
CARDIOVASCULAR SYSTEM
Blood Vessels:
Vascular disorders are responsible for more morbidity and
mortality than any other category of human diseases, arterial diseases
are the most important. This importance achieved from:
1- Narrowing vessels and this is producing ischemia of tissues perfused
by such vessels.
2- Damaging the endothelial lining and this is promoting intravascular
thrombosis, a process that contribute to critical ischemia of vital organs
such as the heart and brain.
3- Weakening the walls of vessels, predisposing to dilation or possibly
rupture.
4- Contributing to the pathogenesis of some of the most common
diseases in human as atherosclerosis, hypertension and diabetes.
Arterial Disorders
:
Arteriosclerosis:
-
Is the generic term for 3 pattern of vascular diseases, all of
which cause thickening and inelasticity of arteries:
(1) The dominant pattern is atherosclerosis .
(2) Monkeberg's medial calcific sclerosis characterized by calcification
in the media of muscular arteries.
(3) Arteriosclerosis which occurs in small vessels associated with
hypertension and diabetes mellitus.

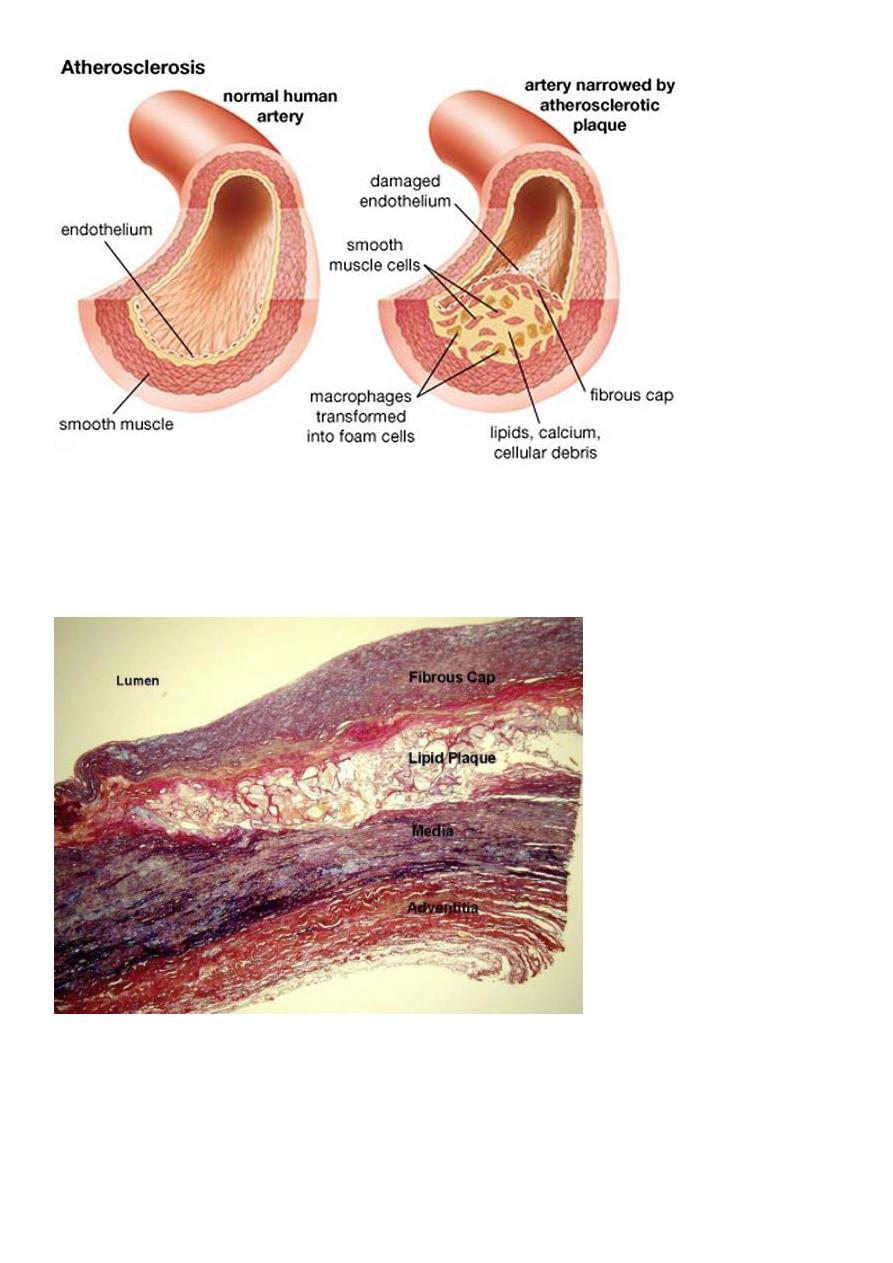
Atherosclerosis:-
It's characterized by intimal plaques called (atheroma) that
protrude into the lumen, weaken the underlying media and undergo a
series of complications as thrombosis so called
atherothrombotic
disease
.
