…….. Glomerulonephritis (5%)
2. In tubules…….. Acute tubular necrosis the (hypoxic/toxic/ septic) (85%).
3. Interstitium…… interstitial disease Leading to Interstitial nephritis
(10%).
III. post renal ( obstruction…. Stone, tumor, prostatic enlargement )
Pre renal ARF
If prerenal causes are not corrected quickly before autoregulation of
the kidney failed, there will be hypoxia and decreased perfusion of the
renal tubules and damage of them and acute tubular necrosis will be
established (ex dehydration and bleeding if not corrected).
Autoregulation: ability of the kidney to deal with decreased perfusion
so that tissue injury due to hypoxia will not happen & it involves:
•
Afferent v.( vessels entering the glomerulus) dilation usually through
prostaglandin release ( inhibited by NSAID, so the latters are risky in
dehydrated patients even before hypotension develop)
•
Efferent v. ( vessels leaving the glomerulus) vasoconstriction this is
mediated by angiotensin II and renin( inhibited by ACI inhibitors as
captopril) and so the latters are risky in dehydrate and any volume
depleted individual.)
Autoregulation will fail below 80 and above 150 mmhg systemic
systolic blood pressure.( severe hypertension leads to severe spasm of
vascular beds involving the kidney consequently leads to decrease renal
perfusion). If the cause not corrected, autoregulation will fail and acute
renal failure become established due to acute tubular necrosis.
ACUTE tubular necrosis
•
Etiology and Pathogenesis
•
Ischemic-ATN
pre renal causes if not corrected rapidly ischaemia and death of
the tubules happen, because, autoregulation will fail which is
between 80-150. in elderly and chronic kidney disease regulation
may fail even at 100 mmhg . ACEIs & NSAIDs cause efferent
dilation and prostaglandin inhibition respectively thereby
impairing autoregulation and preferably not to be given in
vascularily depleted and hypotensive patients because they will
impair autoregulation and cause injury.
•
There is release of vasoconstrictors as indothelin I, Thrombxane
A2….
•
There is tubuloglomerular feedback: damaged tubule leads to
vasoconstriction and decrease glomerular filtration rate this will
prevent sodium delivery to tubules and lessen the damage
Nephrotoxic ATN
caused by toxic substance as drugs or bacterial toxins as in
sepsis
•
3 phases of ATN pathogenesis , initiation phase and
maintenance and recovery phase… the tubular cell start to
recover and regenerate .recovery usually happen in 2-3
weeks.
•
The duration of recovery phase will depend on the severity
