اﻟﺮﺣﻤﻦ اﻟﻠﮫ ﺑﺴﻢ
اﻟﺮﺣﯿﻢ
اﻟﻐﺎﻧﻣﻲ ﺷﻛر ﺧﺿﯾر ﻣﮭﻧد.د
اﻟو اﻟﻘﻠب وﺗﺷوھﺎت ﺑﺄﻣراض دﻗﯾق أﺧﺗﺻﺎص
وا واﻟﻛﺑﺎر ﻟﻸطﻔﺎل اﻟﻘﺳطﺎري واﻟﺗداﺧل ﻻدﯾﮫ
اﻟﻘﻠﺑﯾﮫ ﻷﻣراض
اﻟﻣﻛﺗﺳﺑﮫ
ﻟﻸطﻔﺎل

Rheumatic fever and
Rheumatic heart disease

Acute rheumatic fever is a non-suppurative complication of group A beta
hemolytic streptococcal (GABHS) sore throat.
It affects joints, skin, subcutaneous tissue, brain and heart. Except heart, all
other effects are reversible
Cardiac complications are significant in absence of secondary prophylaxis and
culminate into chronic and life threatening valvular heart disease
Acute rheumatic fever (RF) occurs as a result of a complex interaction between
group A streptococcus (GAS), a susceptible host, and the environment
RF is the most common cause of acquired cardiac disease in children and young
adults 80% of children younger than 15 years of age

The degree of cardiac involvement is quite variable, ranging from very
mild, subclinical
valvulitis to severe carditis with significant acute mitral and/or aortic
regurgitation
resulting in heart failure. The acute rheumatic cardiac involvement may
resolve or
Persist and evolve as chronic rheumatic valvular disease, with cardiac
symptoms
developing years after the initial episode

Host:
Children between the ages of 5 and 15 years are most commonly affected. RF is
uncommon before age 5 years, almost never occurs before 2 years of age, and is
uncommon beyond the age of 35 years.
Children with RF before age 5 years commonly present with arthritis and rarely present
with chorea; when present, cardiac involvement is more severe than in older children
and persistent RHD is common
Adults with a primary episode of RF are much more likely to have joint manifestations
than cardiac involvement . Recurrences are most frequent during adolescence and
early adulthood.
With the exception that chorea is more common in girls, there is no definite
gender predisposition
Most of the clinical manifestations of RF occur approximately 10 days to 5 weeks
(average 18 days) following GAS pharyngitis in a susceptible host
Streptococcal Infection:
Most children have at least one episode of pharyngitis per year,
approximately
10% to 30% of which are due to GAS, the most common
bacterial cause of
pharyngitis certain GAS strains have been associated with RF,
while others have
been associated with poststreptococcal glomerulonephritis
M types 1, 3, 5, 6, 14, 18, 19, 24, 27, and 29 have been
associated with
outbreaks of RF

Natural History
The prognosis and natural history of rheumatic carditis and RHD are strongly influenced
by both the severity of the initial carditis and RF recurrences Mild carditis without
recurrences is much more likely to show resolution than severe initial carditis and/or
cases with recurrent episodes of RF.
Only 30% to 40% of patients with acute mitral regurgitation have a persistent murmur at
follow-up, with most of the clinical improvement occurring in the first 6 months after
the acute illness.
Patients with more severe carditis (heart failure and/or cardiomegaly) are more likely to
have persistent RHD and aortic regurgitation is less likely to decrease in severity or
disappear than mitral regurgitation .
Age and gender also influence prognosis, as acute rheumatic cardiac involvement
resolves more frequently in boys , and children presenting with RF before age 5 years
have more severe cardiac involvement and more commonly have persistent chronic
RHD
The diagnosis of RF requires :
two major, or one major and two minor Jones criteria along with
evidence of a preceding streptococcal infection.
The major criteria are polyarthritis, carditis, chorea, a characteristic rash
called erythema marginatum, and subcutaneous nodules.
