D. Usama Surgery
Fifth Stage
1
Anatomy of the thorax L1
Chest wall and pleura:
Beneath the skin and subcutaneous tissue, the chest wall is covered by the pectoralis muscles
anteriorly and the latissimus dorsi and serratus anterior muscles posterolaterally. In an anterior
thoracotomy, the fibers of the pectoralis major are split, exposing the intercostal muscles. In the
standard posterolateral thoracotomy, the latissimus dorsi is divided, and then the serratus anterior
is divided or split. From the standpoint of preservation of normal chest wall mechanics, an anterior
thoracotomy is usually better tolerated; however, exposure and control of intrathoracic structures
are often better accomplished through the posterolateral approach, which is the standard
thoracotomy incision.
There are 12 pairs of ribs, 7 of which are true ribs and 5 of which are false ribs. True ribs have
costal cartilage that directly articulates with the sternum. False ribs do not. The eleventh and
twelfth ribs are called floating ribs because they are not attached anteriorly
The sternum is divided into the manubrium, the body, and the xiphoid. The clavicle articulates
with the sternum and the first costal cartilage.
Muscles of the intercostal space are the external, internal, and transversus thoracic muscles. There
are 11 intercostal spaces. Each intercostal space contains a vein, an artery, and a nerve, which
course along the lower edge of the rib. All the intercostal spaces are wider anteriorly than
posteriorly, the widest being the third.
The lower border of the pectoralis major muscle forms the anterior axillary fold. The tendon of
the latissimus dorsi forms the posterior axillary fold .
The parietal pleura is divided into four parts: costal, cervical, diaphragmatic, and mediastinal. The
costal pleura lines the ribs, cartilages, and vertebral bodies and is the thickest portion of the
parietal pleura. The visceral pleura covers the lungs so firmly.
The intercostal neurovascular bundle:
In the plane between the innermost intercostal muscle and outer two layers (external and internal
intercostal muscles) runs the neurovascular bundle. From above downward the order is vein,
artery, and nerve (VAN). They are protected by the downward projection of the lower border of
the rib
The intercostal nerves:
Are mixed spinal nerves formed from a dorsal and a ventral root, the dorsal root being sensory
and the ventral root containing somatic motor neurons
D. Usama Surgery
Fifth Stage
2
The intercostal arteries:
Two sets of intercostal arteries, the posterior and the anterior, are responsible for supplying
the intercostal spaces
The posterior intercostal arteries are branches of the descending thoracic aorta except in
the first two spaces where they are branches of the supreme intercostal artery, given off by
the costocervical trunk of the second part of the subclavian artery.
The anterior intercostal arteries are branches of the internal thoracic arteries from the first
part of the subclavian artery
The anterior intercostal arteries are smaller than the posterior intercostal arteries with
which they anastomose
The intercostal veins:
In each space there is one posterior and two anterior intercostal veins
The anterior veins drain into the musculophrenic and internal thoracic veins.
The vein of the first space (called supreme intercostal vein), posteriorly, drains to the
brachiocephalic, vertebral, or superior intercostal vein.
The superior intercostal vein is formed by the posterior intercostal veins of the second,
third, and sometimes the fourth spaces. This drains into the azygos vein on the right side
and on the left side open into the left brachiocephalic veins
Lymphatic drainage of the chest wall:
There are three upgoing lymph channels on each side of the thoracic cavity, and they freely
communicate with each other.