Atherosclerosis alone accounts for more than half of all deaths in the
western world ,the disease begins in childhood and progress slowly
over the decades.
Risk factors:
-
Can be divided into constitutional factors and acquired factors which
are controllable.
(I) Constitutional factors:-
1- Age: between 40-60 years increasing the risk to five folds.
2- Sex: men are much more prone to atheroma and its consequences
than women that's because females hormones may be protective while
androgen may increase the risk of atheroma.
So that after menopause the frequency of myocardial infarction
decade of life.
th
and 80
th
becomes the same in both sexes by the 70
3- Familial predisposition: it's most likely polygenic and it may relate to
familial clustering of other risk factors, such as HT, DM and familial
hypercholesterolemia.
In other instances, it involves well defined hereditary genetic
derangement in lipoprotein deposition that result in high blood lipid
vessels.

(II) Acquired factors:-
Can be divided into major risk factors which include:-
1- Hyperlipidemia such as increased of LDL.
2- Hypertension.
3- Cigarette smoking.
4- Diabetes mellitus.
The less important risk factors are:-
1- Insufficient regular physical activity.
2- Obesity which regarded as independent risk factor.
3- Behavioral pattern & stress people who are aggressive and angry
particularly at risk
4- Diet habbit.
The multiple factors impose more than additive effect e.g. if 3 risk
factors are present as (hyperlipidemia, HT and smoking) the heart
attack rate 7 times greater than when none are present, but
atherosclerosis may develop in absence of any apparent risk factors.
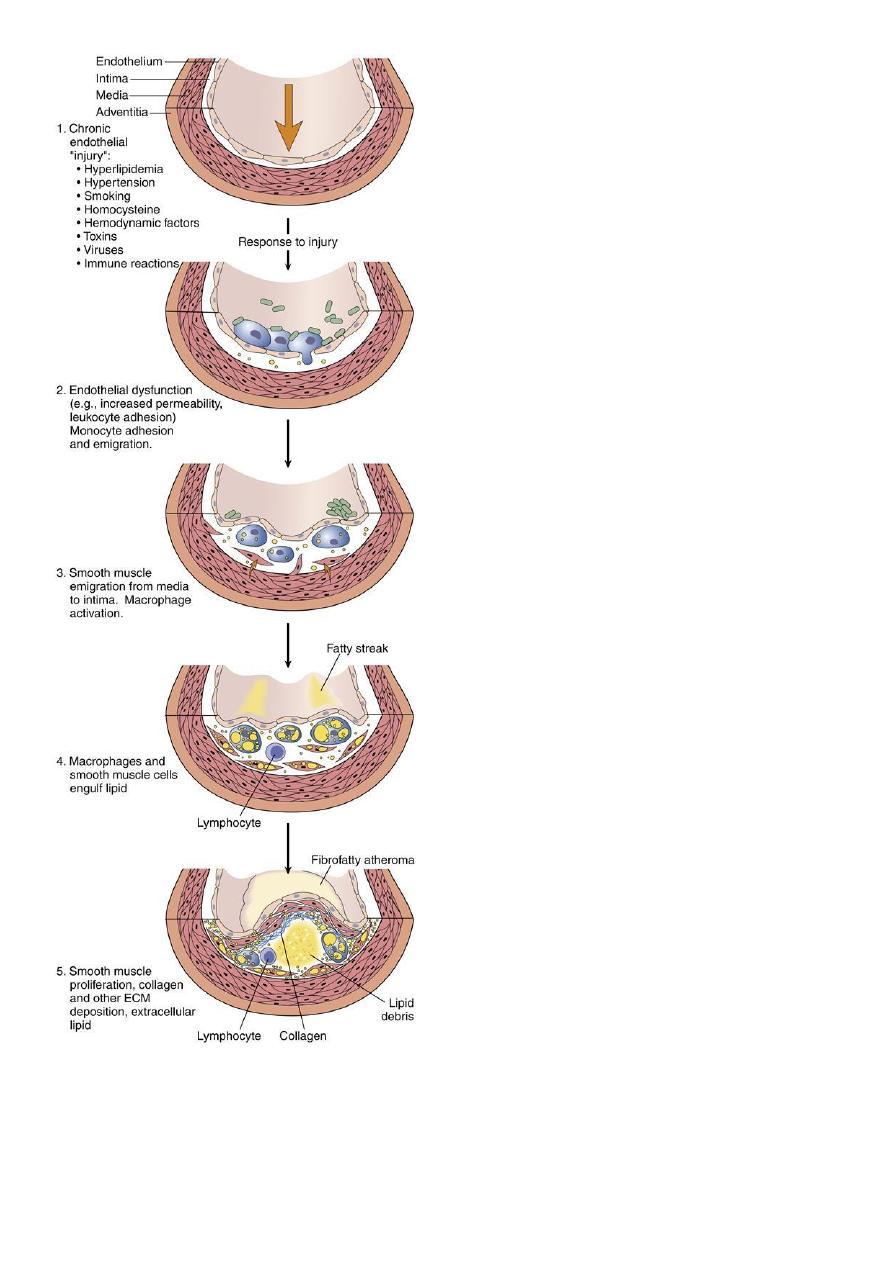
Pathogenesis:
-
These are a number of hypotheses for pathogenesis of
atherosclerosis, the most important one is response- to- injury
hypothesis which begins by chronic endothelial injury from
hyperlipidemia, HT, cigarette smoking, immune reaction,
haemodynamic factors, toxins and viruses, these factors cause
increased endothelial permeability to:-
1- Lipoproteins especially LDL or modified LDL.
