
Lec. 2
Anaesthesia
Dr.Nazzal Jabr
2- Risk Assessment
There are three components that must be considered when evaluating perioperative risk:
1- The patient's medical condition preoperativel.
2- The extent of the surgical procedure.
3- The risk from the anaesthetic.
In general, the major contribution to increased risk is that of the patient's health prior to the procedure and
the magnitude of the surgery. However, patients presenting for surgery often have more fear about their
anaesthetic than the surgery itself.
Fortunately, anaesthesia-related morbidity and mortality is rare, but unfortunately, not absent. This does,
however, create its own problems. The combination of infrequent but serious events has led one author to
state that "Perhaps the most insidious hazard of anaesthesia is its relative safety.
Goals of Risk Assessment
Accurately assessing perioperative risk has two goals. The first is to assess the potential risk in performing
the desired procedure on a specific patient. The risk can be deferred, avoided altogether if it is severe, or
effectively reduced with intervention. Thus, accurate risk assessment is meaningful because it leads to a
decision to proceed, postpone, or cancel surgery. Emergent or lifesaving procedures must be performed,
regardless of the degree of perioperative risk, and some purely cosmetic surgeries may be postponed
indefinitely. But surgical procedures such as prostatectomy, cholecystectomy, and joint replacement lie in a
gray zone because postponement carries real long-term risk. Accurate preoperative assessment of
perioperative risk facilitates a decision about procedures in the gray zone.
