1
L2
Viral Infection
D. Hazim
Viral meningitis
Viral infection is the most common cause of meningitis, and usually results in a benign and self-limiting illness
requiring no specific therapy. It is a much less serious illness than bacterial meningitis unless there is associated
encephalitis.
Clinical features
The condition occurs mainly in children or young adults, with acute onset of headache and irritability
and the rapid development of meningism.
In viral meningitis, the headache is usually the more severe feature.
There may be a high pyrexia, but focal neurological signs rarely occur.
Viruses
Enteroviruses (echo, Coxsackie, polio)
Mumps
Influenza
Herpes simplex
Varicella zoster
Epstein-Barr
HIV
Investigations
The CSF usually contains an excess of lymphocytes, but glucose and protein levels are commonly normal or the
protein level may be raised.
Management
There is no specific treatment and the condition is usually benign and self-limiting. The patient should be treated
symptomatically in a quiet environment. Recovery usually occurs within days, although a lymphocytic
pleocytosis may persist in the CSF.
VIRAL ENCEPHALITIS
Common viruses causing viral encephalitis
Arboviruses
Enteroviruses
HSV
Pathology
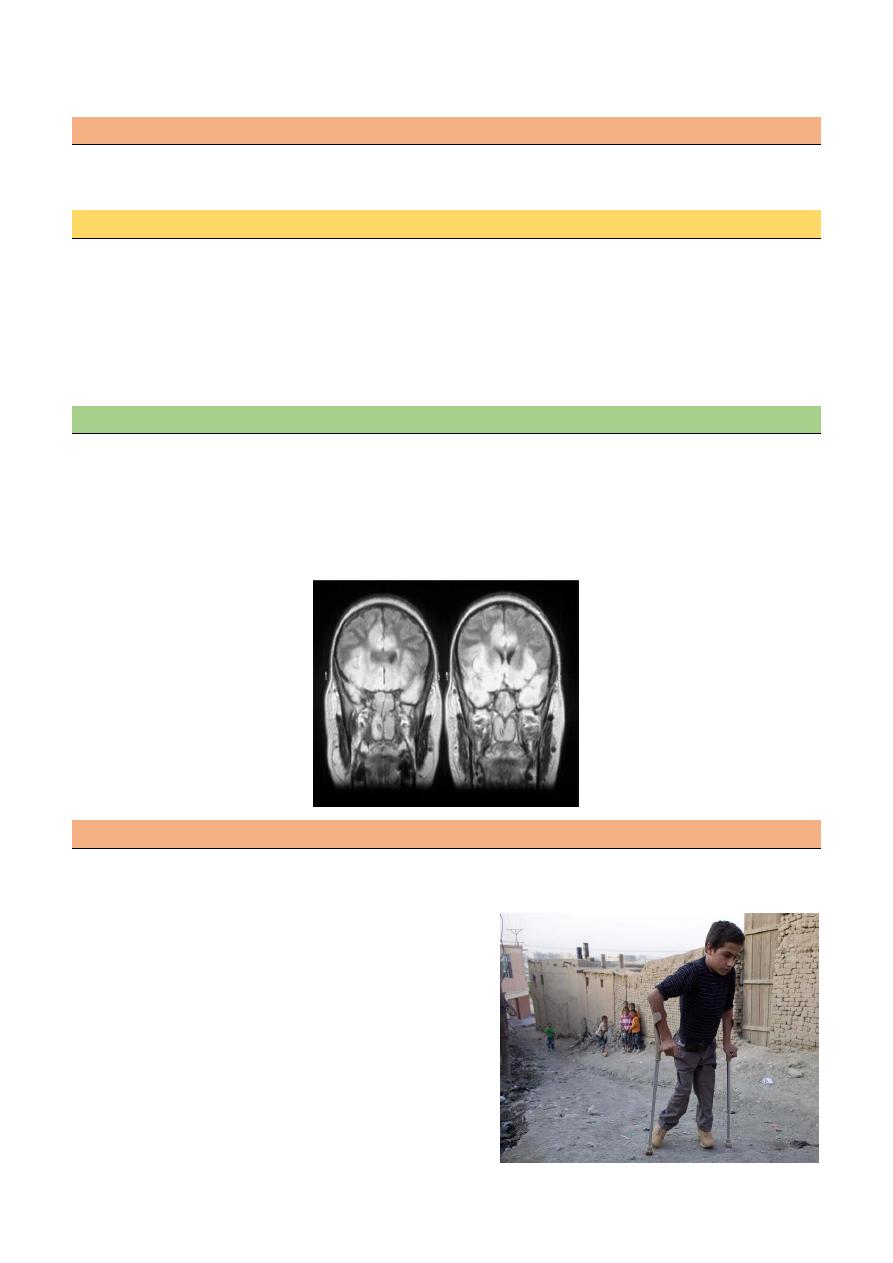
Inflammation can occur in the cortex, white matter, basal ganglia and brain stem, and the distribution of
lesions varies with the type of virus.
In herpes simplex encephalitis, the temporal lobes are usually primarily affected.
Clinical features
Viral encephalitis presents with acute onset of headache, fever, focal neurological signs (aphasia and/or
hemiplegia) and seizures.
Disturbance of consciousness ranging from drowsiness to deep coma.
Meningism occurs in many patients.
Herpes simplex encephalitis
The majority of cases of herpes simplex encephalitis (HSE) in adults are caused by HSV-1.
10% are caused by HSV-2, usually associated with immuno-compromise or occurring in the neonate.
