IDA

Anemias
• Definition : Anemia is a blood disorder
characterized by abnormally low levels of healthy
red blood cells (RBCs) or reduced hemoglobin
(Hgb), the iron-bearing protein in red blood cells
that delivers oxygen to tissues throughout the body.
Reduced blood cell volume (hematocrit) is also
considered anemia.
• The reduction of any or all of the three blood
parameters reduces the oxygen-carrying capability
of the blood, causing reduced oxygenation of body
tissues, a condition called hypoxia.
• The reduction of any or all of the three blood parameters
reduces the oxygen-carrying capability of the blood,
causing reduced oxygenation of body tissues, a condition
called hypoxia.
• Description: All tissues in the human body need a regular
supply of oxygen to stay healthy and perform their
functions. RBCs contain Hgb, a protein pigment that
allows the cells to carry oxygen (oxygenate) tissues
throughout the body. RBCs live about 120 days and are
normally replaced in an orderly way by the bone marrow,
spleen, and liver.
• As RBCs break down, they release Hgb into the blood
stream, which is normally filtered out by the kidneys and
excreted. The iron released from the RBCs is returned to
the bone marrow to help create new cells.

• Anemia develops when either blood loss, a slow-down in the
production of new RBCs (erythropoiesis), or an increase in red
cell destruction (hemolysis) causes significant reductions in
RBCs, Hgb, iron levels, and the essential delivery of oxygen to
body tissues.
• Anemia can be mild, moderate, or severe enough to lead to
life-threatening complications. More than 400 different types
of anemia have been identified. Many of them are rare. Most
are caused by ongoing or sudden blood loss.
• Other causes include vitamin and mineral deficiencies,
inherited conditions, and certain diseases that affect red cell
production or destruction.
• It can also be classified based on the size of red blood
cells and amount of hemoglobin in each cell. If the cells are
small, it is microcytic anemia.
If they are large, it is macrocytic anemia
while if they are normal sized, it is normocytic anemia.

• Diagnosis in men is based on a hemoglobin of less than
130 to 140 g/L (13 to 14 g/dL), while in women, it must be
less than 120 to 130 g/L (12 to 13 g/dL). Further testing is
then required to determine the cause.
