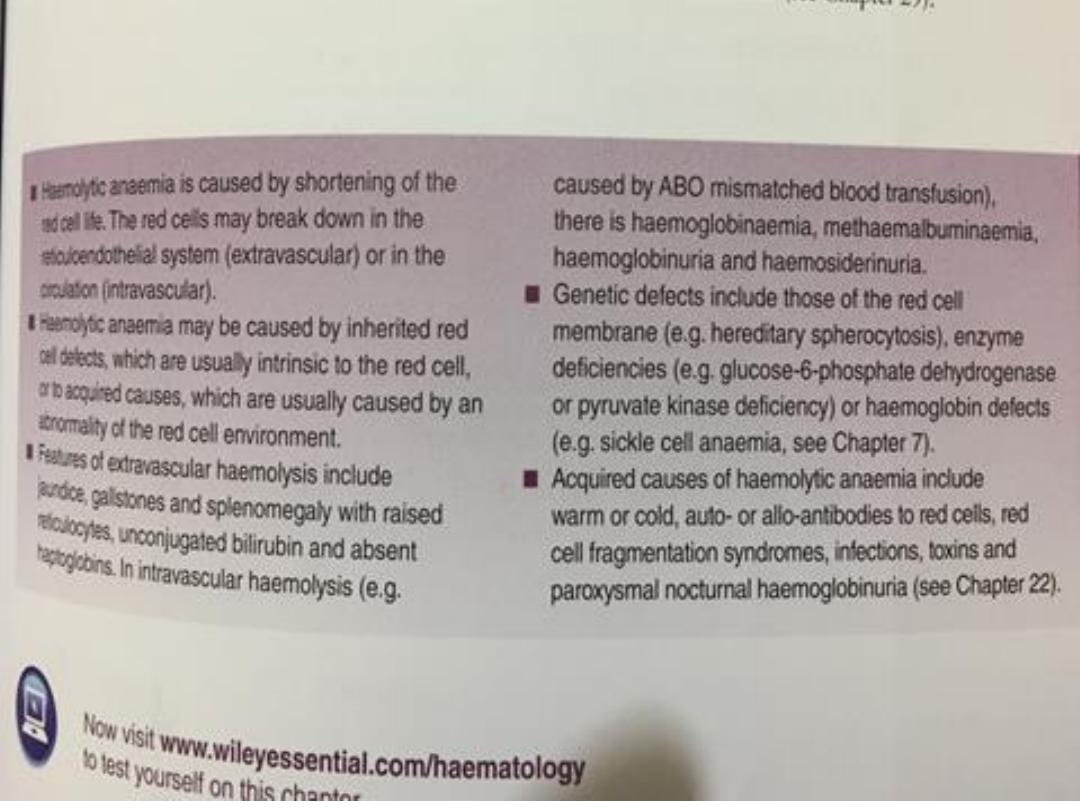
Hemolytic anemia

HEMOLYTIC ANEMIA
• Anemia of increased destruction
1. Normochromic, normochromic anemia
2. Shortened RBC survival
3. Reticulocytosis - Response to increased RBC destruction
4. Increased indirect bilirubin
5. Increased LDH
• HEMOLYTIC anemia testing
1. Absent haptoglobin
2. Hemoglobinuria
3. Hemoglobinemia

HEMOLYTIC ANEMIA Causes
• INTRACORPUSCULAR HEMOLYSIS
1. Membrane Abnormalities
2. Metabolic Abnormalities
3. Hemoglobinopathies
• EXTRACORPUSCULAR HEMOLYSIS
1. Nonimmune
2. Immune

Autoimmune haemolytic anaemia
• This results from increased red cell destruction due to red cell
autoantibodies. The antibodies may be IgG or M, or more rarely
IgE or A. If an antibody avidly fixes complement, it will cause
intravascular haemolysis, but if complement activation is weak,
the haemolysis will be extravascular.
• Antibody-coated red cells lose membrane to macrophages in the
spleen and hence spherocytes are present in the blood. The
optimum temperature at which the antibody is active (thermal
specificity) is used to classify immune haemolysis:
• Warm antibodies bind best at 37°C and account for 80% of cases.
The majority are IgG and often react against Rhesus antigens.
1. Primary (idiopathic)
2. Secondary (occurring in association with an underlying disorder
such as SLE, lymphoma, chronic lymphocytic leukemia or after
use of certain drugs)

• Cold antibodies bind best at 4°C but can bind up to
37°C in some cases. They are usually IgM and bind
complement. To be clinically relevant, they must act
within the range of normal body temperatures.
They account for the other 20% of cases.
• Infections (especially mycoplasmal pneumonias or
infectious mononucleosis) ,Lymphoproliferative
disorders ,
Idiopathic

