1
GASTROINTESTINAL TRACT
ASS. PROF.DR. MAHA SHAKIR HASSAN
Lec 4
Small and Large Intestines
DEVELOPMENTAL ANOMALIES
• Atresia or stenosis, the former being complete failure of development of
the intestinal lumen and the latter representing only narrowing.
Duplication usually takes the form of well-formed saccular to tubular
cystic structures, which may or may not communicate with the lumen of
the small intestine.
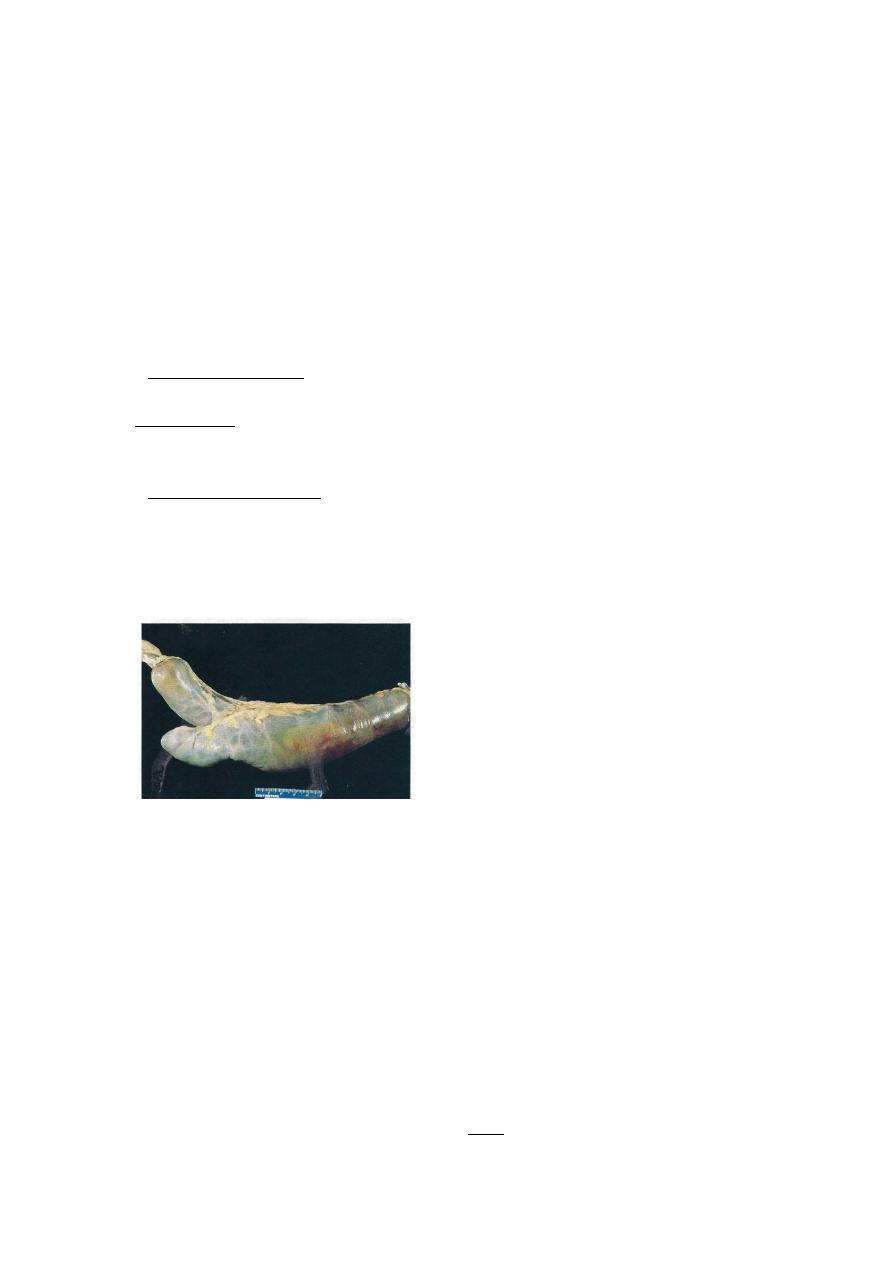
• Meckel diverticuluin is the most common and innocuous of the
anomalies. It results from failure of involution of the omphalomesenteric
duct, leaving a persistent blind-ended tubular protrusion up to 5 to 6 cm
long. The diameter is variable. Usually in the ilium, and composed of all
layers of small intestine. They are generally asymptomatic
Meckel diverticulum. The blind pouch is located on the antimesenteric side of the small bowel.
