
[1]
Malignant tumor of the urinary bladder
(ca bladder)
Incidence
The male-female ratio is 3-1
*Ca bladder is the 2nd most common cancer of the genitourinary
tract.
*The average age at diagnoses is 65yr.
*at the time of diagnosis approximately 75% of the bladder ca.
are localized to the bladder & 25% have spread to regional lymph
node or distant sites.
Risk factors & pathogenesis
1-Cigarette smoking.
Smokers have 2-6 fold increase risk of bladder ca. than non
smokers.
Smoking is causative factor in up to 50% in men
The causative agents beta naphthylamine which are secreted
into the urine of smokers.
2-Occupational exposures.
Pt who expose to organic chemical as aromatic amines, aniline
dyes, B-naphthylamine,

[2]
usually include people work in chemical, dye, rubber, petroleum,
leather, & printing industries are at increased risk.
3-Cyclophosphamide (cytoxane).
Drug used for management of various malignant diseases is also
increase risk of ca bladder.
4- Physical trauma to the urothelium
induced by chronic infection (schistomiasis), instrumentation, &
calculi increase risk of malignancy.
5-diet: In general, a Mediterranean diet has the lowest urothelial
cancer risk due to the increased ingestion of fruits and vegetables
specifically citrus, apples, tomatoes, carrots
6-Genetic changes
include activation of oncogenes & loss or inactivation of tumor
suppressor genes.
-loss of chromosome 9 appear to be consistent finding in all stages
&grades of ca bladder. Suggest early events in ca bladder
development.
-More recent studies examining p53 tumor suppressor
gene mutations in primary, recurrent, and upper
tract tumors suggest that these tumors can have a single clonal
origin
Staging.
CIS—carcinoma in situ.
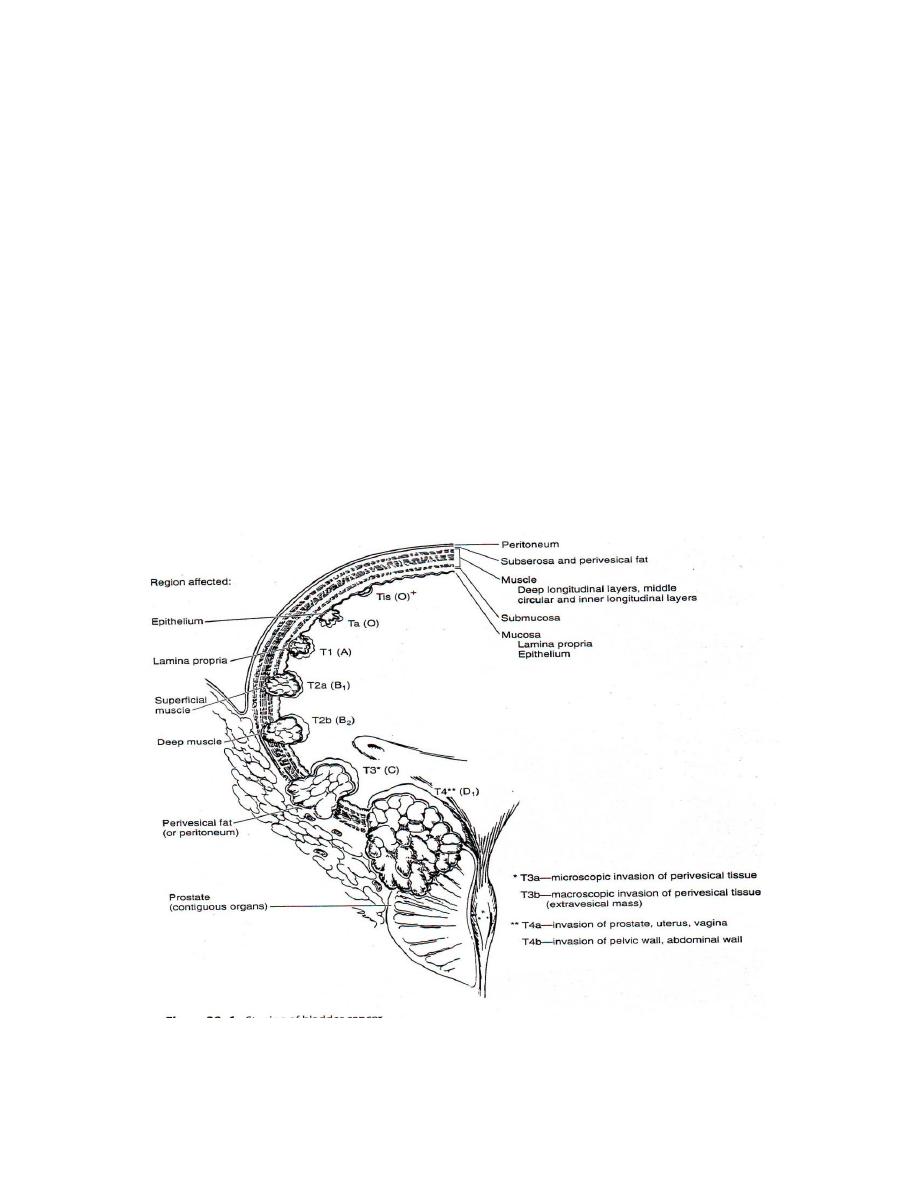
[3]
Ta—epithelium not involve the lamina propria.
T1—reaching the lamina propria.
T2a—superficial detrusor muscle.
T2b—deep detrusor muscle.
T3a—microscopic invasion of perivesical tissue.
T3b—macroscopic invasion of perivesical tissue. Extravesical
mass.
T4a—invasion of prostate, uterus, &vagina.
T4b—invasion of pelvic wall, abdominal wall.
*superficial tumor—CIS, Ta, T1, T2a.