The second goal is to identify modifiable risk factors. Although many factors that increase the risk of
surgery and anesthesia are static, the impact of others can be lessened, eliminated, or adjusted. Treatment of
ongoing pneumonia, coronary revascularization, and control of essential hypertension are examples of types
of modifiable risk. It is in this realm that the anesthesiologist may make the largest impact with accurate
preoperative risk assessment. By not only assessing risk but also identifying risk factors most amenable to
treatment and recommending appropriate modification of those risk factors, the balance of risk and reward
may be changed considerably.
Lec. 2
Anaesthesia
Dr.Nazzal Jabr
Anaesthetic Mortality
Several studies attempting to determine anaesthesia mortality and morbidity have been completed. It is
difficult to separate the contributions of anaesthesia and surgery to morbidity and mortality, as patients
rarely receive an anaesthetic without undergoing a surgical procedure.
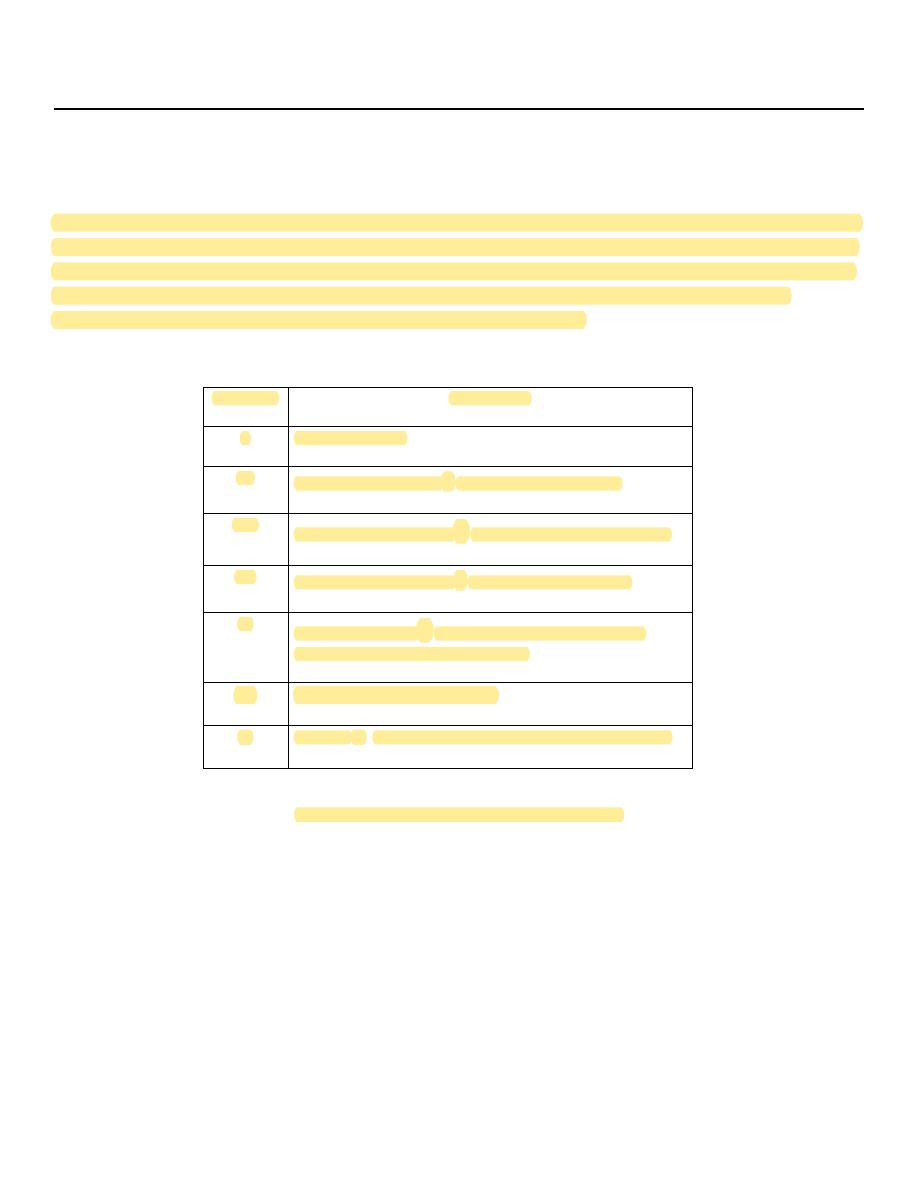
Table.1 summarizes several studies
which have attempted to determine the risk of mortality due solely to anaesthesia.
Table.1: Estlmates of Prlmary Anaesthetic
Mortality
Incidence of Primary
Anaesthetic Mortality
No. in
study
Year
Country
Author
1:5,138
195,232
1980
Canada
Turnbul
1:5,059
338,934
1980
Finland
Hovi-Vivander7
1:10,000
108,000
1982
United
Kingdom
Lunn & Mushin
1:10,000
163,240
1985
United States
Keenan & Boyen
1:13,207
198,103
1986
France
Tiret
1:26,000
550,000
1987
Australia
Holland1
1:185,000
500,000
1987
United
Kingdom
Buck1
Lec. 2
Anaesthesia
Dr.Nazzal Jabr
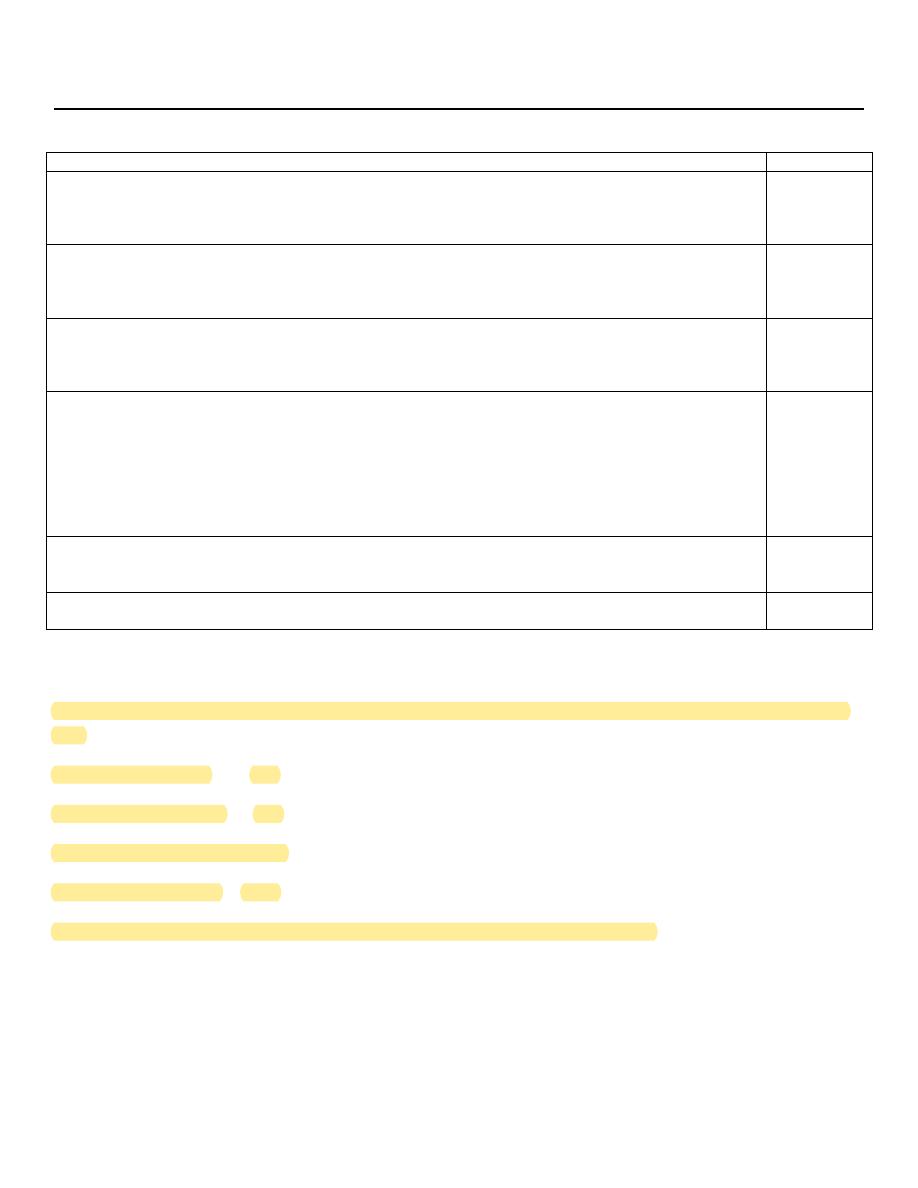
