Lecture-4 Management of Rheumatoid Arthritis
Possible Causes of Premature Death in RAChronic inflammation results in accelerated atherosclerosis leading to stroke& myocardial
infarction
Renal disease
Respiratory disease
Gastrointestinal disease
Infection
Objectives of RA Treatment
Relieve painDecrease joint inflammation
Prevent joint destruction
Restore function of disabled joints
Correct deformed joints
Maintain quality of life
Drugs for RA
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Disease-modifying anti-rheumatic drugs (DMARDs)
SyntheticBiologic
Glucocorticoids
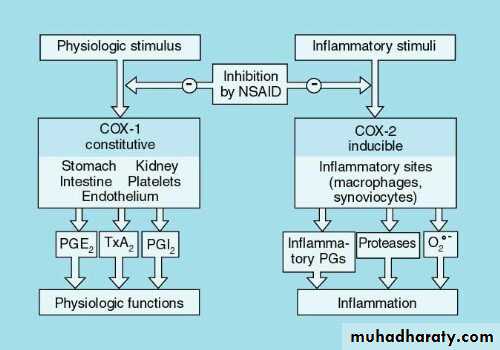
NSAIDsCyclo-oxygenase inhibitors
Do not slow the progression of the disease
Provide partial relief of pain and stiffnessNSAIDs
Non-selective COX inhibitorsIbuprofen
Diclofenac sodium
COX–2 inhibitors
celecoxib
COX-2 Inhibitors
COX-2 inhibitors appear to be as effective NSAIDsAssociated with less GI toxicity
However increased risk of CV eventsDMARDs
Disease Modifying Anti-Rheumatic DrugsReduce swelling & inflammation
Improve painImprove function
Have been shown to reduce radiographic progression (erosions)
90% of the joints involved in RA are affected within the first year
SO TREAT IT EARLYMANAGEMENT OF RHEUMATOID ARTHRITIS:Some Disease-modifying Anti-rheumatic Drugs (DMARDS)
• DMARD
• Methotrexate
• Hydroxychloroquine
• Sulfasalazine
• Leflunomide
• Azathioprine
• Cyclosporine
• Gold
MONITORING
Hematologic, lung, liver (avoid alcohol)
Ophthalmologic
Hematologic, GI
Hematologic, liver
Hematologic, liver
Renal, blood pressure
Hematologic, renal
Disease-modifying antirheumatic drugs DMARDs
DMARDs can substantially reduce the inflammation of RA, reduce or prevent joint damage, preserve joint structure and function, and enable a person to continue his or her daily activities. Although some DMARDs act slowly, they may allow to take a lower dose of glucocorticoids to control pain and inflammation.Drugs in this class include methotrexate, hydroxychloroquine, sulfasalazine, and leflunomide.
An improvement in symptoms may require four to six weeks of treatment with methotrexate, one to two months of treatment with sulfasalazine, and two to three months of treatment with hydroxychloroquine. Even longer durations of treatment may be needed to derive the full benefits of these drugs.
Combination therapy (using 2 to 3) DMARDs at a time works better than using a single DMARD
Synthetic DMARDs
MethotrexateSulphasalazine
Chloroquine
Hydroxychloroquine
Leflunomide
Methotrexate (MTX)
Dihydrofolate reductase inhibitor↓ thymidine & purine nucleotide synthesis
“Gold standard” for DMARD therapy7.5 – 30 mg weekly
Absorption variableElimination mainly renal
Biologics
Monoclonal Antibodies to TNF
Infliximab
Adalimumab
Soluble Receptor Decoy for TNF
Etanercept
Receptor Antagonist to IL-1
Anakinra
Monoclonal Antibody to CD-20
Rituximab
• Prompt introduction of DMARD therapy plays a central role.
• The patient should be advised that this will not improve symptoms immediately, but in the longer term there is a good chance that symptoms will come under control and joint damage will be prevented.• If the first-choice drug fails to control disease activity, other DMARDs can be added
If adverse effects occur, the patient should be switched to another DMARD.
If disease activity persists despite an adequate trial of two DMARDs including methotrexate, anti-TNF therapy should be considered.Most patients also require NSAID and other analgesics.
Because of the delayed onset of action, corticosteroids are often given when DMARDs are commenced to give symptomatic relief.
Tumor Necrosis Factor (TNF)
TNF is a potent inflammatory cytokineTNF is produced mainly by macrophages and monocytes
TNF is a major contributor to the inflammatory and destructive changes that occur in RA
Blockade of TNF results in a reduction in a number of other pro-inflammatory cytokines (IL-1, IL-6, & IL-8)Side Effects
InfectionCommon (Bacterial)
Opportunistic (Tb)
Demyelinating Disorders
Malignancy
Worsening CHF
Glucocorticoids
Potent anti-inflammatory drugsSerious adverse effects with long-term use
To control the disease
Indications
As a bridge to effective DMARD therapy
Systemic complications (e.g. vasculitis)
Surgery in RA
Synovectomy of the wrist or finger tendon sheaths of the hands may be required for pain relief or to prevent tendon rupture when medical interventions have failed.In later stages when joint damage has occurred, osteotomy, arthrodesis or arthroplasty may be required.
PROGNOSIS
average life span is reduced by 8-15 years & 5- years survival for patients with sever RA is only 50%.40% will be disabled within 4 years……..
Factors associated with poor prognosis:
1-systemic features(wt. loss, extra-articular manifestations)2-insidious onset
3- female gender
4-higher base line disability
5-rheumatoid nodules
6- involvement of MCP joints
7- positive rheumatoid factor
8- disease duration over 3 months
9- early bone erosions