They are the right and left parasternal, and bronchomediastinal trunks (alongside the trachea), the
thoracic duct, and the right lymphatic duct
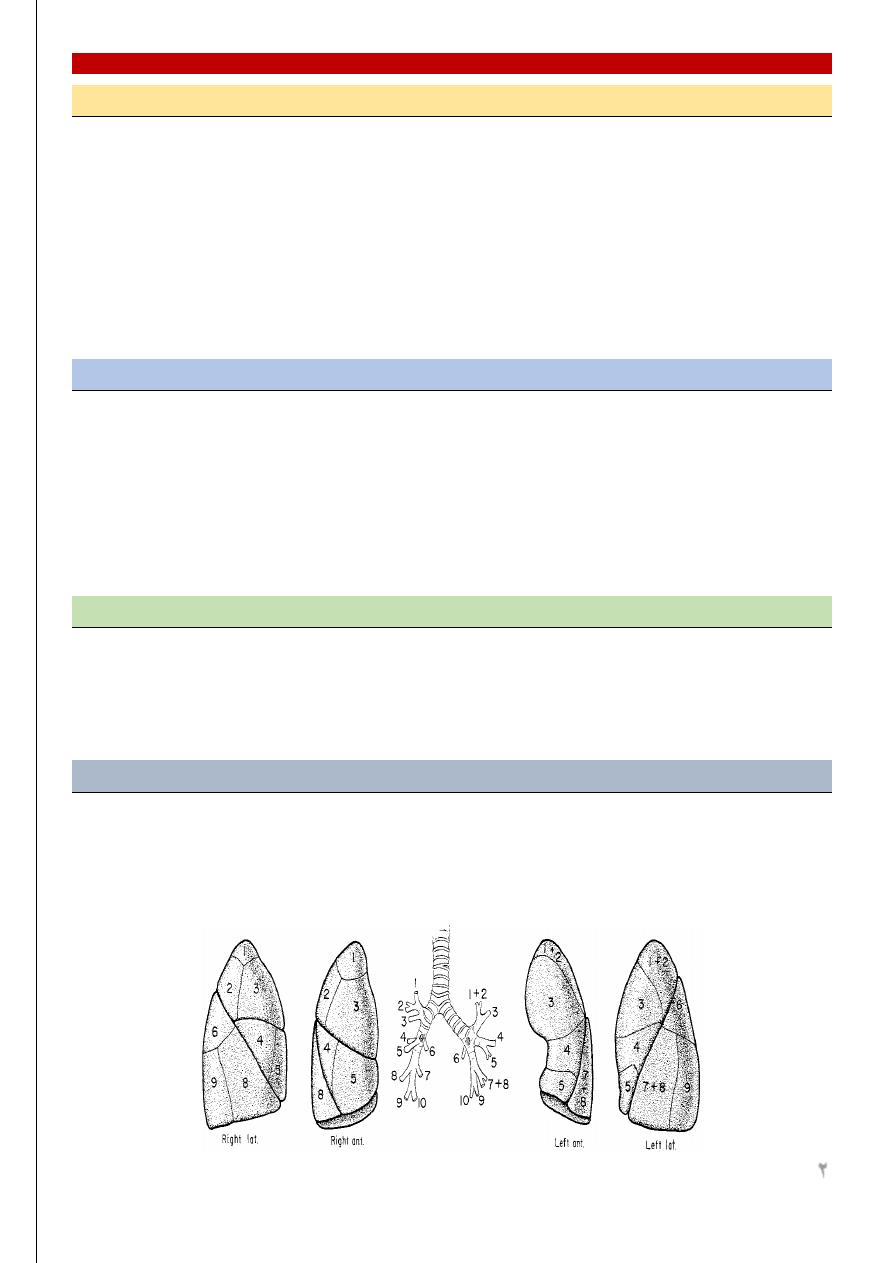
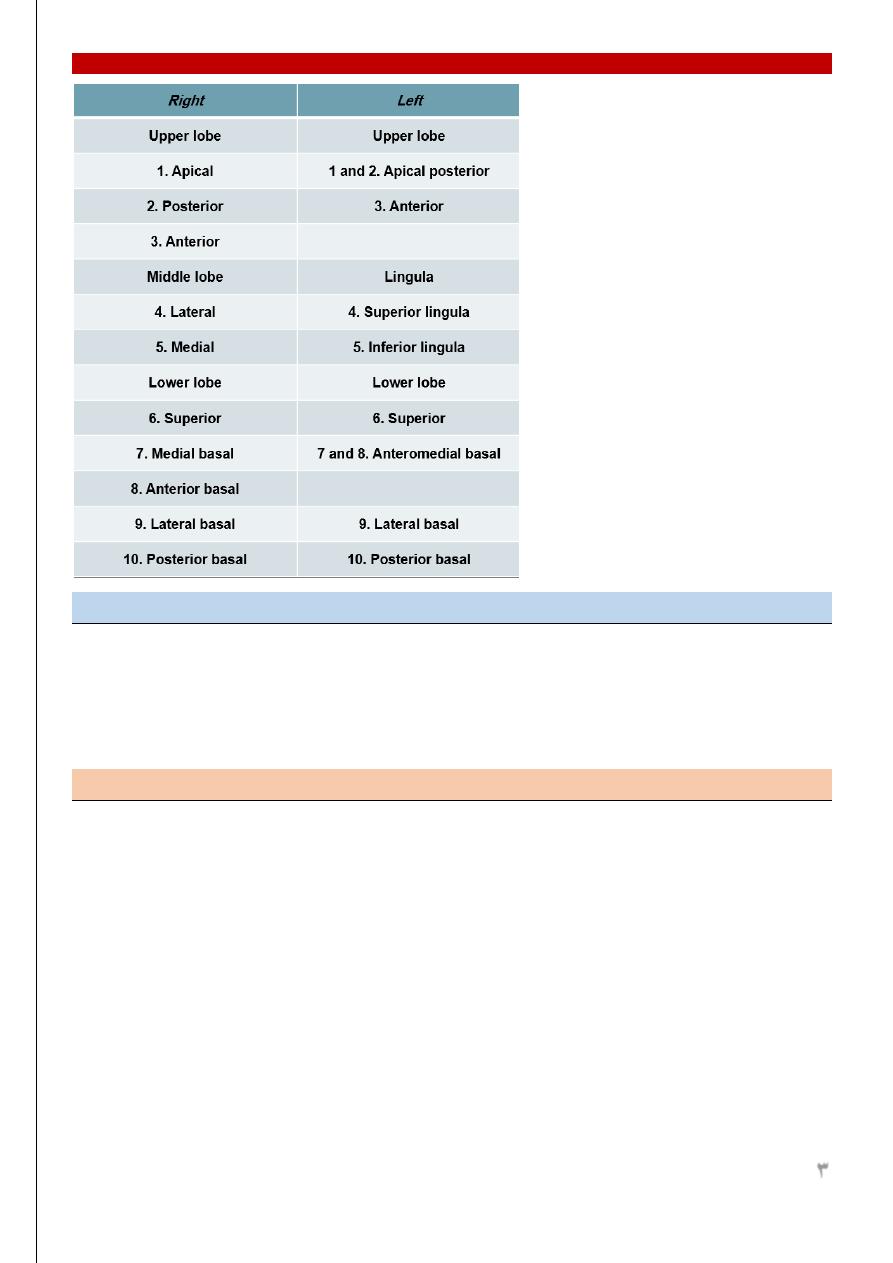
Lung Lobes, Fissures and Bronchopulmonary Segment Anatomy:
With the bronchus at the center, each bronchopulmonary segment functions as an individual unit
with its own pulmonary arterial and venous supply.
The larger right lung has three lobes—upper, middle, and lower—and is composed of 10
bronchopulmonary segments. The left lung has two lobes and 8 segments
D. Usama Surgery
Fifth Stage
3
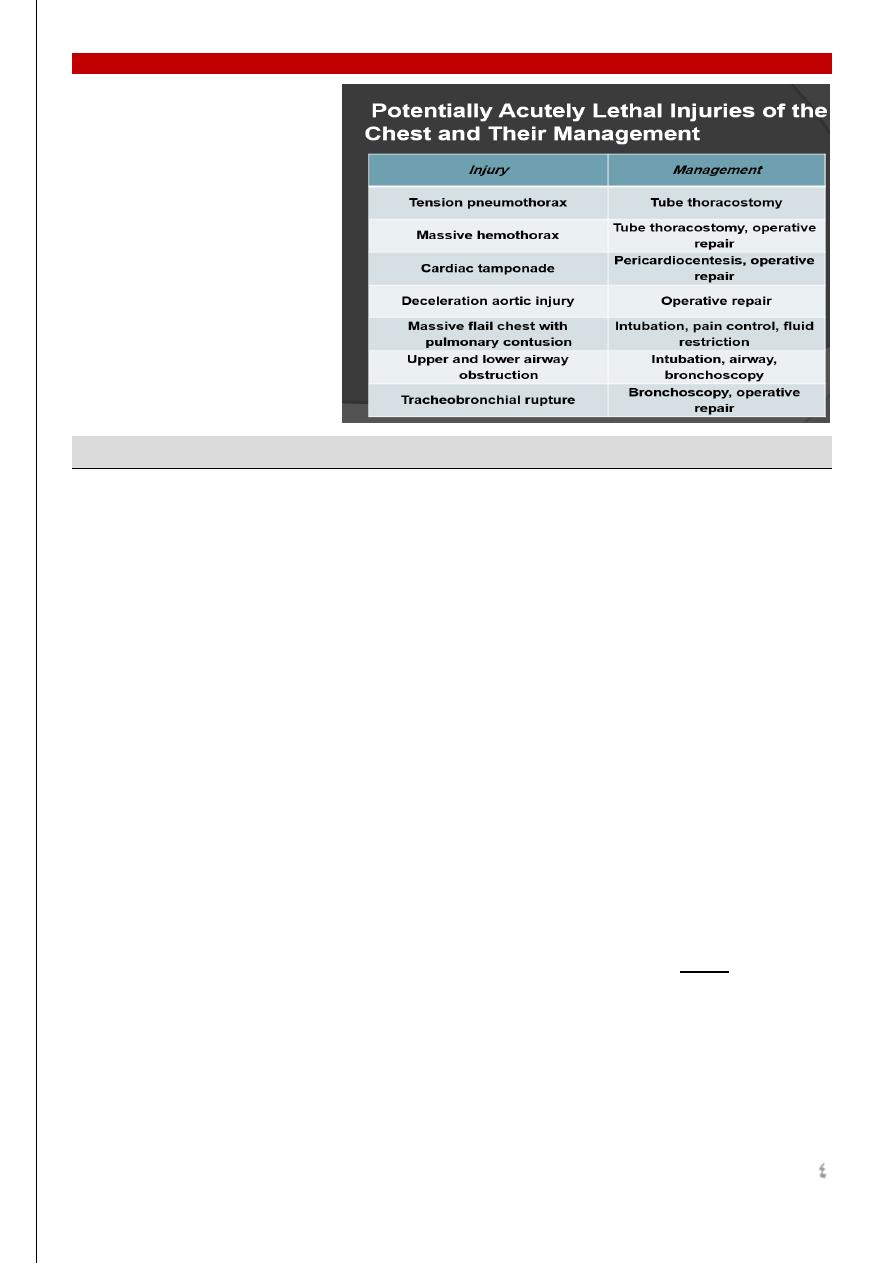
Chest Trauma
The chest contains the two most vital of the life sustaining organs; the heart and the lung.
