Fifth Stage
Internal Medicine
Dr. Abbas / Lec . 9
1
HEMORRHAGIC CEREBROVASCULAR DISEASE
15% of stroke
10% intra-cerebral hemorrhage
5% subarachnoid hemorrhage
Intracerebral hemorrhage
Causes
1-Hypertension
2-Amyloid (congophilic) angiopathy
3-Arteriovenous malformation
4-Bleeding diathesis
5-Drugs (amphetamines, cocaine, anticoagulants, thrombolytics)
6-head injury
7-tumour
In hypertensive ICH :
Rupture of microaneurysms (Charcot-Bouchard aneurysms, 0.8-1.0 mm
diameter) and degeneration of small deep penetrating arteries are the principal
pathology. Such hemorrhage is usually massive, often fatal and occurs in
chronic hypertension and at well-defined sites - basal ganglia, pons, cerebellum
and subcortical white matter .
In normotensive patients,
particularly over 60 years, lobar intracerebral hemorrhage occurs - in the
frontal, temporal, parietal or occipital cortex. Cerebral amyloid angiopathy
(rare) is the cause in some of these hemorrhages, and the tendency to re-bleed
is associated with particular apolipoprotein E genotypes
Clinical Manifestations
Although not particularly associated with exertion, intracerebral hemorrhages
almost always occur while the patient is awake and sometimes when stressed.
The hemorrhage generally presents as the abrupt onset of focal neurologic
deficit. Seizures are uncommon. The focal deficit typically worsens steadily
over 30–90 min and is associated with a diminishing level of consciousness and
signs of increased ICP, such as headache and vomiting
The putamen is the most common site for hypertensive hemorrhage, and the
adjacent internal capsule is usually damaged
Contralateral hemiparesis is therefore the sentinel sign.. When hemorrhages
are large, drowsiness gives way to stupor as signs of upper brainstem
compression appear. Coma ensues, accompanied by deep, irregular, or
2
intermittent respiration, a dilated and fixed -pupil, and decerebrate rigidity. In
milder cases, edema in adjacent brain tissue may cause progressive
deterioration over 12–72 h.
In pontine hemorrhages, deep coma with quadriplegia usually occurs over a
few minutes. There is often prominent decerebrate rigidity and "pin-point" (1
mm) pupils that react to light., severe hypertension, and hyperhidrosis are
common. Death often occurs within a few hours, but small hemorrhages are
compatible with survival
Cerebellar haemorrhage There is headache and rapid reduction of
consciousness with signs of brainstem origin (e.g. nystagmus, ocular palsies).
Gaze deviates towards the haemorrhage. Skew deviation may develop.
There are unilateral or bilateral cerebellar signs, if the patient is awake.
Cerebellar haemorrhage sometimes causes acute hydrocephalus. Emergency
surgical clot evacuation is often necessary after imaging
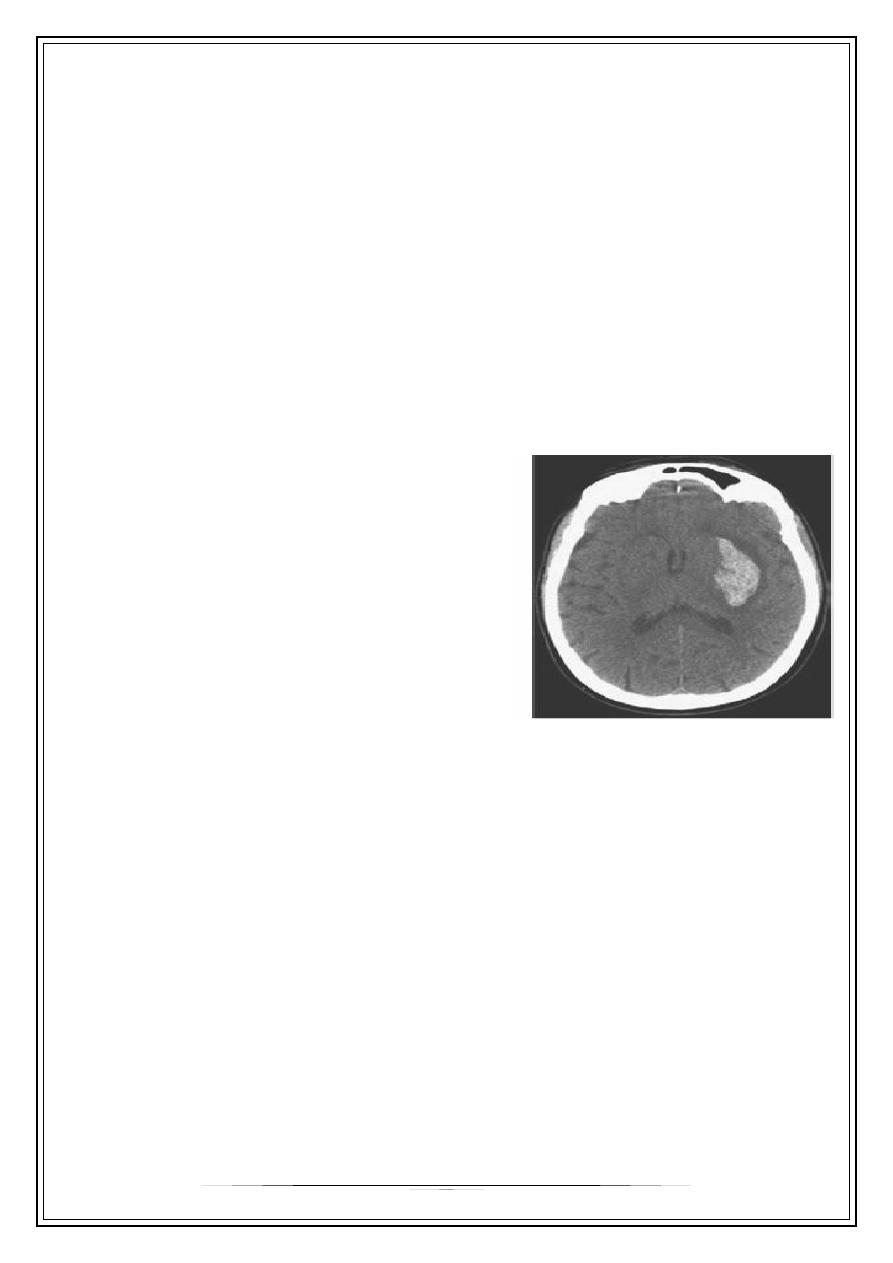
Diagnosis
Intracerebral hemorrhage often cannot be
distinguished from other types of strokes
based on clinical findings alone. The test of