Hirschsprung Disease: Congenital Megacolon
Distention of the colon to greater than 6 or 7 cm in diameter (megacolon)
occurs as a congenital and as an acquired disorder. Hirschsprung disease
(congenital megacolon) results during development, the caudal migration
of neural crest-derived cells along the alimentary tract arrests at some
point before reaching the anus. Hence, an aganglionic segment is left that
lacks both the Meissner submucosal and Auerbach myenteric plexuses.
This causes functional obstruction and progressive distention of the colon
proximal to the affected segment. In most instances, only the rectum and
sigmoid are aganglionic, but in about a fifth of cases a longer segment,

2
and rarely the entire colon, is affected. Approximately 50% of cases
result from mutations in RET gene and RET ligands, as this signaling
pathway is required for development of the myenteric nerve plexus
MORPHOLOGY
The critical lesion is the lack of ganglion cells, and of ganglia, in the
muscle wall and submucosa of the affected segment. The affected
segment is not distended. proximal properly innervated segment that
undergoes dilation. Thus, when only the distal colon is affected, the
remainder of the colon becomes massively distended. The wall may be
thinned by distention or in some cases is thickened by compensatory
muscle hypertrophy.
Clinical Features.
In most cases a delay occurs in the initial
passage of meconium, which is followed by vomiting in 48 to 72 hours.
The principal threat to life is superimposed enterocolitis with fluid and
electrolyte disturbances. More rarely, the distended colon perforates,
usually in the thin-walled cecum. The diagnosis is established by
documenting the absence of ganglion cells in the nondistended bowel
segment.
Acquired megacolon may result from (1) Chagas disease, in which the
trypanosomes directly invade the bowel wall to destroy the plexuses, (2)
organic obstruction of the bowel by a neoplasm or inflammatory stricture,
(3) toxic megacolon complicating ulcerative colitis (discussed later), or
(4) a functional psychosomatic disorder.
VASCULAR DISORDERS
Angiodysplasia:
Tortuous dilatation of submucosal and mucosal blood vessels, most often
in the cecum or right colon. Usually only after the 6th decade.
The
pathogenesis of angiodysplasia remains undefined but has been attributed
to mechanical and congenital factors.
Degenerative vascular changes
related to aging may also have some role.
Hemorrhoids:
It is variceal dilitation of the anal and perianal submucosal venous plexus.
Pathogenesis: Persistently elevated venous pressure within hemorrhoidal
plexus.

3
Predisposing conditions:
1. Chronic constipation.
2. Pregnancy.
3. Rarely portal hypertention.
Malabsorption Syndromes and diarrhea
Malabsorption, which presents most commonly as chronic diarrhea, is
characterized by defective absorption of fats, fat- and water-soluble
vitamins, proteins, carbohydrates, electrolytes and minerals, and water.
Chronic malabsorption can be accompanied by weight loss, anorexia,
abdominal distention. A hallmark of malabsorption is steatorrhea,
characterized by excessive fecal fat and bulky, frothy, greasy, yellow or
clay-colored stools.
Most common types:
1-
Gluten-sensitive enteropathy
, also known as celiac disease,
is the prototype of a noninfectious cause of malabsorption resulting from
a reduction in small intestinal absorptive surface area. The basic disorder
in celiac disease is sensitivity to gluten, the component of wheat and
related grains (oat, barley, and rye) that contains the water-insoluble
protein gliadin. There is autoimmune mechanism responsible of
development of such disease. The small intestinal mucosa, when exposed
to gluten, accumulates large numbers of B cells and plasma cells
sensitized to gliadin; accumulation of lymphocytes in gastric and colonic
mucosa also may occur. In addition to filling the lamina propria,
lymphocytes also cross into the epithelial space, with accompanying
damage to surface enterocytes. Total flattening of mucosal villi (and
hence loss of surface area) is the outcome, affecting the proximal more
than the distal small intestine.