Warm autoimmune haemolysis
• The incidence of warm autoimmune haemolysis is
approximately 1/100 000 population per annum; it
occurs at all ages but is more common in middle
age and in females.
Investigations
• There is evidence of haemolysis and spherocytes on
the blood film. The diagnosis is confirmed by the
direct Coombs or antiglobulin test
•

Management
• If the haemolysis is secondary to an underlying cause, this must be
treated and any implicated drugs stopped. It is usual to treat
patients initially with prednisolone 1 mg/kg orally. A response is
seen in 70–80% of cases but may take up to 3 weeks; a rise in
haemoglobin will be matched by a fall in bilirubin, LDH and
reticulocyte levels.
• Transfusion support may be required for lifethreatening problems,
such as the development of heart failure or rapid unabated falls in
haemoglobin.
The least incompatible blood should be used but this may still give
rise to transfusion reactions or the development of alloantibodies.
• About two-thirds of patients respond to corticosteroid treatment.
In patients who relapse after corticosteroid cessation or who are
refractory to corticosteroids, rituximab is usually used as a second-
line drug.

• Other treatments include use of additional
immunosuppressive drugs and/or splenectomy.
About one third to one half of patients have a sustained
response after splenectomy.
• In cases of fulminant hemolysis, high-dose pulse
corticosteroids can be used.
• For less severe but uncontrolled hemolysis, immune
globulin infusions have provided temporary control.
• Long-term management with immunosuppressants
(including cyclosporine) has been effective in patients
in whom corticosteroids and splenectomy have been
ineffective.
Cold agglutinin disease
• This is due to antibodies, usually IgM, which bind to the
red cells at low temperatures and cause them to
agglutinate. It may cause intravascular haemolysis if
complement fixation occurs.
• Chronic cold agglutinin disease This affects elderly
patients and may be associated with an underlying low-
grade B cell lymphoma. It causes a low-grade
intravascular haemolysis with cold, painful and often
blue fingers, toes, ears or nose (so-called acrocyanosis).
•

Paroxysmal cold hemoglobinuria
• Paroxysmal cold hemoglobinuria (PCH; Donath-Landsteiner
syndrome) is a rare type of cold agglutinin disease. PCH is
more common in children. Hemolysis results from exposure
to cold, which may even be localized (eg, from drinking cold
water, from washing hands in cold water). An IgG antibody
binds to the P antigen on RBCs at low temperatures and
causes intravascular hemolysis after warming.
• It occurs most often after a nonspecific viral illness or in
otherwise healthy patients, although it occurs in some
patients with congenital or acquired syphilis..
• The severity and rapidity of development of the anemia
varies and may be fulminant.
In children, this disease is often self-resolving

TREATMENT OF COLD AGGLUTININ
• Treatment is directed at any underlying lymphoma but
if the disease is idiopathic, then patients must keep
extremities warm, especially in winter.
• In many cases, avoidance of cold environments and
other triggers of hemolysis may be all that is needed to
prevent symptomatic anemia.
• In cases associated with a lymphoproliferative disease,
treatment is directed at the underlying disorder.
• Rituximab is commonly used, and chemotherapy
regimens used to treat B-cell cancers can be effective.
• In severe cases, plasmapheresis is an effective
temporary treatment.
• Transfusions should be given sparingly, with the blood
warmed through an on-line warmer.
Splenectomy is usually of no value. and
immunosuppressants have only modest effectiveness.
Paroxysmal cold hemoglobinuria
• In PCH, therapy consists of strict avoidance of exposure
to cold. Immunosuppressants have been effective, but
use should be restricted to patients with progressive or
idiopathic cases.
• Splenectomy is of no value.
• Treatment of concomitant syphilis may cure PCH.