The minor criteria are fever, arthralgia, elevated acute phase reactants,
and
prolonged PR interval on the ECG and evidence of a preceding GAS
infection
The latest Update allows the diagnosis of RF to be made without
fulfilling the above criteria in three circumstances:
1-patients who present with isolated chorea
(2) patients who present with indolent or insidious onset carditis
(detected months to years after the acute illness),
(3) patients with a prior history of RF/RHD
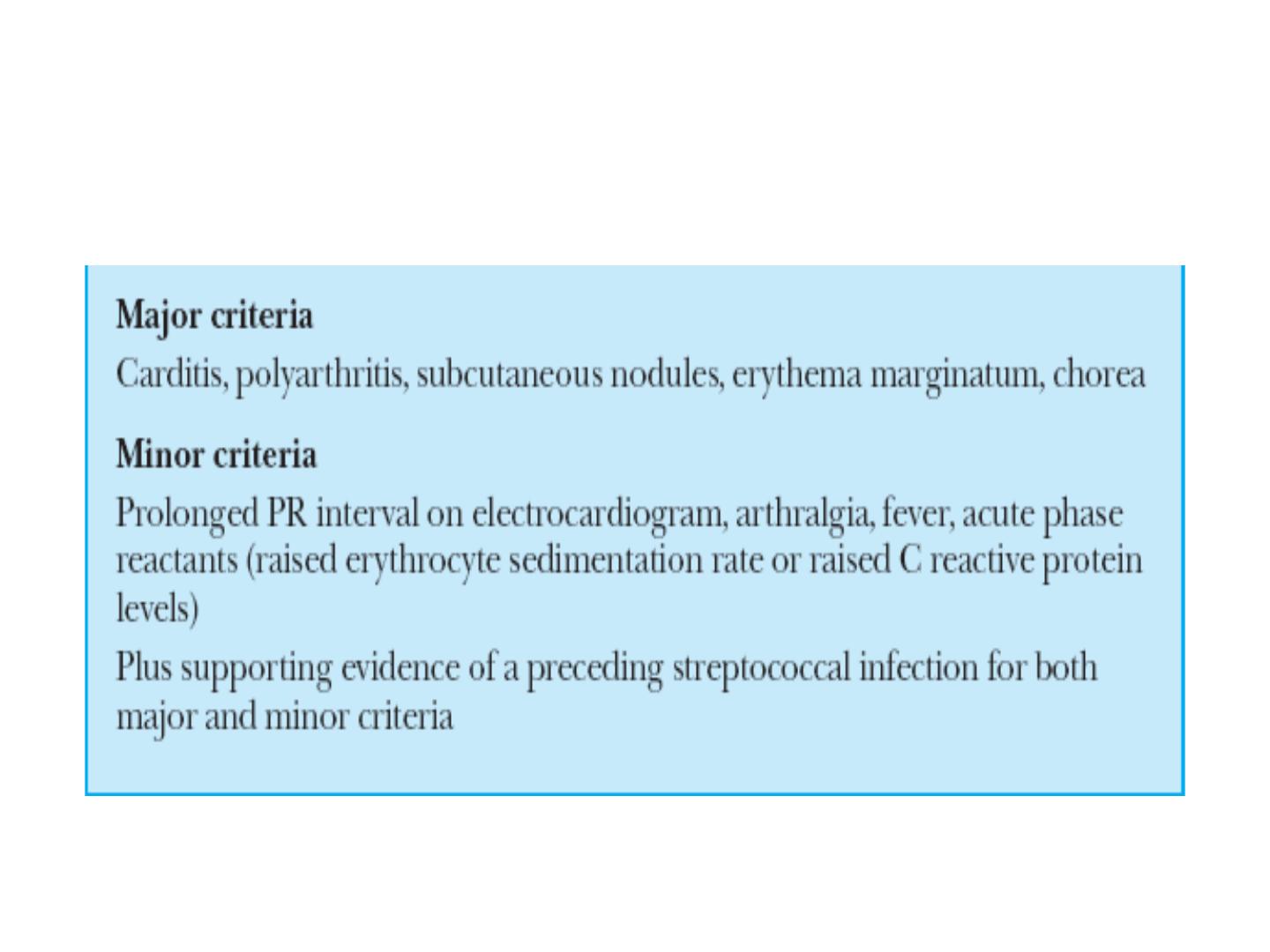
Modified Jones Criteria for diagnosis of
acute Rheumatic fever

Arthritis
The latency period between GAS infection and most manifestations of RF ranges from 10 days to 5
weeks (latency between GAS infection and chorea is 1 to 6 months).
