
1
Epidemiology and control of communicable diseases
Epidemiology and Control of Malaria
L13
Malaria
What is Malaria?
Malaria is a parasitic disease caused by sporozoa of the genus plasmodium.
Four species of parasites:
P. Falciparum, P. Vivax, P. Malariae, P. Ovale.
Arthropod hosts are female anopheles mosquitoes (vector of malaria).
Extent of Malaria
-
An estimated 225 million cases of malaria worldwide in 2009.
-
665,000 people died from malaria in 2010 accounting for 2.23% of deaths
worldwide.90% of malaria-related deaths occurring in Subsaharan Africa, with about
60% of deaths being children under 5 years of age.
-
In 2015, 95 countries and territories had ongoing malaria transmission and an estimated
3.2 billion people – nearly half the world’s population – were at risk of malaria.
Global disease burden in 2015
-
There were an estimated 214 million cases of malaria worldwide in 2015, and an
estimated 438 000 deaths. Approximately 90% of all malaria deaths occur in Africa.
-
In 2015, an estimated 292 000 African children died before their fifth birthday due to
malaria. Globally, the disease caused an estimated 306 000 under-five deaths in 2015.
-
Between 2000 and 2015, an expansion of malaria interventions helped to reduce malaria
incidence by 37% globally, and by 42% in Africa.
-
During the same period, malaria mortality rates decreased by an estimated 60%
worldwide and by 66% in Africa. In the under-five age group, mortality rates have
declined by 65% globally, and by 71% in Africa.
2
-
Other regions have achieved impressive reductions in their malaria burden. Since 2000,
the malaria mortality rate declined by 72% in the Region of the Americas, by 65% in the
Western Pacific Region, by 64% in the Eastern Mediterranean Region and by 49% in the
South-East Asia Region. In 2015, for the first time, the European Region reported zero
indigenous cases of malaria.
-
Children, pregnant women, people with splenectomy, and non immune persons are at
risk of severe infection.
-
Clinically: marked by attacks of chills ,fever ,and sweating occurring at intervals that
depend on the time required for development of a new generation of parasites in the
body ..
-
Deaths usually due to anaemia, cerebral malaria, and metabolic acidosis.
Global Health Observatory (GHO)
Cases
214 million malaria estimated cases worldwide in 2015
Incidence
37% global decrease in malaria incidence between 2000 and 2015
Mortality
60% estimated decrease in global malaria deaths between 2000 and 2015
Incubation period
I.P. = 7 – 30 days
P. Falciparum 7-14 days
P. Vivax & Ovale 8-14 days
P. Malariae 7-30 days
Period of communicability
Untreated or insufficiently treated patients: may be a source of infection as long as
gametocytes are present in the blood)
The mosquito remains infective for life.
Blood transfusion: as asexual forms remain in the circulating blood.
Stored blood: remains infective at least a month.
3
Epidemiology of Malaria
1. Epidemic malaria:
Great fluctuation occurs from time to time
2. Endemic malaria:
Constant presence of infection without great fluctuation
a. Endemic malaria with low epidemic potential (Stable malaria): Transmitted by
Anthropophilic mosquitoes with long life expectancy. continuous transmission of
infection leads to development of immunity among adults. Children mainly affected.
Epidemic is unlikely. The disease is maintained by small number of mosquitoes.
b. Endemic malaria with high epidemic potential (Unstable malaria):
- Transmitted by zoophilic mosquitoes with short life expectancy.
-
Low transmission rate
-
Low immunity
-
Variation in endemicity
-
Risk of epidemic
Factors determining the epidemiology of malaria
1. Environmental factors:
Temperature, humidity, rainfall, and altitude all affect transmission of malaria.
-
P. falciparum requires a minimum temperature of 20
o
C to develop in female
mosquito.
-
A relatively high humidity is required for survival of adults vectors.
-
Rainfall is essential for breeding sites.
-
Global warming presents a risk for serious epidemics.
2. Vector factors:
These are behavioral factors of vectors
-
Some species are anthropophilic,
-
Others are zoophilic,
-
Some prefer to bite indoor, others outdoors.
-
Malaria vectors bite between dusk and dawn.
4
3. Parasite factors:
-
Prepatency period is shortest in p. falciparum and longest in p. malariae.
-
Relapse: in p.vivax & ovale relapse occurs because of presence of intrahepatic parasites
with retarded development. For p. falciparum & p. malariae; when parasitological cure
has not been achieved.
4. Host factors:
Genetic factors:
Several genetic factors may protect against severe disease and mortality from p.
falciparum. These include: HbS heterozygote, α- thalassemia homo & hetrozygotes, β-
thalassemia heterozygote, and G6PD, absence of Duffy antigen, and ovalocytosis.
Immune factors:
-
Infants borne to immune mothers are partially protected from clinical malaria for 4-6
months because of passive immunity and high level of HbF.
-
At about 6 months – 5 years children are susceptible to severe attacks, then become less
frequent, the substantial immunity persists throughout life later.
Nutritional factors:
The influence of nutrition on malaria is complex. There is good evidence that severe
malnutrition may be antagonistic to malaria, while mild to moderate malnutrition is a risk
factor for severe malaria.
Behavioral factors:
-
Uncontrolled urbanization
-
Population movement
-
Mining , agriculture of cotton, sugar cane & rice.
-
Behavioral patterns are influenced by cultural, ethnic, and religious background.
-
Late night and outdoor activities increase biting opportunities for mosquitoes.