[4]
*deep tumor—T2b, T3.
Tumor grading.
G1—well differentiated.
G2—moderately well differentiated.
G3—poorly differentiated.
G4—undifferetiated.
Histopathology
Ninety-eight percent of all bladder cancers are epithelial
malignancies, with most being transitional cell carcinomas (TCCs).
A. NORMAL UROTHELIUM
The normal urothelium is composed of 3–7 layers of transitional
cell epithelium resting on a basement membrane
Beyond the basement membrane is loose connective tissue, the
lamina propria,in which occasionally smooth-muscle fibers can be
identified.
These fibers should be distinguished from
deeper, more extensive muscle elements.
The muscle wall of the bladder is composed
of muscle bundles coursing in multiple directions.
As these converge near the bladder neck, 3 layers can be
recognized: inner and outer longitudinally oriented layers and a
middle circularly oriented layer.

[5]
B. PAPILLOMA
papillary tumor with a fine fibrovascular stalk
Papillomas usually occurring in younger patients.
C. TRANSITIONAL CELL CARCINOMA
Approximately 90% of all bladder cancers are TCCs.
*Carcinoma in situ (CIS) is recognizable as flat, anaplastic
epithelium.
D. NONTRANSITIONAL CELL CARCINOMAS
1. Adenocarcinoma
<2% of all bladder cancers.They are mucus-secreting and may
have glandular
2. Squamous cell carcinoma
5% and 10% of all bladder cancers in the United States and is often
associated with a history of chronic infection, bilharzial infection,
vesical calculi, or chronic catheter use.
It is the most common type in eagpt and causing higher mortality
rate in that countery
3. Undifferentiated carcinomas
rare (accounting for <2%), have no mature epithelial elements.
4. Mixed carcinoma—

[6]
4–6% of all bladder cancers and are composed of a combination
of transitional, glandular, squamous, or undifferentiated
patterns.
Clinical features
1-Hematuria is the presenting symptom in 85-90% of pt. with ca
bladder.
Usually intermittentand painless except if accompany by
infection may be gross or microscopic.
2-Frequency, urgency & dysuria may accompany the hematuria.
Irritative voiding symptoms more common in pt with CIS.
3-Passing clot or necrotic tumor perurethra.
4-Suprapubic mass.
5-Obstructive uropathy.
6-Distant metastasis.
usually symptoms of advanced disease include bone pain or flank
pain
Investigations
*GUE & urine cytology
Usually reveal RBC in urine. Pyuria may be due to concomitant
infection.
*Hematology
-Anemia, due to chronic blood loss or invasion of bone marrow.
[7]
-Increase b.urea & s.creatine
*Radiology
-Ultrasonography.
-IVU (filling defect in the bladder with or without hydronephrosis)
-CT & MRI may be used to characterized the extent of the tumor
& detect lymph nodes
*Cystourethroscopy & tumor resection
The diagnosis and initial staging of bladder cancer is made by
cystoscopy and transurethral resection (TUR).
Treatment
A-Superficial bladder tumor
1-Transurethral resection + intravesical Immunotherapy or
chemotherapy (most common used).
2-Partial cystectomy.
3-Radical cystectomy.
Radical cystectomy may indicated in superficial tumor if its
1-extensive, multiple superficial or large intracavity tumor.
2-high grade tumor, grade 3 & above
3-rapidly recurring tumor after resection, or recurring in high
grade.

[8]
4-tumor anamenable to endoscopic resection eg tumor in the
anterior wall.
B-Deep bladder tumor
Usually treated by partial or radical cystectomy.
Partial cystectomy is indicated in cases in which the tumor is
single & located at the dome or fundus of the urinary bladder or
at the lateral wall of the bladder which permit resection of 1-2
cm of normal tissue around the tumor
Radical cystectomy
in male—include removal of bladder with its covering peritoneum
& extrvesical fat, prostate, seminal vesicle &membranous
urethra.
In female—removal of the bladder with its covering peritoneum
& extravesical fat, both ovaries, fallopian tubes, uterus, cervix,
&anterior vaginal vault.
Radiotherapy.
Is an alternative to radical cystectomy in patients with
1-deeply infiltrating bladder cancer which is beyond surgery.
2-patients who are poor surgical candidates.
Treatment generally well tolerated but unfortunately local
recurrence is common.