Of the major Jones criteria, migratory polyarthritis is most common, affecting 40% to 70% of cases .
The arthritis of RF classically migrates from large joint to large joint, and most commonly affects
the knees, ankles, elbows, and wrists.
Importantly, the presentation and evolution of the joint manifestations may be affected by
administration of anti-inflammatory medications (aspirin or other nonsteroidal anti-
inflammatory agents), monoarticular arthritis is a common mode of presentation .
The joints affected with RF are red, swollen, and extremely tender.In some cases, the joints may be
involved sequentially and simultaneously rather than in a migratory pattern, with a new joint
becoming involved while a different joint is at a different phase of inflammation and resolution.
Even untreated, the arthritis of RF usually resolves within 3 to 4 weeks and is not associated with
residual abnormalities.
Although carditis and arthritis commonly occur together, the severity of the joint and heart involvement
tend to be inversely related . The reasons for this inverse relationship are unclear; some have
speculated that joint involvement leads to earlier medical attention and initiation of
antiinflammatory treatment, thus preventing more severe cardiac involvement

The arthritis of RF typically responds to aspirin within 48 to 72 hours. In fact, lack of
clinical response and improvement within 2 to 3 days should prompt consideration
of alternative diagnoses
Unfortunately, although arthritis is the most common major manifestation of RF, it is
also the least specific
Some patients develop arthritis after a streptococcal pharyngitis that differs from that
typically associated with acute RF. This entity, termed poststreptococcal reactive
arthritis, typically occurs after a shorter latent period (7 to 10 days) and tends to be
nonmigratory and more persistent, in some cases involves small joints or the axial
skeleton, and does not respond as dramatically to anti-inflammatory medications as
does the typical arthritis of RF

Sydenham chore
It is now known that the clinical manifestations of Sydenham chorea occur due to
neuropathologic changes and inflammation in the basal ganglia, cerebral cortex and
the cerebellum
Sydenham chorea occurs in approximately 10% to 30% of cases of RF . The gender
distribution is equal in younger children, but after the age of 10 years, females are
more often affected, and chorea is uncommon in postpubertal males . Involuntary,
purposeless movements, muscular incoordination and/or weakness, and emotional
lability
Movements are abrupt and erratic, commonly affecting muscles of the face and
extremities. Findings may include “fidgetiness,” facial grimaces, tongue movements
described as resembling a “bag of worms,” halting and explosive speech, pronation
of the hands

Irregular contractions of the hands when asked to squeeze an object
(“milkmaid's grip”), hyperextension of the fingers when hands are extended
forward with eyes closed (“spooning”), and clumsiness. Patients often come
to attention based on deterioration in school performance, and
neurobehavioral symptoms seen along with the chorea include irritability,
poor attention span, lack of cooperation, and obsessive-compulsive
symptoms are not uncommon. Sensory deficits do not occur. The neurologic
manifestations are usually bilateral, but may be unilateral (hemichorea). The
neurologic symptoms tend to decrease with rest
and sedation and increase with effort or excitement. The duration of chorea is
variable, ranging from 1–2 weeks to 2–3 years.