2
The herpes virus leads to inflammation, infection and necrotizing lesions particularly in the inferior and
mesial temporal lobes, which may also involve the orbital frontal cortex and limbic structures.
Route of infection
Primary infection usually develops in the oropharyngeal mucosa before the virus is transported by retrograde
transneuronal spread via the trigeminal nerve to establish latency in the olfactory bulb or trigeminal ganglion.
Clinical feature
The onset of HSE is with fever, headache and alteration of consciousness which may develop gradually
or rapidly over amatter of hours.
The most common manifestations are personality change, dysphasia with progressive behavioral
disturbance and occasional psychotic features.
Less typical features include the development of hemiparesis or a visual field defect (particularly
superior quadrantic).
Focal or generalized seizures are often associated with olfactory or gustatory hallucinations
Diagnosis
The EEG show periodic sharp-wave complexes from temporal lobe on low amplitude background
CT-scan low density lesion within the temporal lobe with mass effect .
MRI-high signal intensity on T2
CSF-Lymphocytic pleocytosis, elevated protein, normal or glucose
PCR to detect HSV DNA in CSF
CSF may contain RBCs (due to necrosis in the brain tissue)
Treatment:
Acyclovir (10mg/Kg every 8 hour IV for more than 1 hr for 3 weeks) +good hydration
Anticonvulsant therapy (seizure occur in 30%), so Clonazepam, or phenytoin are recommended
3
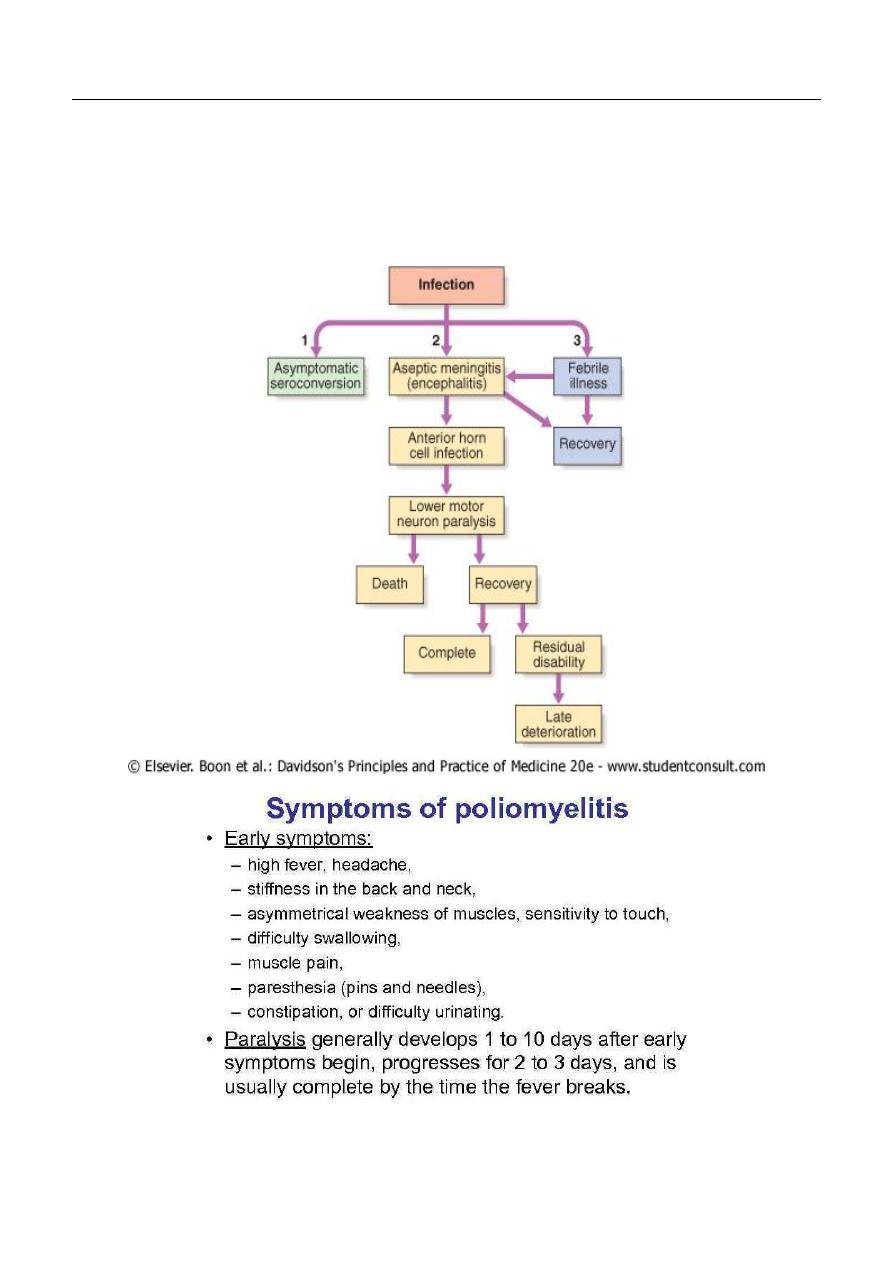
POLIOMYELITIS
The disease is caused by one of three polioviruses, which are a subgroup of the enteroviruses.
It is much less common in developed countries following the widespread use of oral vaccines but is
still a problem in the developing world.
Infection usually occurs through the nasopharynx.
The virus causes a lymphocytic meningitis and infects the grey matter of the spinal cord, brain stem
and cortex.
There is a particular propensity to damage anterior horn cells, especially in the lumbar segments.
Mubark A. Wilkins

4