an duration of the causative insult.
•
ATN clinically can be
clinical scenarios:
•
Oliguric due to decrease perfusion or obstruction by the
sheded dead tubular cells into tubular lumen then polyuric
---polyuria is due to loss of medullary concentration
gradient) this phase usually occur in prerenal causes,
•
non oliguric as in aminoglycoside nephrotoxicity
•
Differential diagnosis of established acute renal failure in a
haemodynamically stable ( normal blood pressure profiles) ,
non-septic patient
1. Urinary tract obstruction
Suggested by a history of loin pain, haematuria, renal colic or
difficulty in micturition but often clinically silent
•
Can usually be excluded by renal ultrasound: essential in any
patient with unexplained ARF
•
Prompt relief of the obstruction restores renal function
2. Drugs and toxin
theraputics ( NSAIDs, ACEI through disturbances in kidney
dynamics) or direct tubular toxicity as aminoglycosides
Auto-toxins: rhabdomyolysis releasing myoglobin; myeloma cast
nephropathy
Poisoning, e.g. paraphenylenediamine hair dye, mushrooms,
snake bite, paracetamol

3 . Vascular event
Due to major vascular occlusion ( renal artery thrombus) or small-
vessel diseases notably malignant hypertension and haemolytic uraemic
syndrome/thrombotic thrombocytopenic purpura
•
May be precipitated by ACE inhibitors in critical renal artery stenosis
•
Urine usually shows minimal abnormalities but there may be
haematuria in renal infarction
4. Rapidly progressive glomerulonephritis (RPGN)
•
Typically, significant (dipsticks 3+) haematuria and minor proteinuria
(often with red cell casts ( protinacious substance with RBC embedded
in ) or 'glomerular' red cells ( destructed RBCs)
•
Sometimes associated with systemic features (e.g. systemic vasculitis,
systemic lupus erythematosus (SLE), Goodpasture's (anti-GBM)
disease)
•
Useful blood tests include: antineutrophil cytoplasmic antibodies
(ANCA), antinuclear antibodies (ANA), anti-GBM antibodies,
complement ( C3 & C4, CH50complement), immunoglobulins
•
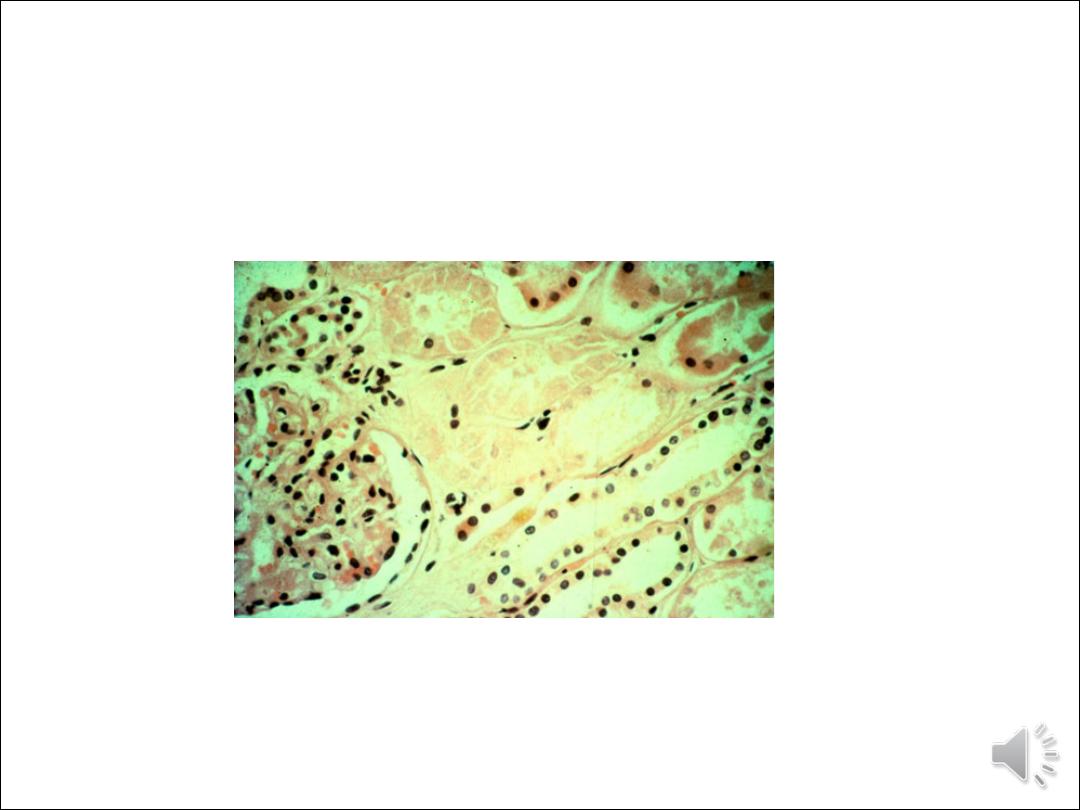
Renal biopsy shows aggressive glomerular inflammation, usually with
crescent formation ( proliferation of epithelial cells).
5. Acute interstitial nephritis
Usually caused by an adverse drug reaction but can be
due to an infection ( bacteria or viral).
•
Characterised by small amounts of blood and protein
in urine, often with leucocyturia sterile pyuria ( as +++
WBC in urine with negative urine culture result).
•
Kidneys are normal size
•
Requires cessation of drug and often prednisolone
treatment 30 mg/day for 3 weeks.