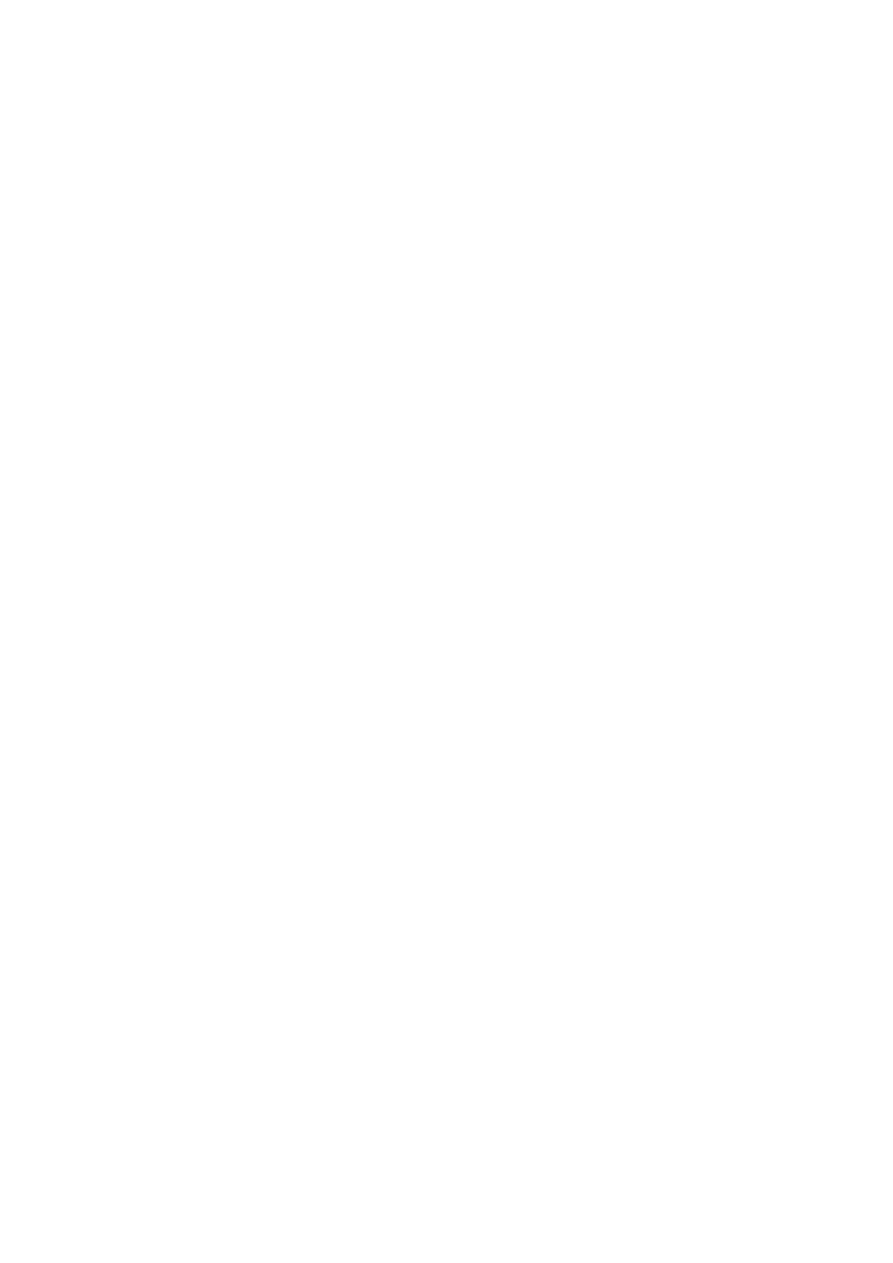
2- Circulating monocytes, leukocytes, T-lymphocytes and SMCs of
intimal or medial origin.
The monocytes after endothelial injury adhere and migrate between
ECs to localized subendothelially they transformed into macrophages
and engulf the lipoproteins to become foam cells, macrophages also
proliferate in the intima. If injury continue, platelets also adhere to the
endothelium. SMCs some of medial origin also migrate in the intima
and take present lipids to transform into foam cells, the accumulation
of these foamy cells appear macroscopically as fatty streaks, the SMCs
also synthesize collagen, elastin and glycoproteins to form mature
fibrofatty atheroma.
Thrombosis is a complication of late-stage atherosclerosis and
organization of thrombi may contribute to plaque formation, platelets
generally do not adhere to the arterial wall without severe injury of
endothelial cells, Where the foam macrophages and SMCs died the
released extracellular lipid and cellular debris which surrounded by
SMCs.