Therefore any injury to the lung that seriously compromise the function of these organs is threat
to life. Many of these injuries are lethal (on spot) or within a short period of time, death often
occurs rapidly. Yet even in this critical situation the lives of over 80% of patients can be saved
with the prompt application of possible measures.
Types of trauma:
Non penetrating trauma
Blunt trauma
Crushing injury
Compression injuries: e.g.:
Crushing the chest wall between two blunt objects
The impaction of the driver against his steering wheel
Fall of a heavy object on the chest
Penetrating and perforating injuries
penetrating wound is a wound with site of entry and no site of exit
perforating wound is a wound with an entry and exit
A. War injuries: like pistol bullet, riffle bullet and fragments from bombs or shells
B. Civilian injuries: like knives and sharp instruments
D. Usama Surgery
Fifth Stage
4
Diagnostic tests:
This should be present in the ER of most hospitals
Chest Imaging:
CXR:
Fractures of the bony thorax,
Pneumothorax, hemothorax, or pulmonary contusion.
Mediastinum widening, pneumomediastinum, or shifting.
Subcutaneous air or foreign bodies.
width of the cardiac silhouette
tamponade.
CT scan:
Should not be performed in the severely hemodynamically unstable patient or in the
presence of life-threatening injuries. However,
It may reveal injuries not seen clearly on plain radiographs, such as aortic disruption,
pneumothorax, pneumomediastinum, and hemothorax.
It may be useful to screen all patients with blunt trauma and
Evaluate unusual or abnormal findings on initial chest X-ray (e.g., diaphragmatic injuries).