•
Clinical feature of Acute renal failure
Symptoms ( uremia can cause almost any symptom)
1. Features of the underlying illness( heart failure), diarrhoea, fever in severe
infection and septic shock, burn, bleeding ex GIT bleed. Dizziness,
fainting, syncope, thirst, generalized tierdness. Decreased urine output in
prerenal or can be non oliguria in ATN. Obstructive features as rapid
reduction of urine output , severe loin pain= obstruction
Features of increased blood urea ( anorexia, nausea vomiting , disturb
consciousness (uremic encephalopathy) ,fits( cns hemorrhage,hypocalcemia,
sodium abnormality), tremor flabbing , increase respiratory rate & SOB),
fatigue and weakness with pallor, itching and ecchymosis and uremic frost
rare now adays , chest pain due to pericarditis or ischaemia, palpitation due
to arrythmia ( electrolyte disturbances and acidosis). Constipation or
diarrhoea ( uremic enteritis and colitis or due to ischemic bowel due to
accelerated atherosclerosis or arrythmia as AF)
signs
Signs of dehydration and decreased perfusion( early postural hypotension
…reduction in blood pressure > 20/10 from lying to standing …then supine
hypotension), tachycardia , dry mucus membranes, underfilling of capillary
beds, decreased JVP ( unless patient has heart failure)
1. Signs of the predisposing illness (ex increased JVP in heart failure)
•
CNS Assess consciousness by glasco coma scale,
neck stiffness, flapping tremor
•
Pallor and earthy color ( pallor + hyperpigmented
skin), leg oedema and hypertension due to oligurea
and continued water or IV fluid intake
•
Heart… pericardial rub
•
Chest… tachypenia, pleural rub ,effusion,
consolidation due to secondary pneumonia
•
Abdomen … distension due to ileus ( hyperkalemia,
uremic ileus) tender epigastrium due to peptic
ulceration, renal artery bruit due to renal artery
stenosis.
•
Leg odema

)
Investigations
1.
ECG to detect hyperkalemia( tent t wave to sign wave and asystole) and arrythmia.
2.
B urea if elevated > 30 mg/dl day …. Consider dialysis , S creatinine, ( cystatin C elevated earlier
than creatinine and can predict renal failure in hospital and RCU OR HDU settings
3.
Serum K ( normal elevated or rarely low), Na can be low if water intake continued with oligurea,
Ca ( decreased due to decrease 1,25 (OH)2 cholecalceferol production by the damaged kidney
,Po4 ( increased especially in hemolysis and rhabdomyolysis, and catabolic states),Mg & uric acid
are increased.
4.
Arterial blood gas analysis ( PH, Hco3,,PO2, Pco2).. acidosis
5.
Investigate according to the cause ex blood culture for septicemic patients
6.
Imaging study ( initially ultrasound to exclue obstrucion.. Postrenal) and to show renal size (
normal in acute RF and some causes of CRF as in DM, MM, amyloidosis, HIVAN, ADPCKD,tumors
of the kidney, obstructive uropathy).
7.
Urine Na < 20 mmol/l in pre renal because the kidney reabsorb it to increase the vasculr
compartment, FeNa < 1%, increase osmolality > 600 mOsmol/l)
8.
GUE to exclude RBC cast and proteinurea ( active sediment) .. Glomerulonephritis, WBC cast and
urine eosinophil to exlude interstitial nephritis and muddy brown cast to exclude acute tubular
necrosis
9.