The ASA physical status
The ASA physical status classification system was originally proposed in 1941, and revised by Dripps in 1961
to provide a uniform assessment of a patient's preoperative physical condition. As this system is simple, easy
to use, and requires no laboratory investigations, it has now been widely accepted as the standard means of
preoperative patient classification. Although developed as a tool for classifying a patient's physical
condition, the ASA physical status has been used to stratify patient risk.
Category
Description
I
Healthy patient.
I1
Mild systemic disease
-
no functional limitation.
I11
Severe systemic disease
-
definite functional limitation.
IV
Severe systemic disease
-
a constant threat to life.
V
Moribund patient
-
not expected to survive with or
without an operation for 24 hours.
VI
Brain-dead organ donor
E
A suffix
E
is added to denote an emergency procedure.
Table 2: ASA Physical Status Classification
Cardiac Risk
Several perioperative risk studies have attempted to assess which perioperative cardiac risk factors are
important. Ischaemic heart disease has received the most attention because mortality from a perioperative
myocardial infarction approaches 50%. In 1977 Goldman published a multifactorial risk index for cardiac
patients undergoing non-cardiac procedures (table 3). A scoring system weighted these factors in their
ability to predict adverse cardiac outcome. From these data, Goldman suggested that patients with a score
greater than 25 be considered only for life-saving procedures. Patients scoring 13-25 were advised to have
preoperative medical consultations to lower their morbidity and mortality.