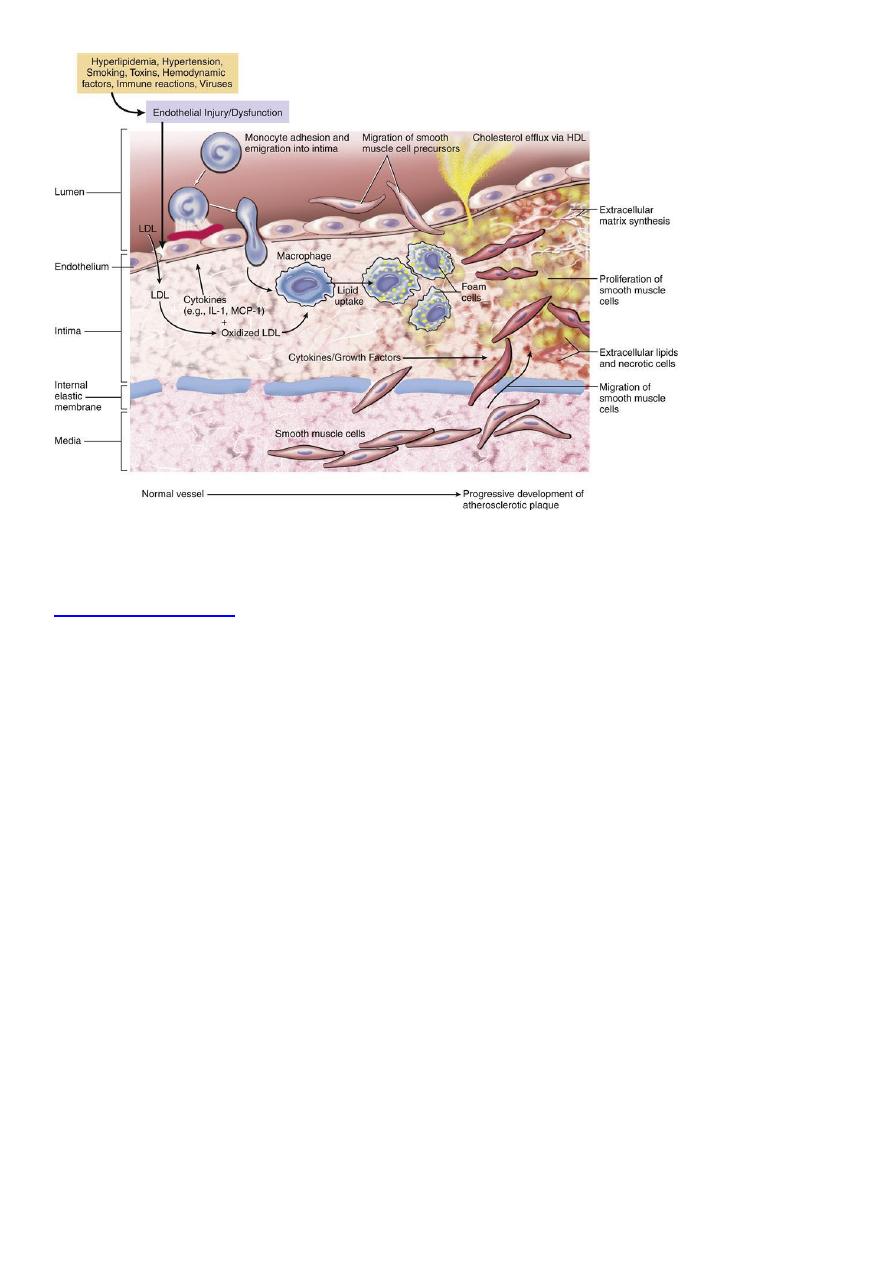
Morphology:-
-
:
Macroscopically
The atheroma plaque appearance depending on the content of
lipid, so it may be bright yellow if lipid content more, or grey if fibrous
tissue more.
-
The plaques have essentially 3 components:
-
:
Microscopically
1- Cells including vascular SMCs, blood derived
monocytes/macrophages and scattering of lymhpcytes.
2- Connective tissue fibers and matrix.
3- Lipids.
Some plaques contain relatively small amounts of lipids and are
composing almost entirely of connective tissue cells from fibrous
plaque.
The extracellular lipid core composed of cholesterol (which forms
needle-like crystals).