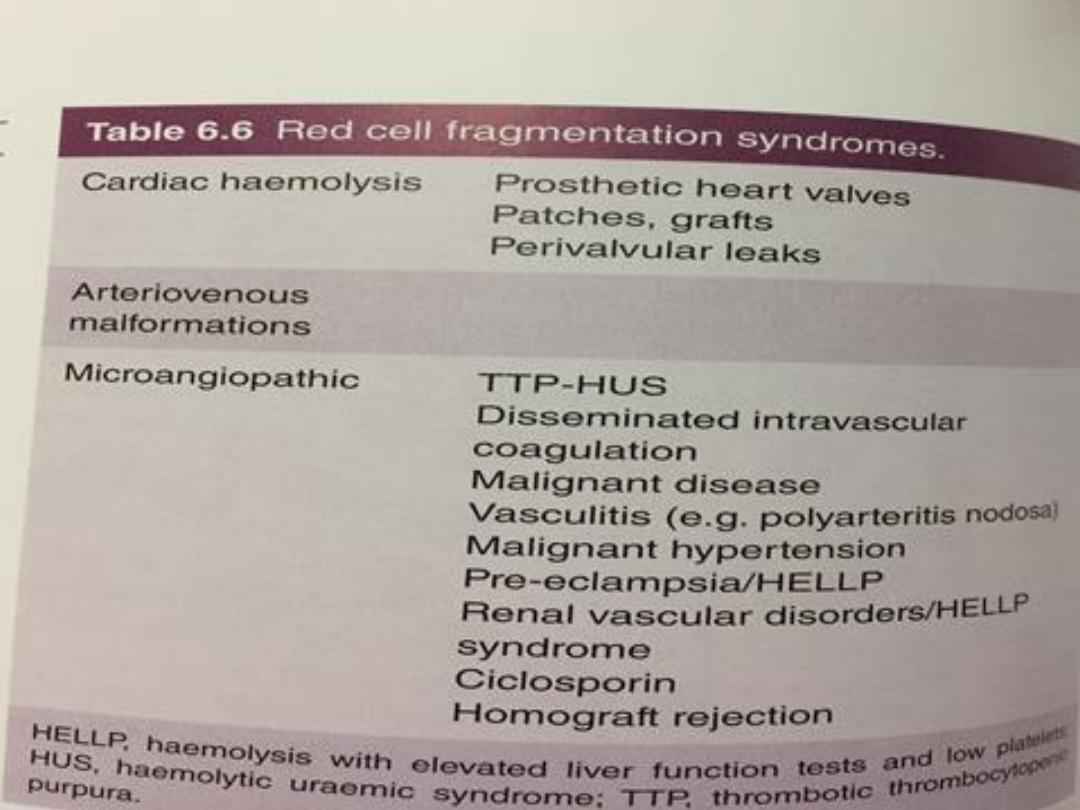
Non-immune haemolytic anaemia
• Physical trauma Physical disruption of red cells may
occur in a number of conditions and is
characterised by the presence of red cell fragments
on the blood film and markers of intravascular
haemolysis:
A. Mechanical heart valves.
B. March haemoglobinuria. Vigorous exercise, such
as prolonged marching or marathon running, can
cause red cell damage in the capillaries in the feet.
• Thermal injury. Severe burns cause thermal damage
to red cells, characterised by fragmentation and the
presence of microspherocytes in the blood.

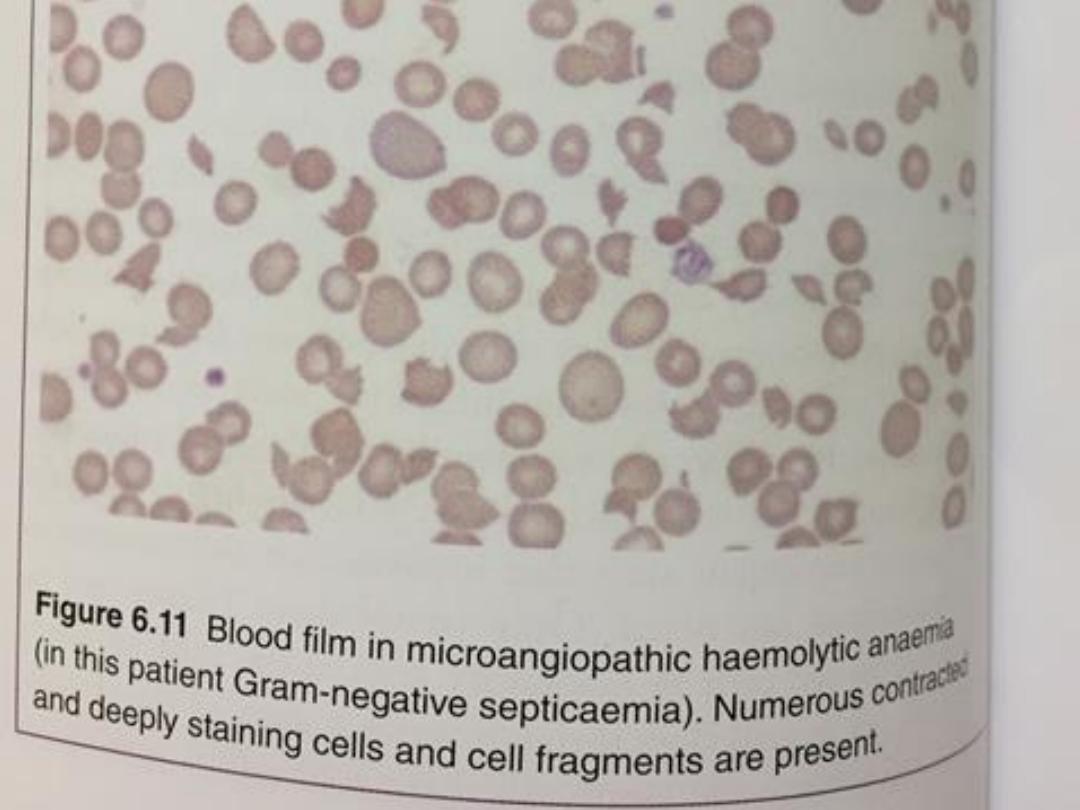
• Microangiopathic haemolytic anaemia. Fibrin
deposition in capillaries can cause severe red cell
disruption. It may occur in a wide variety of conditions:
disseminated carcinomatosis, malignant or pregnancy-
induced hypertension, haemolytic uraemic syndrome
thrombotic thrombocytopenic purpura and
disseminated intravascular coagulation
• Infection
Plasmodium falciparum malaria Clostridium perfringens
septicaemia
Chemicals or drugs
Dapsone and sulfasalazine cause haemolysis Arsenic
gas, copper, chlorates, nitrites and nitrobenzene
derivatives may all cause haemolysis.