• Anemia is the most common blood disorder, affecting
about a third of the global population.
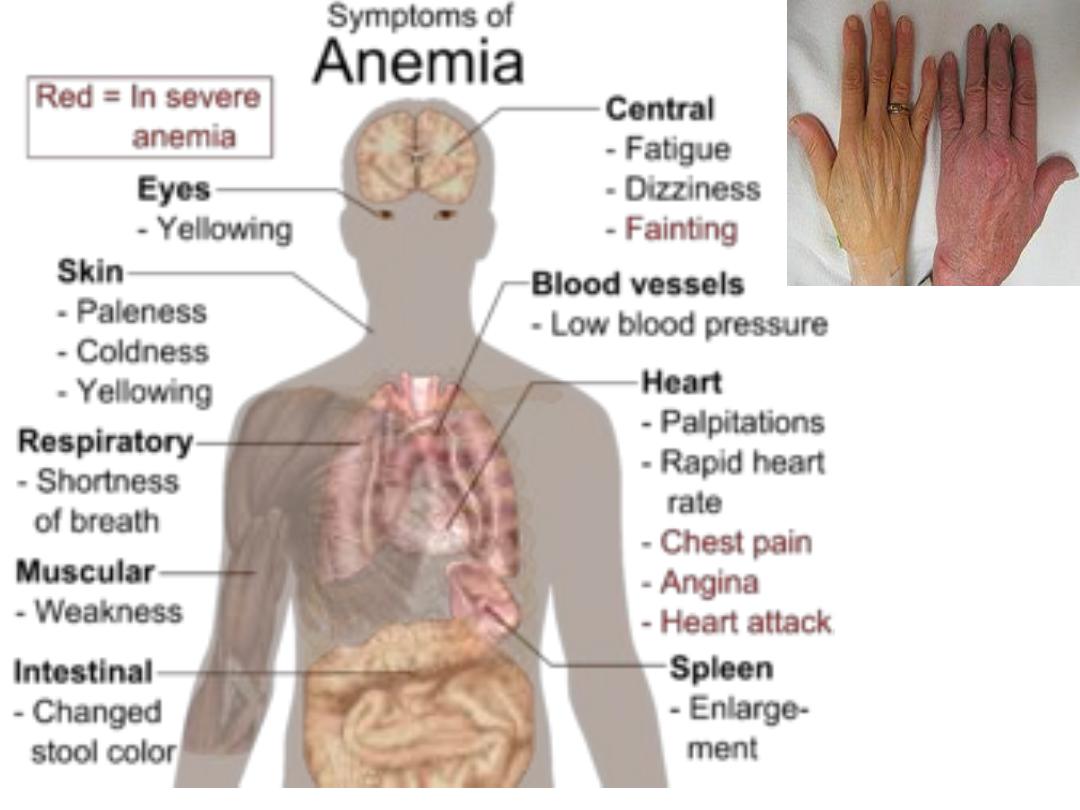
• Anemia goes undetected in many people and symptoms
can be minor. The symptoms can be related to an
underlying cause or the anemia itself. Most commonly,
people with anemia report feelings of weakness or tired,
and sometimes poor concentration.
•

• They may also report shortness of breath on exertion. In
very severe anemia, the body may compensate for the
lack of oxygen-carrying capability of the blood by
increasing cardiac output. The patient may have
symptoms related to this, such as palpitations, angina (if
pre-existing heart disease is present),
intermittent claudication of the legs, and symptoms
of heart failure
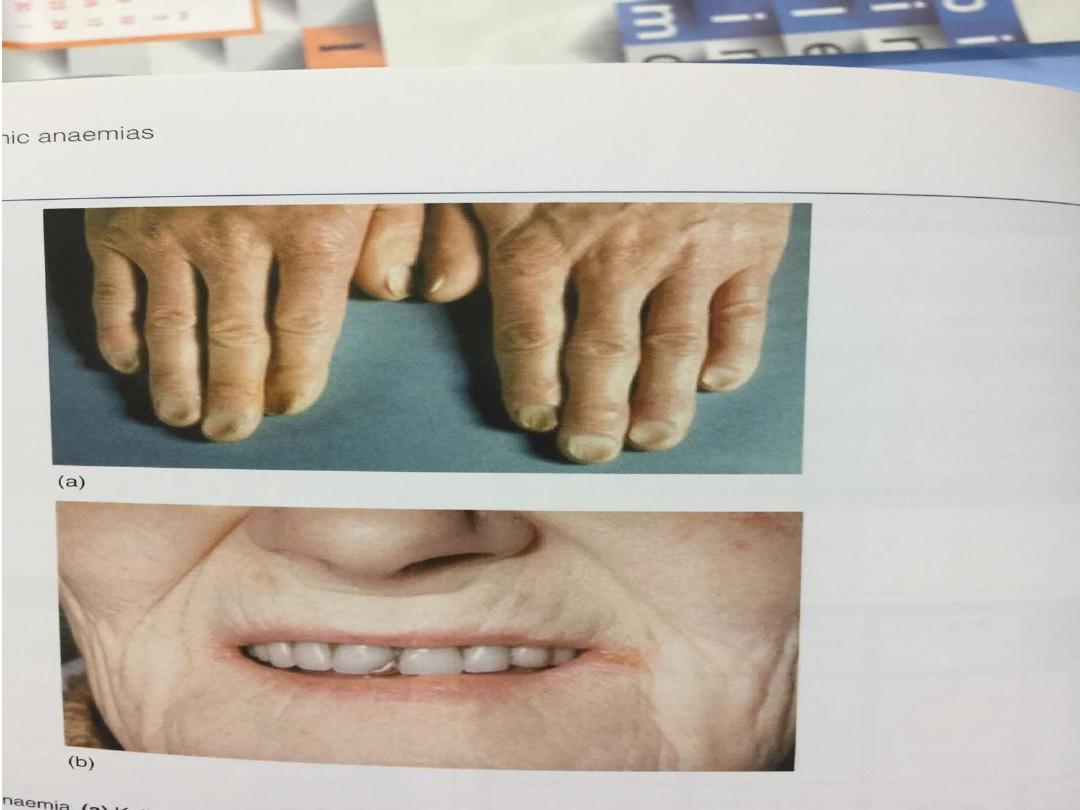
• On examination, the signs exhibited may
include pallor (pale skin,
lining mucosa, conjunctiva and nail beds), but this is not a
reliable sign. There may be signs of specific causes of
anemia, e.g., koilonychia (in iron
deficiency), jaundice (when anemia results from
abnormal break down of red blood cells — in hemolytic
anemia),
• bone deformities (foundin thalassemia major)