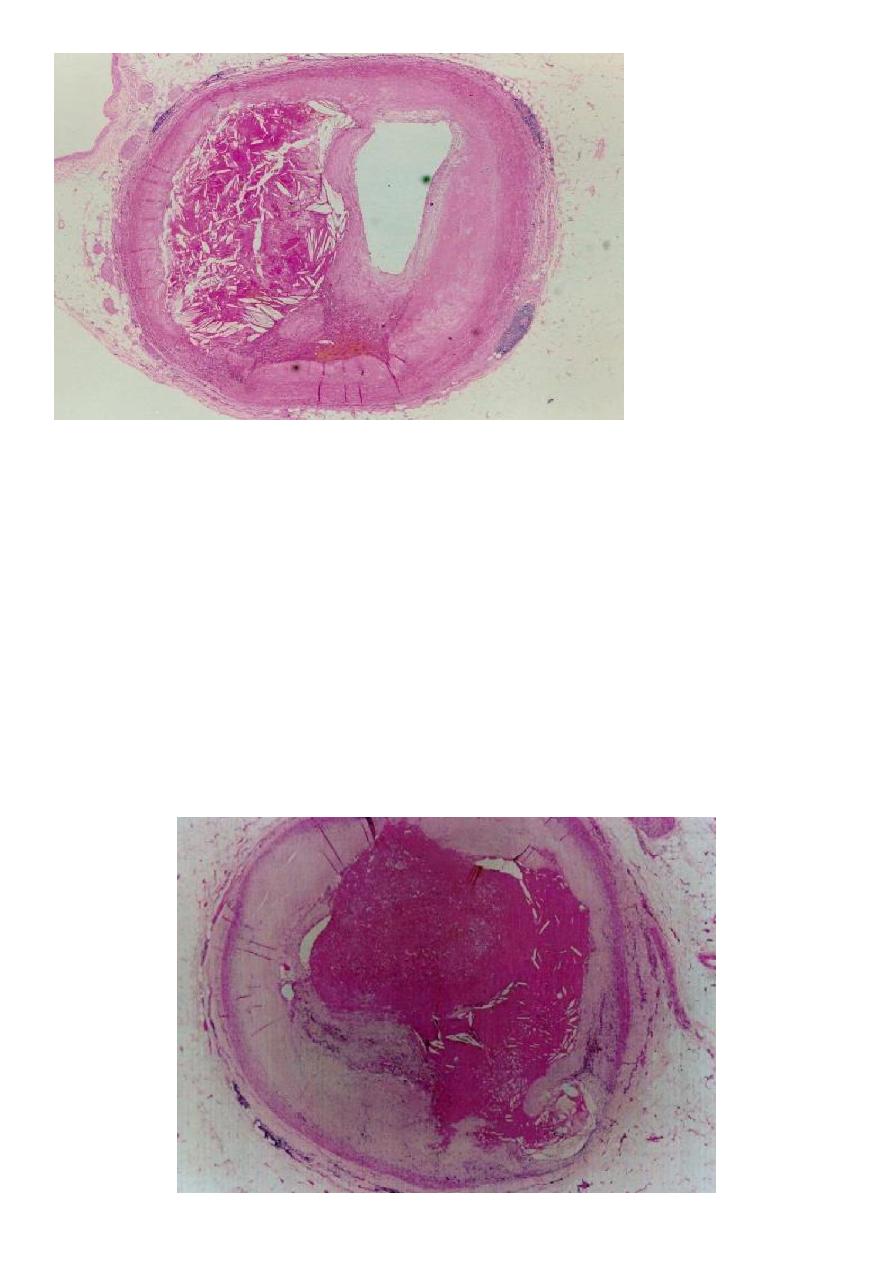
Plaques may develop
4 complications
, these are:-
1- Ulceration.
2-
thrombosis
.
3-intraplaque hemorrhage
.
4-
total occlusion
.
Hypertension and hypertensive vascular disease:
-
Hypertension is associated with both functional and pathologic
alteration , it's a common disease and important risk factor in ischemic
heart disease, CVA and congestive heart failure.