choice for making the diagnosis is a non–
contrast-enhanced CT scan that shows
areas of hemorrhage as zones of increased
density, which may or may not have
associated regions of decreased density
indicating infarction.
Treatment
General Measures
With initial care directed at maintenance of the airway, oxygenation, nutrition,
and prevention and treatment of secondary complications.
Optimal blood pressure treatment is uncertain, although the general guidelines
for excessive hypertension and reduction of cerebral perfusion apply as for
ischemic strokes.
There is no accepted protocol for the management of increased intracranial
pressure; osmotherapy, hyperventilation, and neuromuscular paralysis rarely
are beneficial.
Fluid management should maintain euvolemia; fluid restriction or volume
expansion is not of proven value.
Seizures are particularly harmful in critically ill patients and are treated despite
lack of data from randomized trials.
Maintenance of normal body temperature is theoretically desirable because
fever may accelerate tissue destruction
3
Medical Therapy
Intravenous administration of recombinant factor VIIa within 4 hours after
onset reduces the volume of hemorrhage and surrounding cerebral edema, as
measured by CT, and improves neurologic outcomes at 90 days despite an
increase in ischemic stroke and myocardial infarction [.
2
]
Corticosteroids may increase the risk for infectious complication
Surgical Therapy
The goal of surgical treatment of intracerebral hemorrhage is to remove as
much blood clot as possible as quickly as possible. Ideally, surgery should
remove the underlying cause, such as an AVM, and prevent hydrocephalus.
Early surgical intervention to evacuate intracerebral hematomas within 24
hours is no better than medical therapy .However, patients who have
cerebellar hemorrhages and are deteriorating because of brain stem
compression and hydrocephalus caused by ventricular obstruction are still
recommended by some for removal of the clot or amputation of part of the
cerebellum, although no proof exists to support this approach
Subarachnoid haemorrhage
Subarachnoid haemorrhage (SAH) means spontaneous arterial bleeding into
the subarachnoid space, and is usually clearly recognizable clinically by its
dramatic onset. SAH accounts for some 5% of strokes and has an annual
incidence of 6 per 100 000 .
Causes
1-saccular or berry aneurysm 85%
2-non-aneurysmal hemorrhage [10%]
3-AV malformation [5%]
Saccular aneurysms develop on the circle of Willis and adjacent arteries.
Common sites are at the following arterial junctions:
*Between posterior communicating and internal carotid artery - posterior
communicating artery aneurysm
*Between anterior communicating and anterior cerebral artery - anterior
communicating artery aneurysm
*At a bifurcation or at the trifurcation of the middle cerebral artery - middle
cerebral artery aneurysm .