or leg ulcers (seen in sickle-cell disease). In severe
anemia, there may be signs of a hyperdynamic
circulation: tachycardia (a fast heart rate), bounding
pulse, flow murmurs, and cardiac ventricular
hypertrophy (enlargement). There may be signs
of heart failure. Pica, the consumption of non-food
items such as ice,
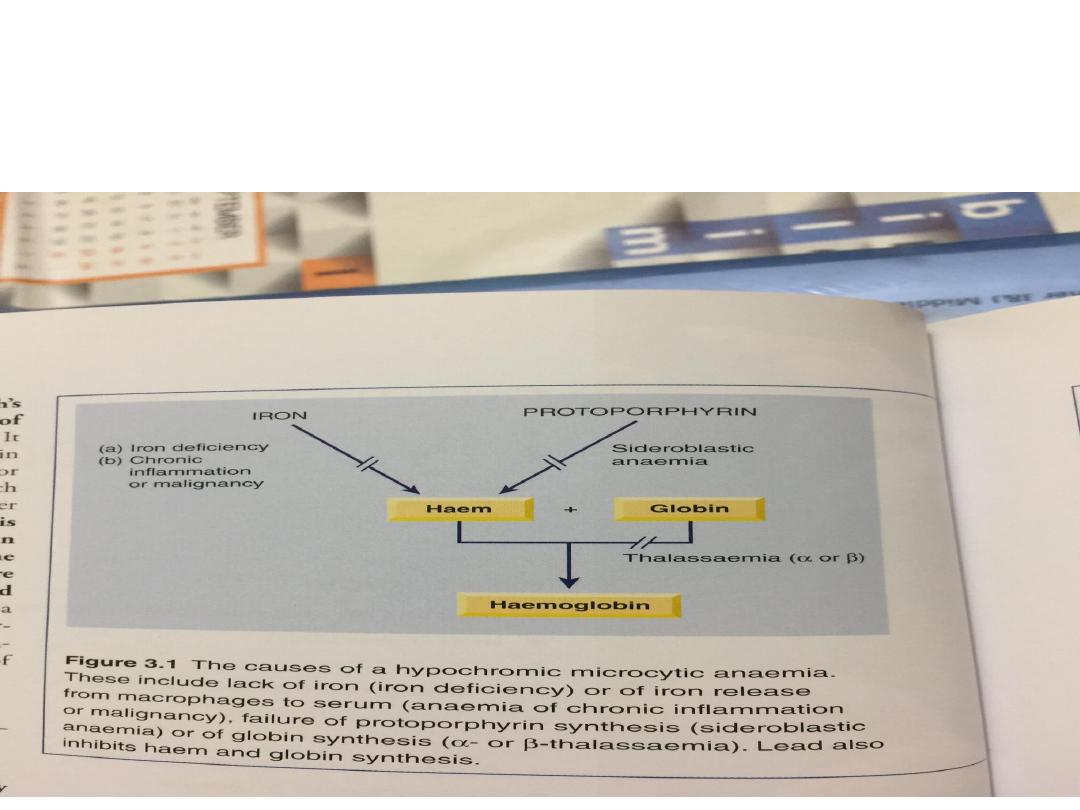
Iron deficiency anaemia
• This occurs when iron losses or physiological
requirements exceed absorption
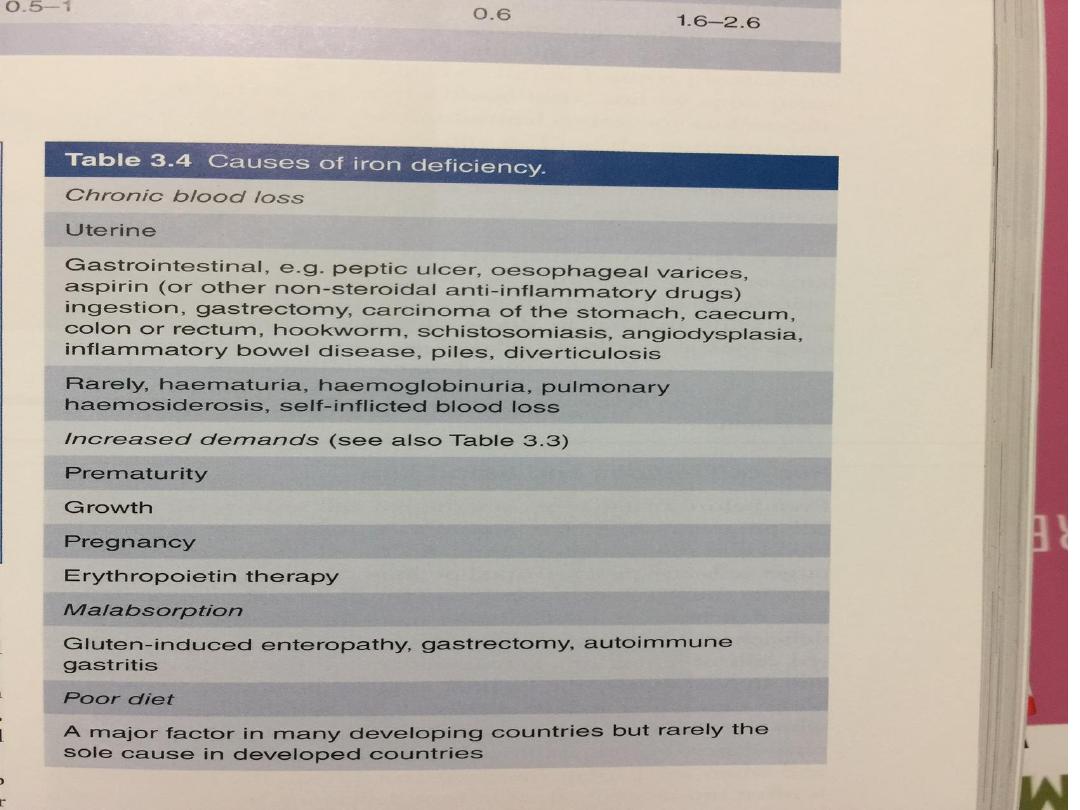
Blood loss
• The most common explanation in men and
postmenopausal women is gastrointestinal blood loss. This
may result from occult gastric or colorectal malignancy,
gastritis, peptic ulceration, inflammatory bowel disease,
diverticulitis, polyps and angiodysplastic lesions.
• Worldwide, hookworm and schistosomiasis are the most
common causes of gut blood loss In women of child-
bearing age, menstrual blood loss, pregnancy and
breastfeeding contribute to iron deficiency by depleting
iron stores; in developed countries, one-third of
premenopausal women have low iron stores but only 3%
display iron-deficient haematopoiesis. Very rarely, chronic
haemoptysis or haematuria may cause iron deficiency.