Carditis
The manifestation of RF associated with long-term morbidity and mortality is carditis,
which occurs in 30% to 70% of cases
Despite traditionally being described as a pancarditis, the dominant and most important
abnormality with acute rheumatic cardiac involvement is the valvulitis, specifically
mitral and/or aortic regurgitation. The clinical presentation may be quite variable,
ranging from the asymptomatic patient with a characteristic heart murmur to the
critically ill patient presenting in heart failure.
Approximately 80% of patients who develop carditis do so within the first 2 weeks of
the RF illness; if no cardiac involvement is detected in the first 2 weeks, the
likelihood of subsequent cardiac involvement during the acute phase is low
tachycardia is often one of the earliest signs of carditis.
A high-pitched, regurgitant, holosystolic murmur of mitral regurgitation is heard best at
the apex
Aortic regurgitation occurs in approximately 20% to 25% of patients with acute
rheumatic carditis, usually in combination with mitral regurgitation. Isolated aortic
regurgitation occurs in approximately 5% of patients with acute rheumatic carditis
Pericarditis occurs in approximately 4% to 11% of patients with acute rheumatic carditi

Erythema marginatum :
is a relatively uncommon finding, occurring in <5% of patients with RF
The
rash appears as a bright pink macule or papule that spreads with
serpiginous
borders and central clearing. The lesions are painless, not pruritic, blanch
on
pressure, and are usually macular rather than papular. Most commonly
seen
on the trunk or proximal extremities, the rash is evanescent and the
lesions
may change in appearance rapidly. A hot bath or shower may bring out or
accentuate the rash
Erythema marginatum is usually associated with carditis, and almost
never occurs as the sole major Jones criterion