Vascular pathology in hypertension:-
Hypertension is associated with 2 forms of small blood vessels disease:
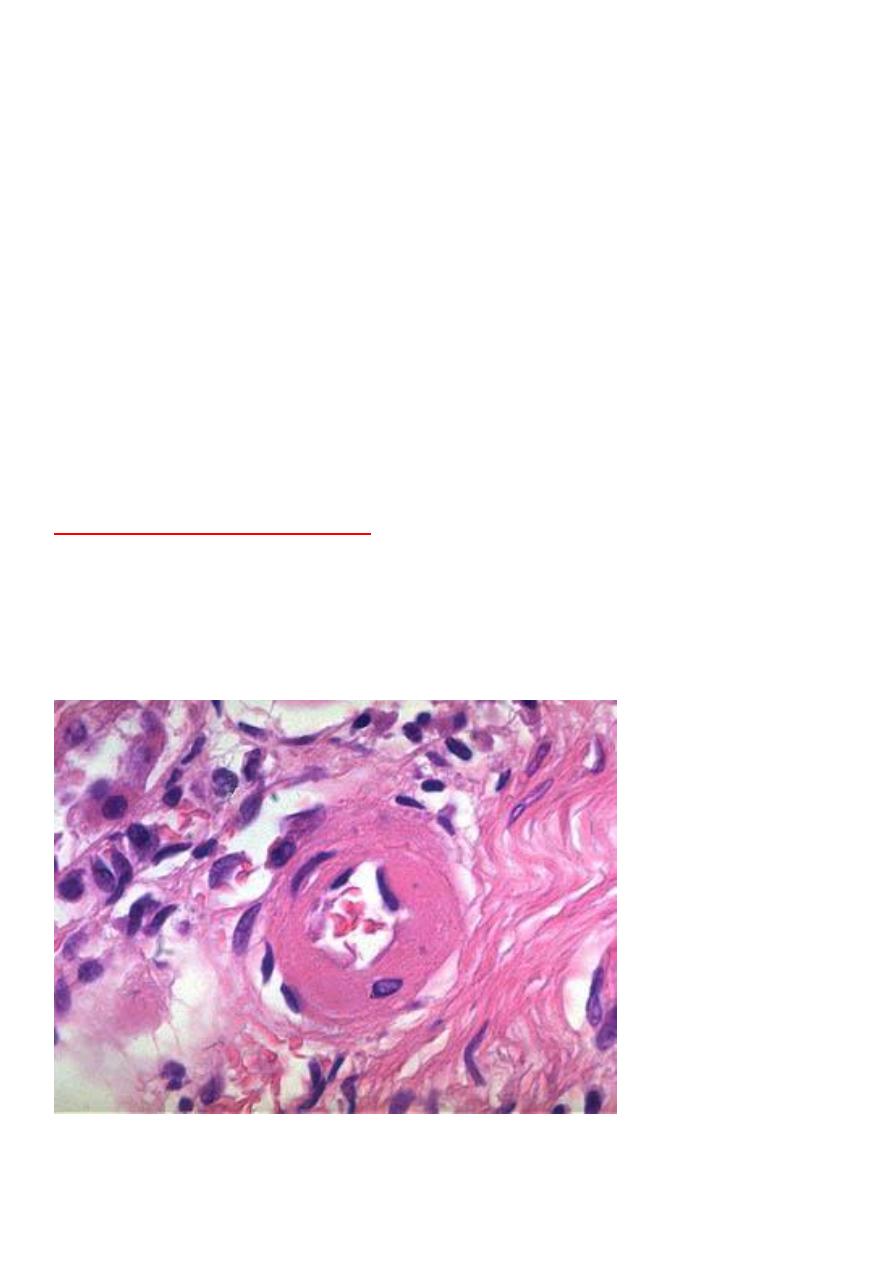
1- Hyaline arteriolosclerosis.
2- Hyperplastic arteriolosclerosis.
-
Hyaline arteriolosclerosis:
-
1
the wall is consisting of homogenous, pink, hyaline thickening of the
walls of arterioles with narrowing of the lumen.