The age of presentation with symptomatic diarrhea and malnutrition
varies from infancy to mid adulthood; removal of gluten from the diet is
met with dramatic improvement. There is, however, a low long-term risk
of malignant disease on the order of a two-fold increase over the usual
rate. Intestinal lymphomas, especially T-cell lymphomas, are
disproportionately
represented;
other
malignancies
include
gastrointestinal and breast carcinomas.
2-Tropical sprue

4
Tropical sprue resembles celiac disease in symptomatology but occurs
almost exclusively in persons living in or visiting the tropics. No specific
causal agent has been identified, but the appearance of malabsorption
within days or a few weeks of an acute diarrheal enteric infection strongly
implicates an infectious process, also there is prompt response to broad-
spectrum antibiotic therapy. Small intestinal changes vary from near
normal to a severe diffuse enteritis with villous flattening in contrast to
celiac disease, injury is seen at all levels of the small intestine.
IDIOPATHIC INFLAMMATOR BOWEL DISEASES
Crohn Disease
This disease may affect any level of the alimentary tract, from mouth to
anus. Active cases of CD are often accompanied by extraintestinal
manifistations of immune origin, such as iritis and uveitis, sacroiliitis,
migratory polyarthritis, erythema nodosum, hepatic pericholangitis and
sclerosing cholangitis (bile duct inflammatory disorders), and obstructive
uropathy. Systemic amyloidosis is a rare late consequence. Thus, CD
must be viewed as a systemic inflammatory disease with predominant
gastrointestinal involvement.
Epidemiology.
Worldwide in distribution, CD is much more
prevalent in the United States, Great Britain and is rare in Asia and
Africa. It occurs at any age, from young childhood to advanced age, but
the peak incidence is between the second and third decades of life.
Females are affected slightly more often than males. Whites appear to
develop the disease two to five times more often than do nonwhites.
MORPHOLOGY
In CD, there is gross involvement of the small intestine alone in about
30% of Cases, of small intestine and colon in 40%, and of the colon alone
in about 30%. When fully developed, CD is characterized by (1)
sharply delimited and typically transmural involvement of the bowel
by an inflammatory process with mucosal damage, (2) the presence
of noncaseating granulomas in about 35% of cases, and (3) fissuring
with formation of fistulae.
In diseased segments hypertrophy of the muscularis propria. As a result
the lumen is almost always narrowed; in the small intestine this is
evidenced radiagraphically as the “string sign,” a thin stream of barium
passing through the diseased segment. Strictures may occur in the colon
but are usually less severe.
5
A classic feature of CD is the sharp demarcation of diseased bowel
segments from adjacent uninvolved bowel. When multiple bowel
segments are involved, the intervening bowel is essentially normal
(“skip” lesions).
In the intestinal mucosa, early disease exhibits focal mucosal ulcers
resembling canker sores (aphthous ulcers).
With progressive disease, ulcers coalesce into long, serpentine linear
ulcers, which tend to be oriented along the axis of the bowel, because the
intervening mucosa tends to be relatively spared, it acquires a coarsely
textured, cobblestone appearance.
Narrow fissures develop between the folds of the mucosa, often
penetrating deeply through the bowel wall all the way to serosa.
Further extension of fissures leads to fistula or sinus tract formation,
either to an adherent viscus, to the outside skin, or into a blind cavity to
form a localized abscess.