Malabsorption
• A dietary assessment should be made in all patients to
ascertain their iron intake. Gastric acid is required to
release iron from food and helps to keep iron in the soluble
ferrous state Achlorhydria in the elderly or that due to
drugs such as proton pump inhibitors may contribute to the
lack of iron availability from the diet, as may previous
gastric surgery.
• Iron is absorbed actively in the upper small intestine and
hence can be affected by coeliac disease
• Physiological demands At times of rapid growth, such as
infancy and puberty, iron requirements increase and may
outstrip absorption. In pregnancy, iron is diverted to the
fetus, the placenta and the increased maternal red cell
mass, and is lost with bleeding at parturition

Investigations Confirmation of iron deficiency :
• Plasma ferritin is a measure of iron stores in tissues and is the
best single test to confirm iron deficiency
• Plasma iron and total iron binding capacity (TIBC) are measures
of iron availability; hence they are affected by many factors
besides iron stores.
Investigation of the cause
• This will depend upon the age and sex of the patient, as well as
the history and clinical findings. In men and in post-menopausal
women with a normal diet, the upper and lower gastrointestinal
tract should be investigated by endoscopy or radiological
studies.
• Serum antiendomysial or anti-transglutaminase antibodies and
possibly a duodenal biopsy are indicated to detect coeliac
disease. In the tropics, stool and urine should be examined for
parasites
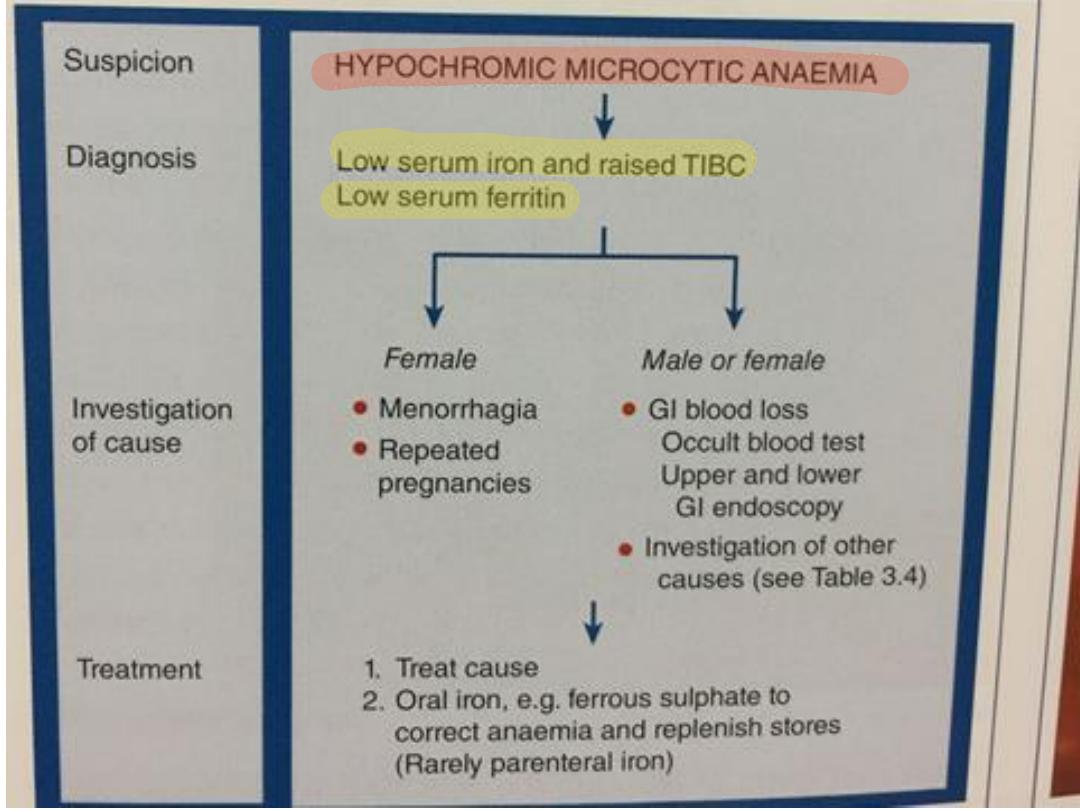

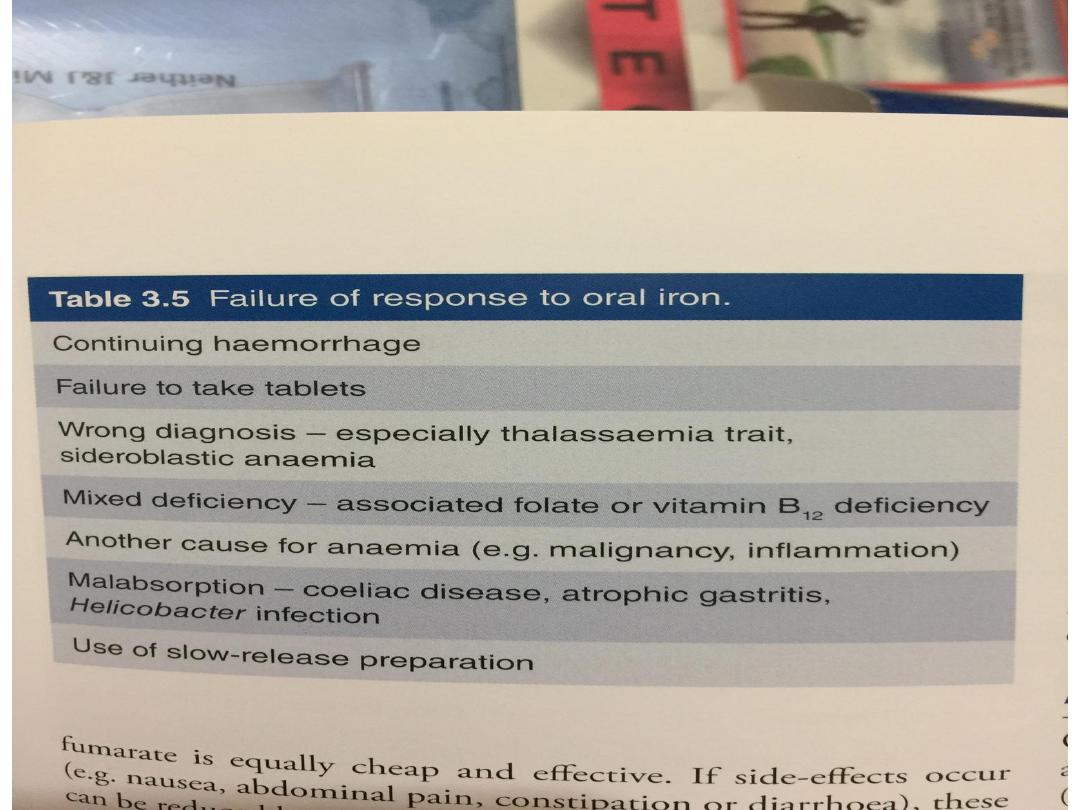
Management
• Unless the patient has angina, heart failure or
evidence of cerebral hypoxia, transfusion is not
necessary and oral iron replacement is appropriate.
• Ferrous sulphate 200 mg 3 times daily is adequate
and should be continued for 3–6 months to replete
iron stores.
• The haemoglobin should rise by around 10 g/L
every 7–10 days and a reticulocyte response will be
evident within a week. A failure to respond
adequately may be due to non-compliance,
continued blood loss, malabsorption or an incorrect
diagnosis.

• Patients with malabsorption or chronic gut disease may
need parenteral iron therapy. Previously, iron dextran
or iron sucrose was used but new preparations of iron
isomaltose and iron carboxymaltose have fewer allergic
effects and are preferred.