-
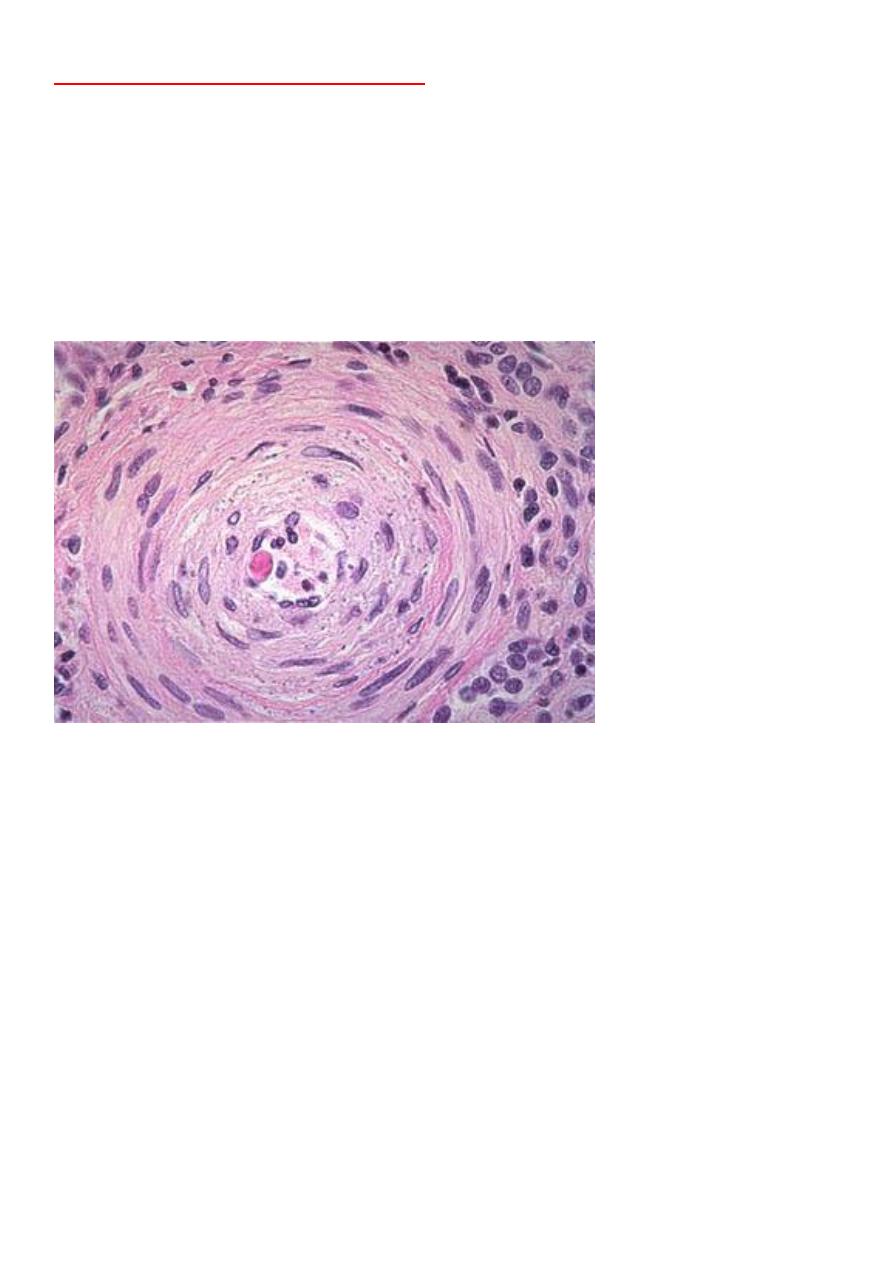
Hyperplastic arteriolosclerosis:
-
2
this type seen in light microscope by its concentric laminated, onion
like, thickening of the lumen, there is hypertrophy and hyperplasia of
vascular SMCs and thickening of basement membrane.