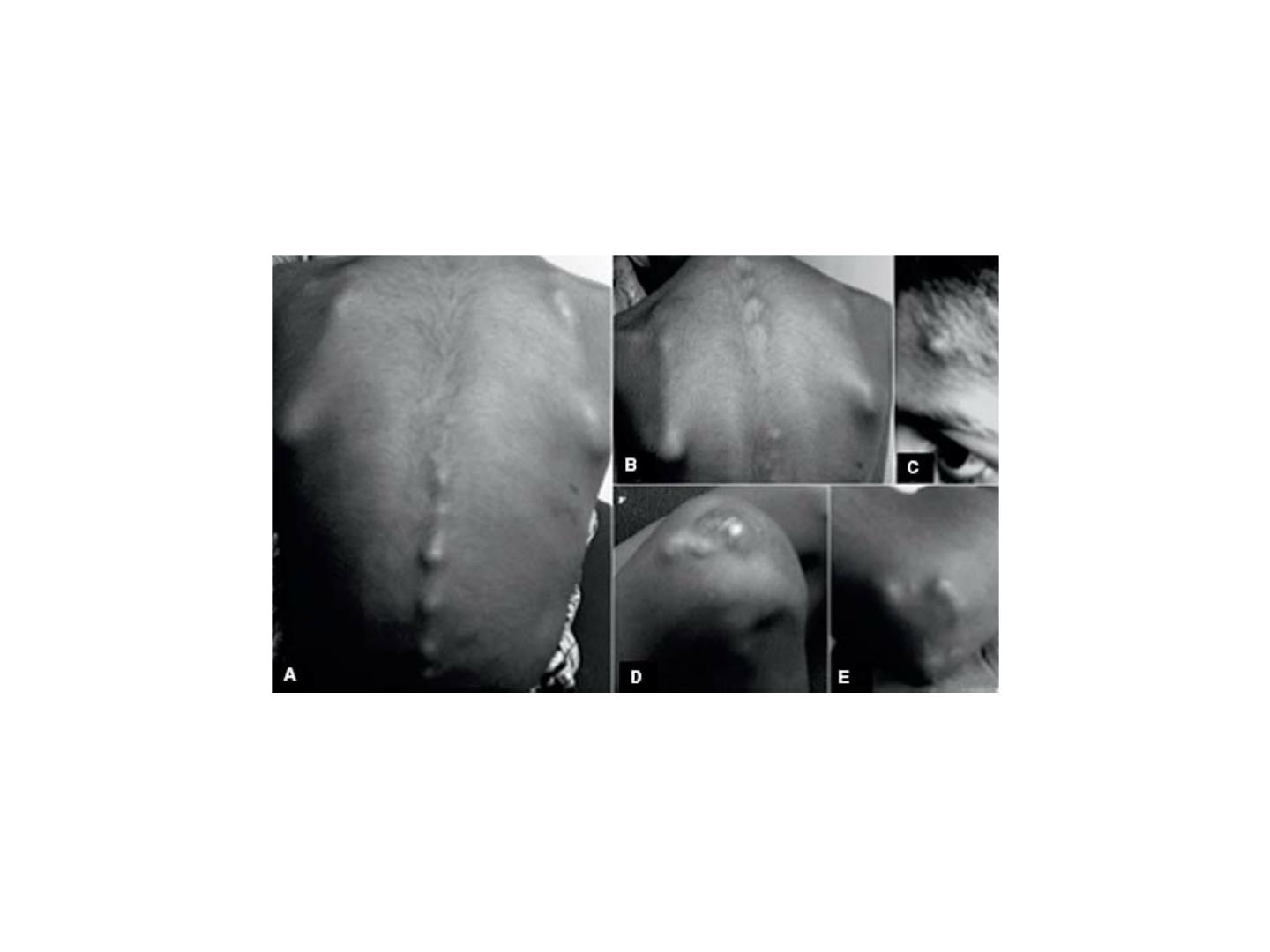
Subcutaneous Nodules
Subcutaneous nodules are relatively uncommon in RF, reported in 0% to 10%
of cases . They are not pathognomonic of RF, and may occur with systemic
lupus erythematosus or rheumatoid arthritis. The nodules are 0.5 to 2.0 cm
in diameter, round, firm, freely movable, nontender, with no evidence of
inflammation. They tend to occur in crops over extensor surfaces of joints or
bony prominences of the elbows, wrists, knees, ankles, scalp, spinous

Minor Criteria and Other Clinical Manifestations
The minor Jones manifestations are less specific than the major criteria
and include fevere , arthralgia, eleveated acute phase reactant
reactants, and first-degree AV block (prolonged PR interval) on ECG
elevated or rising antibody titers are more reliable evidence of a
preceding GAS infection. The titers most commonly measured are