Echocardiography:
Focused Assessment for the Sonographic evaluation of the Trauma patient, or FAST examination
Angiography:
Angiography remains the gold standard in the diagnosis of aortic transection or injuries to the
great vessels
Indications for angiographic studies for potential thoracic injuries:
High-speed deceleration injuries
D. Usama Surgery
Fifth Stage
5
Chest X-ray findings :
Widened mediastinum
Loss of aortic knob shadow
Tracheal or esophageal deviation to the right
Downward displacement of left mainstem bronchus
Fractured first rib, sternum, or scapula Multiple rib fractures or flail chest
Massive hemothorax
Upper extremity hypertension
Unexplained hypotension
Pulse deficits
Systolic murmur
Conditions demanding early thoracotomy
Are less than 10%:
1. Continuing intrathoracic hemorrhage
2. Uncontrollable air leak
3. Wounds of the heart
4. Widening of the mediastinum
5. Large chest wall defects
6. Esophageal injuries
7. Massive hemoptysis
8. Cardiac tamponade
9. Ruptured diaphragm
10. Gross pleural contamination with foreign body
D. Usama Surgery
Fifth Stage
6
Chest wall injuries:
Open pneumothorax:
Causes: gun fire, blast, explosion
Manifestations: this will result in sucking wound of the chest wall and there may or may not be
associated injury to the intrathoracic structures. The defect in the chest wall allows air to enter the
pleural space during inspiration causing collapse of the lung and the process is reversed in
expiration.
Treatment: First aid station: the aim is to convert open Pneumothorax to a close one. This is done
by:
Covering the wound with gauze and elastic adhesives
Insertion of intercostals tube attached to underwater seal.
In hospital: after relieving respiratory distress and treating shock. The following lines of treatment
should be followed:
General anesthesia
• Limited thoracotomy
• Debridement
• Control bleeding
• Deal with other injuries
• Chest drain and closure.
Minimal Pneumothorax:
This requires no active treatment. The air will be absorbed and the lung re-expand fully in days –
weeks providing that contamination and lung injury are minimal.
Massive Pneumothorax:
This is treated by tube thoracostomy
Occasionally one find evidence of continuous leakage of large volume of air with failure of the
lung to remain expanded despite adequate pleural decompression by suction. In this situation one
should think of ruptured bronchus or injury to trachea. This can be confirmed by bronchoscopy
and immediate thoracotomy is essential
Tension Pneumothorax:
Massive pneumothorax may become tension pneumothorax, shock usually follows. The large
intrapleural pressure does not only collapse the ipsilateral lung and obstruct venous return to the
heart but also partially compress the contralateral lung.
Decompression of pleura for pneumothorax can be done by:
D. Usama Surgery
Fifth Stage
7
• insertion of a wide bore needle into the pleural space. (The practice of attaching intrapleural
wide bore needles to under water seal should not be done because the needle itself will
cause more damage when the lung expands.)
• Tube thoracostomy connected to underwater seal is the best effectively remove blood and
air.
If despite efficient large volume suction the lung fail to reexpand or the patient is losing more air
from his chest with every breath. A large air leak from ruptured bronchus should be suspected.
In spontaneously ventilating patients, the chest tube may be removed when:
• Lung fully expanded
• No air leak
Any sudden change in cardiovascular or respiratory status in a previously stable patient is in most
cases due to tension pneumothorax secondary to blocked tubes
Fracture of ribs:
Causes: usually blunt non penetrating injury.
Types:
Simple fracture: this is an isolated fracture usually occurring at the outer convexity. As the fracture
is not displaced, so there is no lung injury.
Multiple rib fractures: the ribs fracture at site of maximal curvature i.e., at the posterior and
anterior angles. Tear in the lung lead to hemo or pneumothorax.
Stove in chest: when multiple or single rib fracture produce a segment in the chest wall that is
permanently indented, i.e., portion of the thoracic cage is depressed.