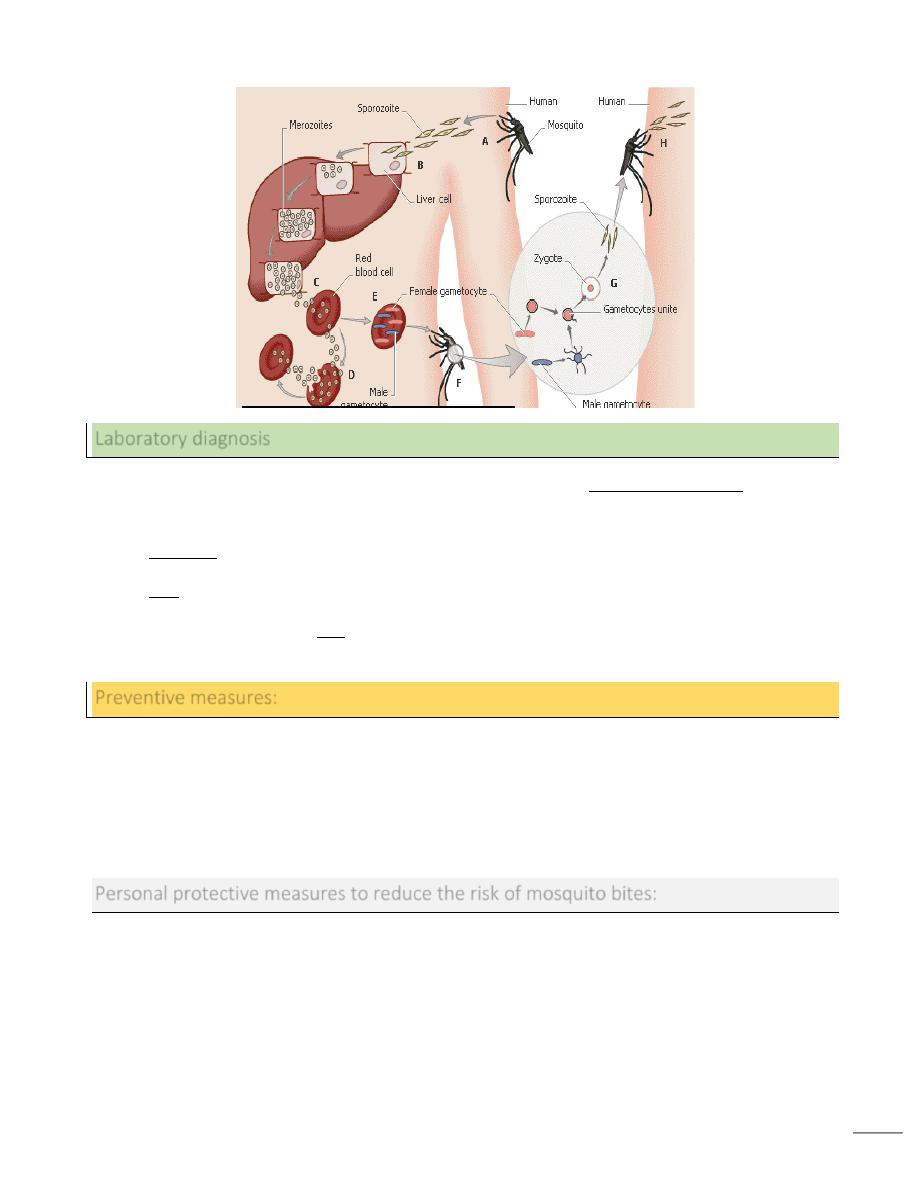
Mode of transmission
Bite of infective female anopheles mosquito.
By injection or transfusion of blood from infected person.
Trans-placental congenital transmission.
5
Laboratory diagnosis
Demonstration of malaria parasites in blood film (thick blood smear). repeated
microscopical examination every 12-24 hours.
Dipsticks that detect circulating plasmodial antigens in blood.
PCR is a most sensitive method, but it is a specialized assay not generally available.
Ab demonstration by IFA or other tests, may appear after the first week of infection, but
may persist for years (indicate past malarial infection)
Preventive measures:
o Personal protective measures against mosquito biting
o Chemoprophylaxis
o Control of vector:
-
Elimination or reduction of anopheles mosquito breeding habitats.
-
Use of residual insecticides against adults anopheles vectors
Personal protective measures to reduce the risk of mosquito bites:
o Avoid going out between dusk and dawn.
o Apply insect repellent to exposed skin.
o Stay in well constructed and maintained building.
o Use screens over doors and windows.
o Use mosquito nets over the bed.
o Use anti-mosquito spray or insecticides

6
Chemoprophylaxis:
o For non-immune travelers to endemic areas of chloroquine sensitive infection:
chloroquine 300 mg base once weekly started 1-2 weeks before travel, continued weekly
during travel, and for 4 weeks after return.
o For travelers to endemic areas of chloroquine resistant infection: mefloquine 5 mg /kg/
week (same as chloroquine) or Doxycycline 100 mg daily is an alternative regimen,
started 1-2 days before travel, continued daily till 4 weeks after leaving the area.
o When mefloquine or doxycycline are not recommended: Fansidar (sulfadoxine
500mg/pyrimethamine 25 mg) or Primaquine (0.5 mg/kg/day) starting on first day of
exposure and for 1 week after leaving the area.
Malaria in pregnancy:
Malaria in pregnant women increases the risk of maternal death, abortion, stillbirth, and
neonatal death.
Chloroquine
(5mg/kg/week) and
Proguanil(
3mg/kg/day) should be taken for prophylaxis. They can be taken during the first
3 months of pregnancy.
Mefloquine
(5mg/kg/week) may be started but from the 4th month of pregnancy.
Doxycycline
prophylaxis should not be given to pregnant women, but to women of
childbearing age. Pregnancy should be avoided for one week after stopping the drug.
Assistant professor D. Ali Abid Saadoon
Mubark A. Wilkins