Aneurysms cause symptoms either by spontaneous rupture, when there is
usually no preceding history, or by direct pressure on surrounding structures;
for example, an enlarging unruptured posterior communicating artery
aneurysm is the commonest cause of a painful third nerve palsy
Arteriovenous malformation (AVM) This is a collection of arteries and veins of
developmental origin, usually within the hemisphere. An AVM may also cause
4
epilepsy, often focal. Once an AVM has ruptured the tendency is to rebleed -
10% will then do so annually
Clinical features of SAH
There is a sudden devastating headache, often occipital. This is usually
followed by vomiting and often by coma. The patient remains comatose or
drowsy for several hours to several days, or longer. Less severe headaches
cause difficulty but SAH is a
possible
diagnosis in any sudden headache.
After major SAH there is neck stiffness and a positive Kernig's sign.
Papilloedema is sometimes present and accompanied by retinal and subhyaloid
haemorrhage (tracking beneath the retinal hyaloid membrane). Minor bleeds
cause few signs, but almost invariably headache
Investigations
CT imaging is the initial investigation of choice
Subarachnoid or intraventricular blood is usually seen.
Lumbar puncture is not necessary if SAH is confirmed by CT, but should be
performed if doubt remains. The CSF becomes yellow (xanthochromic) several
hours after SAH. Visual inspection of the supernatant CSF is usually sufficiently
reliable for diagnosis, but there is a move to use spectrophotometry to
estimate bilirubin released from lysed cells to define with certainty SAH in
doubtful cases.
MR angiography is usually performed in all potentially fit for surgery, i.e.
generally below 65 years and not in coma. In some cases, no aneurysm is
found despite a definite SAH .
Complications
1-hydrocephalus
Blood In the subarachnoid space can lead to obstruction of CSF flow and
hydrocephalus. This can be asymptomatic but may cause deteriorating
consciousness after SAH. Diagnosis is by CT. Shunting may be required .
2-Severe arterial spasm (visible on cerebral angiography and a cause of
coma or stroke) sometimes complicates SAH. It is a poor prognostic sign .
3-Rebleeding
Approximately 30% of patients with aneurysmal subarachnoid hemorrhage
rebleed during the first month, and the incidence is highest during the first 2
weeks after the initial episode. Patients with unrepaired aneurysms who
survive their initial bleeding for more than 1 month have a 2 to 3% annual risk
of rebleeding
4-Seizures
Seizures may occur shortly after subarachnoid hemorrhage in 15 to 90% of
patients. Seizures are thought to be caused by cortical damage from bleeding
into the neocortex or from ischemic necrosis related to vasospasm. The
5
development of persistent epilepsy is unusual. Prophylactic anticonvulsant
therapy has not been useful
Non-neurologic Complications
1-Cardiac complications occur as a consequence of subarachnoid hemorrhage.
In the acute phases of subarachnoid hemorrhage, electrocardiographic
patterns can mimic acute myocardial infarction, a pattern of deep inverted T
waves across the pericardium is classic. Appropriate biomarker assays and
repeat electrocardiograms are needed to document true myocardial damage.
2-hyponatremia
is the most common electrolyte abnormality after subarachnoid hemorrhage.
Sodium loss, which is typically mild, may occur in up to 25% of patients. The
natriuresis has been attributed to inappropriate levels of antidiuretic hormone,
but this hypothesis has not been proved. Hyponatremia can itself result in a
decreased level of consciousness and seizures, but it is often impossible to
distinguish the effects of hyponatremia from the other possible causes of these
neurologic abnormalities
Management
Immediate treatment of SAH is bed rest and supportive measures.
Hypertension should be controlled. Dexamethasone is often prescribed, to
reduce cerebral oedema; it also is believed to stabilize the blood-brain barrier.
Nimodipine, a calcium-channel blocking agent, reduces mortality.
All surviving SAH cases should be discussed urgently with a specialist
neurosurgical centre. Nearly half SAH cases are either dead or moribund before
they reach hospital. Of the remainder, a further 10-20% rebleed and die in the
next several weeks. Delay or failure to diagnose SAH without coma (e.g.
mistaking it for migraine) contributes to this mortality .
Patients who remain comatose or with persistent severe deficits have a poor
prognosis. In others, where angiography demonstrates aneurysm, a direct
neurosurgical approach to clip the neck of the aneurysm is carried out. In
selected cases the results of surgery are excellent. Invasive radiological
techniques, such as inserting a fine wire coil into an aneurysm are also used.
Direct surgery, microembolism and focal radiotherapy ('gamma knife') are used
in AVM .
Thank you,,,