Lec. 2
Anaesthesia
Dr.Nazzal Jabr
Points
History
*
Age >70 years
*
Myocardial infarction within 6 months
*
5
10
Examination
*
Third heart sound (gallop rhythm), raised JVP
*
Significant aortic stenosis
11
3
ECG
*
Rhythm other than sinus, or presence of premature atrial complexes
*
>5 ventricular ectopics per minute
7
7
General condition
*
PaO2 <8kPa or PaCO2 >7.5 kPa on air
*
K+ <3.0 mmol/L;
*
HCO3- <20mmol/L
*
Urea >8.5 mmol/L; creatinine >200mmol/L
*
Chronic liver disease
*
Bedridden from non-cardiac cause
3
3
3
3
3
3
Operation
*
Intraperitoneal, intrathoracic, aortic
3
Emergency surgery
4
Table 3: Goldman's Cardiac Risk Index
The points total is used to assign the patient to one of four classes; the risks of perioperative cardiac events
are:
• Class I (0–5 points) 1%
• Class II (6–12 points) 5%
• Class III (13–25 points) 16%
• Class IV (=26 points) 56%
This has been shown to be a more accurate predictor than the ASA classification.
Lec. 2
Anaesthesia
Dr.Nazzal Jabr
3- Premedication
Premedication originally referred to drugs administered to facilitate the induction and maintenance of
anaesthesia. Nowadays, premedication refers to the administration of any drugs in the period before
induction of anaesthesia.
Indications of preoperative medication include:
I. Patient-related reasons:
1. Sedation
2. Amnesia
3. Analgesia
4. Antisialogogue effect (to dry oral secretions)
5. Medications to decrease gastric acidity and gastric volume.
6. To facilitate induction of anaesthesia.
II. Procedure-related reasons:
1. Antibiotic prophylaxis to prevent infective endocarditis in susceptible patients.
2. Gastric prophylaxis (to minimize the risk of gastric aspiration during anaesthesia).
3. Corticosteroid coverage in patients who are immunosuppressed.
4. To avoid undesired reflexes arising during a procedure (e.g., vagal reflex during eye surgery).
5. Anticholinergic agents to decrease oral secretions and facilitate a planned awake intubation with a
fiberoptic bronchoscope.
III. Coexisting Diseases:
1. To continue the patient's own medications for coexisting diseases. (e.g., beta blockers, antihypertensive
medications, nitrates, antiparkinsonian medications etc.)
2. To optimize the patients status prior to the procedure. (e.g., bronchodilators, nitroglycerine, beta blockers,
antibiotics etc.)
Patients with significant coexisting diseases should be given a reduced amount of preoperative sedative
medication. The obese patient does not necessarily require more preoperative medication. It is safer to
underestimate the required amount of preoperative medication.

Lec. 2
Anaesthesia
Dr.Nazzal Jabr
Additional medications can be given intravenously as needed when the patient arrives in the operating
room. Patients older than 65 years of age should have a reduced drug dosage.
Caution should be exercised in prescribing sedatives to patients 75 years of age or older, as they may
experience excessive depressant effects from these medications.
Contraindications to the premedication
1. Allergy or hypersensitivity to the drug.
2. Upper airway compromise, or respiratory failure.
3. Hemodynamic instability or shock.
4. Decreased level of consciousness or increased intracranial pressure.
5. Severe liver, renal, or thyroid disease.
6. Obstetrical patients.
7. Elderly or debilitated patients.
Preoperative starvation
Traditionally, patients were starved of both food and fluids for prolonged periods preoperatively, but it is
now increasingly recognized that, apart from certain groups with an increased risk of aspiration, this is not
necessary.
Guidelines for preoperative Fasting policy :
1. No solid food for 6 h preoperatively.
2. No formula milk and non clear fluid for 4 h preoperatively.
3. No clear fluids and breast milk for 2h preoperatively.
N.B.
Chewing gum does not increase gastric volume and is best treated as for clear fluids.
Normal medications can be taken with a sips of water.
There is some factors that delayed gastric emptying.