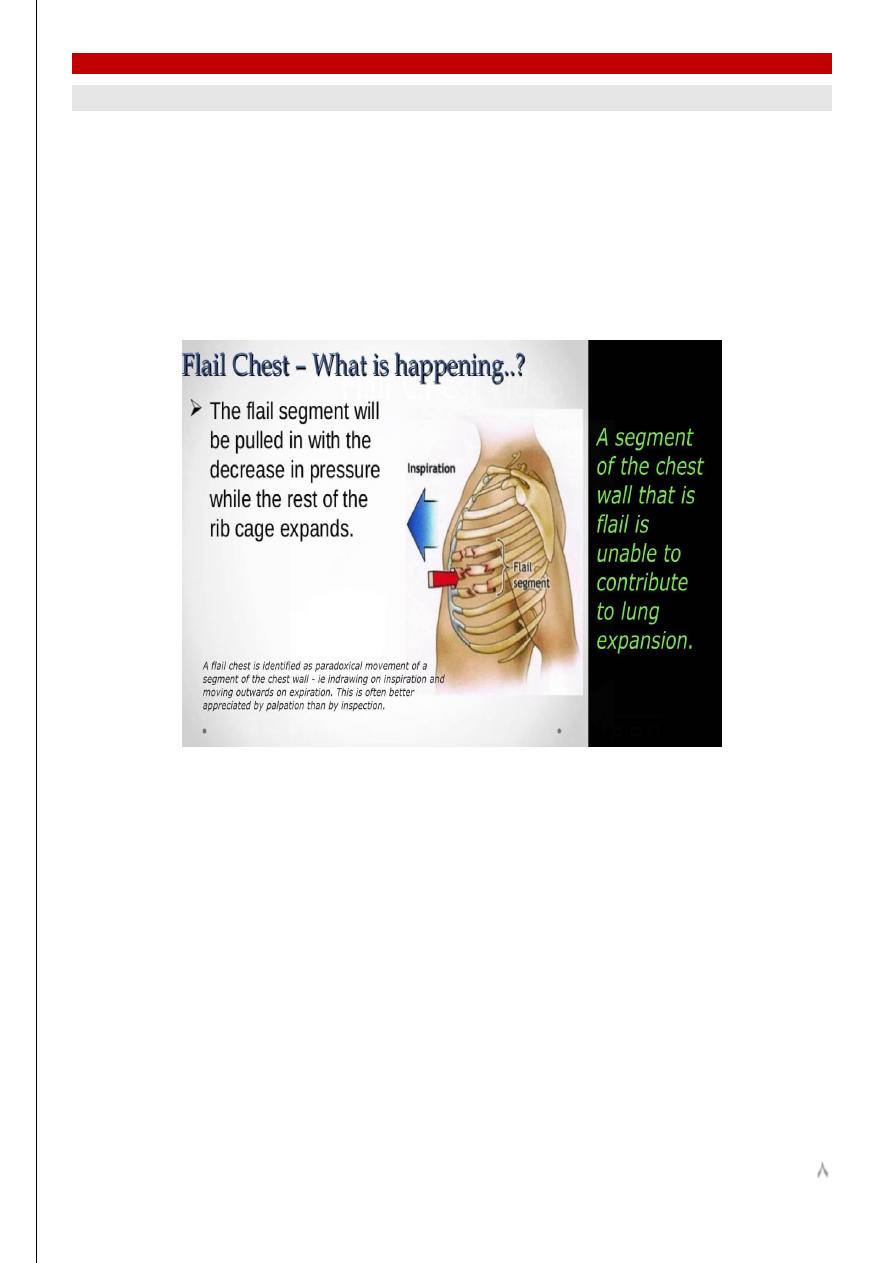
Flail chest: when the multiple ribs fractured produce a flaccid unstable segment exhibiting
paradoxical movement in which the flail area is sucked inwards during inspiration and pushed out
in expiration
Clinical manifestations:
pain, local tenderness, paradoxical movement, sputum reduction, and pneumothorax or
hemothorax or both.
Treatment:
Simple fracture: a. analgesia, b. intercostal nerve block, c. strapping, d. encourage
cough.
Multiple fractures: a. analgesia, b. O2, c. blood, d. tube thoracostomy, e. relieve
airway obstruction, f. stabilization of chest wall.
D. Usama Surgery
Fifth Stage
8
Treatment of flail chest:
Aim of treatment:
Establishing and maintaining a clear airway (endotracheal tube or tracheostomy).
Restoring and maintaining a stabilized chest wall by:
External immobilization
Traction
Internal fixation
IPPV
Drainage of pleural cavity and maintaining an expanded lung by tube thoracostomy.
Conservative treatment (External immobilization):
Pain relief, with close observation and hourly blood gas analysis.
Stabilization of the fractured segment by
Applying stabilizing pressure dressing over the involved segment of the chest wall as
adhesive tape strapping
Turning the patient on the injured side.