antistreptolysin O (ASO) and antideoxyribonuclease B (anti-DNase
b). When a single antibody is measured, 80% to 85% of patients with
RF will have an elevated titer.

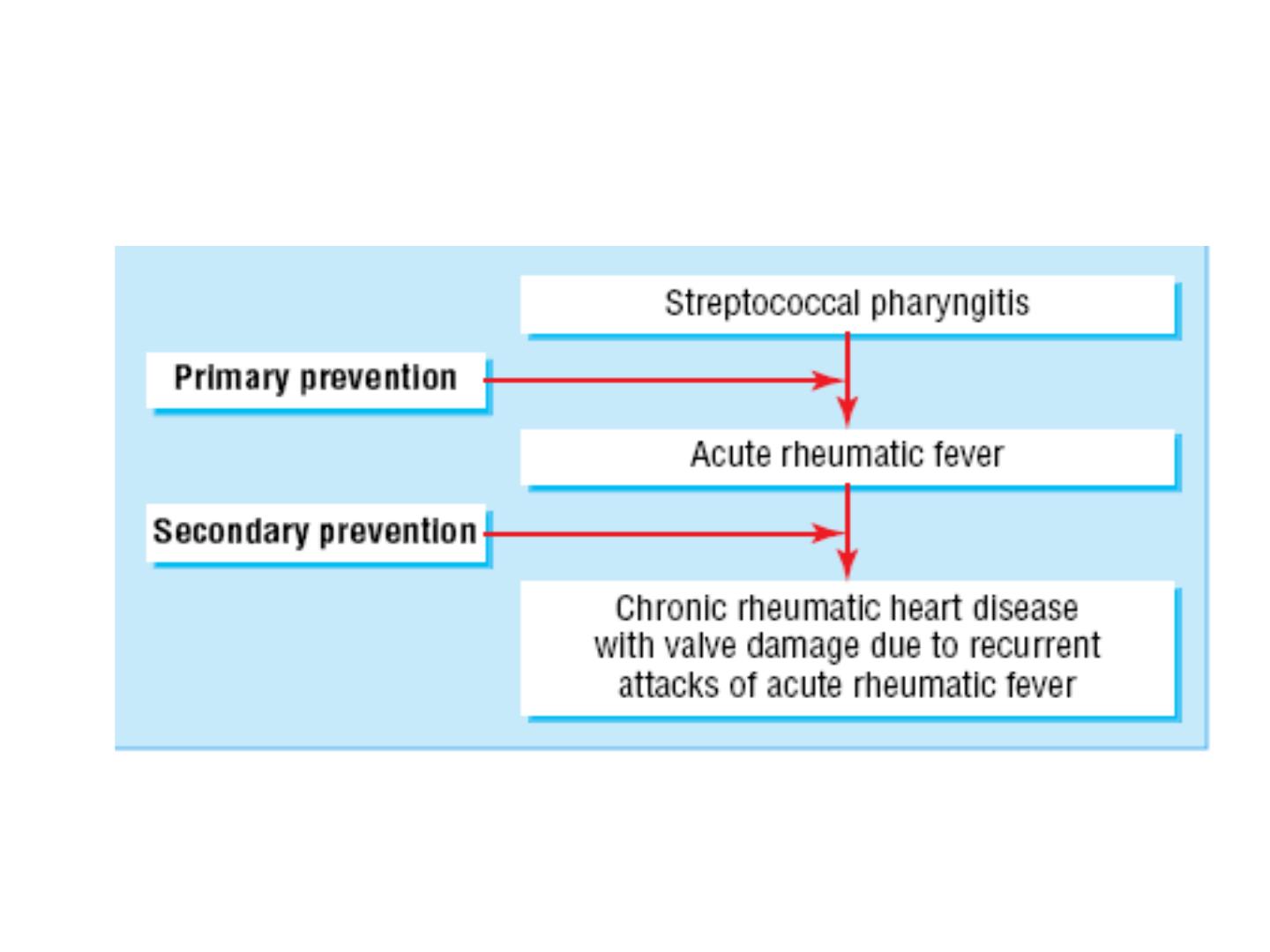
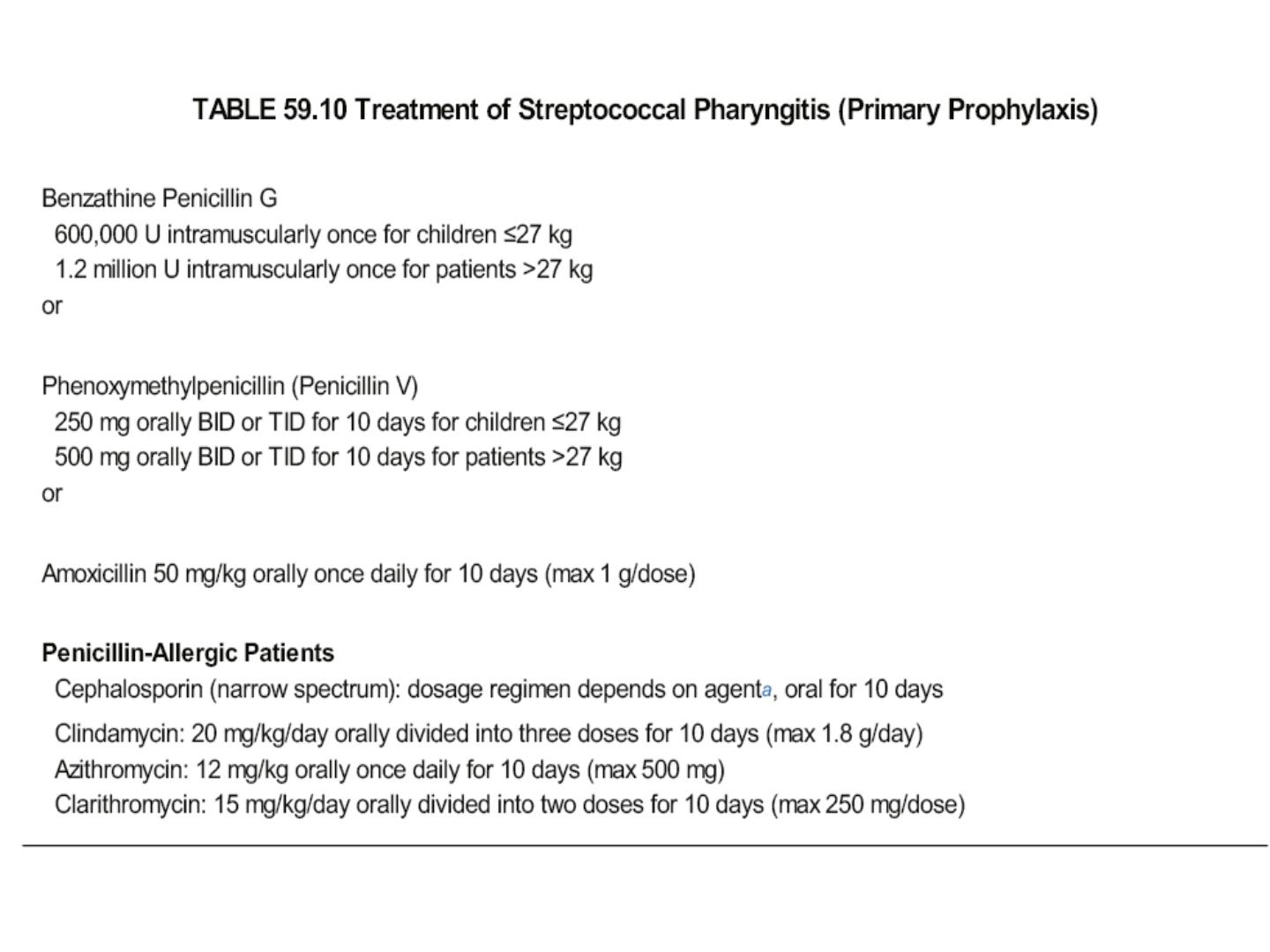
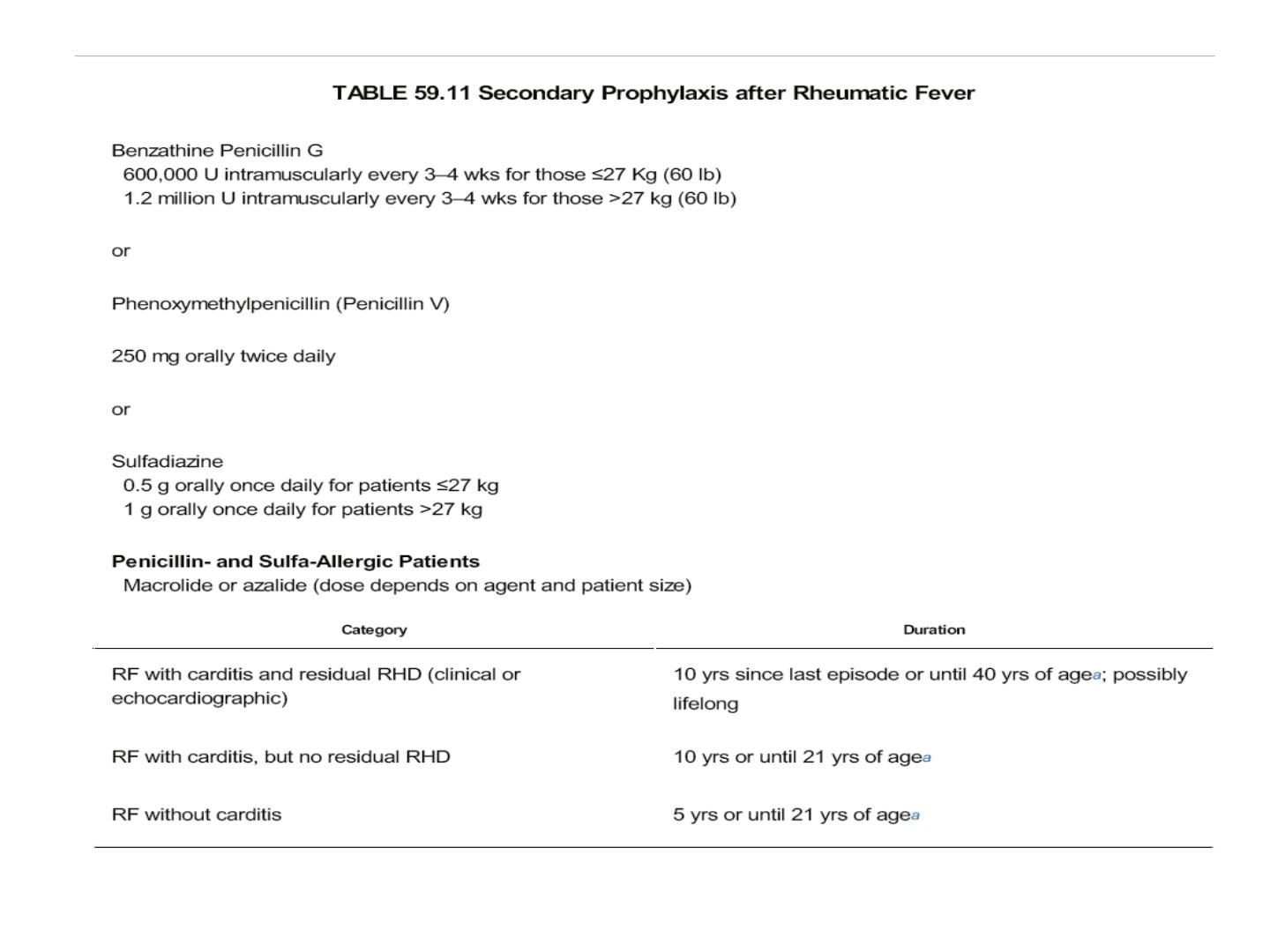
Medical Management of Acute RF
Management of acute rheumatic carditis should include antibiotic
treatment to eradicate pharyngeal streptococci, bed rest
antibiotic therapy is recommended even if the throat culture is negative.
aspirin at a dose of 80 to 100 mg/kg/day (doses as high as 4 to 6 g/day for
adults) for mild-to-moderate carditis. Salicylate levels should be
checked, aiming for serum concentrations of 20 to 30 mg/dL.
For patients with moderate-to-severe carditis and heart failure, many
recommend steroids (prednisone 2 mg/kg/day or equivalent) for ∼ 2
weeks, followed by tapering doses (reduce by 20% to 25% each week)
4 to 6 weeks while other recommend treatment until there is laboratory
evidence of resolution of the acute inflammatory process
(normalization of erythrocyte sedimentation rate and/or C-reactive
protein).

While some patients with heart failure improve, it should be emphasized that
for patients with severe valvular regurgitation and heart failure unresponsive
to medical therapy, surgical restoration of valvular
competence (repair or replacement) may be lifesaving
As previously stated, the arthritis of RF is typically very responsive to aspirin
within 48 to 72 hours.). The duration of anti-inflammatory treatment for
rheumatic arthritis can usually be guided by symptoms and response to
Therapy.
Most patients with chorea can be managed without pharmacologic treatment. In
cases with severe symptoms, reported treatments include phenobarbital,
haloperidol, valproic acid, corticosteroids, plasma exchange, and
intravenous immune globulin