Blood and urine toxicology survey
10. CBC AND ESR
11. Liver function testing
12. Viral hepatitis ( HBV- surface antigen & HCV antibody )
13. Renal biopsy if cause is unknown.
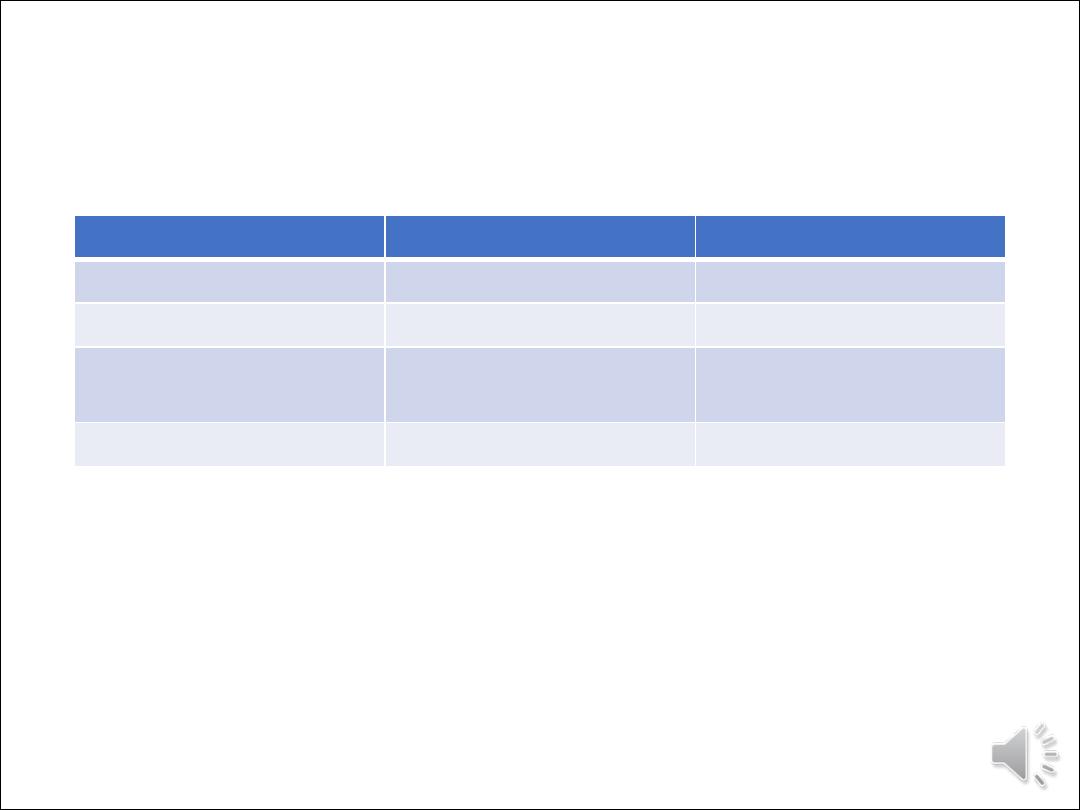
Difference between pre renal and
renal causes of acute renal failure
Renal
Prerenal
criteria
<350mosm/l
>600 mosm/l
Urine osmolality
>2%
<1%
FeNa
<40
>40
bloodUrea / serum
creatinine ratio
<1.3
>1.3
U/P osmol
Prevention of ARF ( easy on papers difficult in practice, adapted )
Hyperuricemia :- ( multiple myeloma, treatment of high burden
malignancy as very high WBC count in leukemia and chemotherapy to
large tumor mass as large lymph nodes in NHL = tumor lysis syndrome)
1. Hydration by normal saline to ensure 2-3 liter urine output.
2. Alkalization of urine by sodium bicarbonate infusion.
3. Zyloric( allopurinol) 300-900 mg day.
4. Rasburicase.
Contrast induced nephropathy ( cardiac catheterization, CT contrast
study…)
1. Normal saline infusion before procedure ( the most effective) or
2. Sodium bicarbonate infusion
3. NAC ( N-acetylecystiene )
4. High dose vitamin C .
5. Stop metformin.

•
Treatment in high dependency unit (ICU)
•
Correct underlying cause as hypovolemia or obstruction or glomerulonephritis
1
restore circulation with fluid that is lost in cases of hypovolemia as rapid as possible. (Ex blood, NS,
plasma)
2
Central venous line for central venous pressure monitoring which reflect blood volume
3
Correct acidosis and hyperkalemia ( 3
rd
stage important and pivotal issue)
4
Dopamine at low dose will not benefit to increase kidney perfusion
5
Dialysis ( hemodialysis or peritoneal dialysis)
6
Correction of underlying cause.
prognosis : if treatment given rapidly in pre renal ………………. Reversible
if delay happen renal failure become established ………..( Acute Tubular Necrosis, ATN)
Indications of dialysis in ARF
1.
Unresponsive fluid overload ( pulmonary oedema), hyperkalemia or metabolic acidosis unresponsive to
medical therapy.
2.
Pericarditis
3.
Uremic encephalopathy, convulsion
4.
Severe uremic symptoms ( nausea and vomiting).
5.
> 30 mg/day elevation in blood urea