Placing a sand bag on the injured site.
Holding palm of hand on the injured site.
Advantages: Can be done at accident site and during hospitalization.
Disadvantages: impair ventilation and impair cough mechanism pneumonia due lower airway
obstruction and atelectasis.
Surgical treatment: fixation
Mechanical ventilator
D. Usama Surgery
Fifth Stage
9
Hemothorax:
Hemothorax and pneumo-hemothorax suggest far more serious situation than pneumothorax :
Causes: may be due to injury to the heart, great vessels, intercostal vessels and internal mammary
vessels.
Treatment:
Minimal hemothorax (blood in the pleural cavity is less than 300 cc) can be left without drainage
(observation only) and will be absorbed in about 10 days.
Moderate hemothorax can be treated by thoracocenthesis but if pneumothorax is also present tube
thoracostomy is needed.
Massive hemothorax treated by restoration of the circulation volume, tube thoracostomy, and then
thoracotomy
Tracheobronchial injuries:
Mainly due to penetrating injuries and rarely due to blunt ones.
It leads to:
Tracheal laceration.
Tracheal rupture.
Bronchial rupture.
Mechanism of blunt injury:
• Forceful antero-posterior compression of the thoracic cage (dashboard injury)
• A consequence of high airway pressures
• Rapid deceleration.
Manifestations:
Respiratory distress,
Dyspnea,
Hemoptysis
Air leak
pneumothorax, mediastinal emphysema... etc.
Hoarseness or dysphonia
Cardiac Tamponade: (a two edged sword)
The victim who lives long enough to reach the hospital is frequently alive because of cardiac
tamponade which prevent hemorrhage. Were if not for the pericardial sac, practically all wounds
of the heart would present a hopeless situation because of blood loss. Tamponade is therefore both
lethal and life saving up to a point. It contributes to the reduction of hemorrhage from the cardiac
wounds but beyond that point a continuation of its action produces profound shock which prove
fatal unless promptly relieved.
D. Usama Surgery
Fifth Stage
10
The two major immediate cause of death following knife or bullet wounds of the heart were either
bleeding or cardiac tamponade or combination of both.
Acute cardiac tamponade result in three physiological effects:
On the venous side:
The increased intrapericardial pressure restricts venous return to the heart resulting in an
elevated central venous pressure.
On the arterial side:
The resultant cardiac compression reduces cardiac output,
BP, and
coronary blood
flow
myocardial hypoxia and failure.
On the systemic side:
The reduced cardiac output initially leads to generalized vasoconstriction
peripheral
vascular resistance
maintenance of normal BP during the early stage of the tamponade
despite a progressively falling cardiac output and a progressively rising venous pressure
Presentation:
Shock
heart sounds
BP
Venous distention
CXR: wide mediastinum (large heart )
Treatment:
1. Airway management with endotracheal intubation,
2. Establishment of intravenous access capable of massive volume resuscitation,
3. Immediate thoracotomy through a left anterolateral approach using a fourth interspace
incision with extension across the sternum to the right side of the chest, if necessary. This
approach allows rapid exposure of the heart and the ability to relieve tamponade from
hemorrhage. In addition, it allows the surgeon the ability to perform open heart massage,
control cardiac injuries, cross-clamp the descending aorta to preferentially perfuse the
brain and coronary arteries, and allow volume resuscitation in the setting of shock.
Diaphragmatic injuries:
Causes: both penetrating and blunt trauma. The diaphragm may burst without any obvious
external wound like crushing between a wall and a car, compression of the abdomen, compression
of the lower costal cartilage…etc. mostly seen in the left diaphragm as the right is protected by
the liver.
Resulting in: diaphragmatic hernia
Manifestations:
D. Usama Surgery
Fifth Stage
11
Penetrating injuries: the injury to the abdomen or chest predominate and the diaphragm should
always be checked during laparotomy or thoracotomy.
Blunt trauma: diaphragmatic injury may be over looked especially when not associated with other
injuries and the patient may be presented late with diaphragmatic hernia.
Investigations:
• CXR _ chest CT
• Ba – swallow
Treatment:
• Thoracotomy
• Reduction of abdominal contents
• Closure of diaphragm
Mubark A. Wilkins