Paroxysmal nocturnal haemoglobinuria (PNH)
• is a rare acquired, non-malignant clonal expansion of
haematopoietic stem cells deficient in GPI-anchor protein;
it results in intravascular haemolysis and anaemia because
of increased sensitivity of red cells to lysis by complement.
• Episodes of intravascular haemolysis result in
haemoglobinuria, most noticeable in early morning urine.
The disease is associated with an increased risk of venous
thrombosis in unusual sites, such as the liver or abdomen.
• PNH is also associated with hypoplastic bone marrow
failure, aplastic anaemia and myelodysplastic syndrome.
• Management is supportive with transfusion and treatment
of thrombosis.Recently, the anti-complement C5
monoclonal antibody eculizumab was shown to be effective
in reducing haemolysis
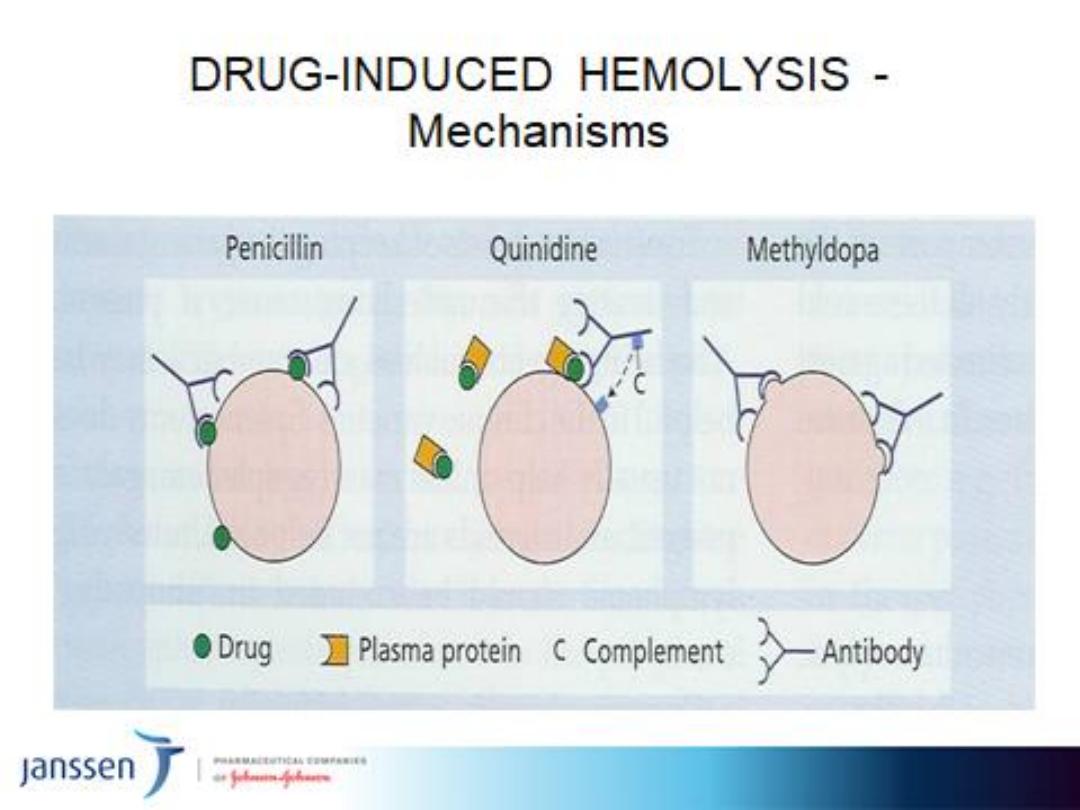
IMMUNE HEMOLYSIS (Drug-Related)
• Immune Complex Mechanism
Quinidine, Quinine, Isoniazid
• “Haptenic” Immune Mechanism
Penicillins, Cephalosporins
• True Autoimmune Mechanism
Methyldopa, L-DOPA, Procaineamide, Ibuprofen