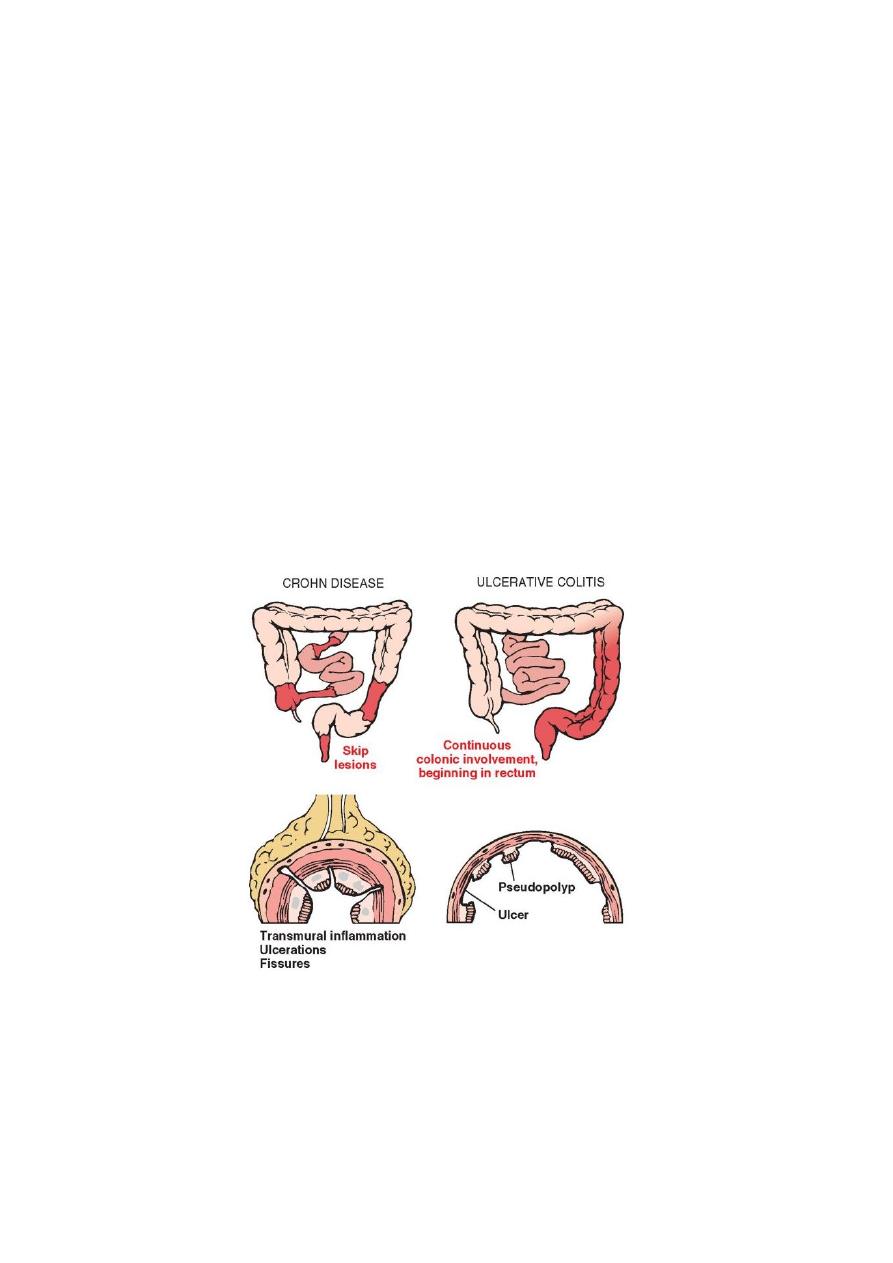
Distribution of lesions in inflammatory bowel disease. The distinction between Crohn disease and
ulcerative colitis is primarily based on morphology
.
By microscopic examination, the mucosa exhibits several
characteristic features :
6
(1) inflammation, with neutrophilic infiltration into the epithelial
layer and accumulation within crypts to form crypt abscesses;
(2) ulceration, which is the usual outcome of active disease: and
(3) chronic mucosal damage in the form of architectural
distortion, atrophy, and metaplasia.
(4) Granulomas may be present anywhere in the alimentary
tract, even in patients with CD limited to one bowel segment.
However, the absence of granulomas does not preclude a
diagnosis of CD.
(5) In diseased segments. the muscularis mucosae and
muscularis propria are usually markedly thickened, and fibrosis
affects all tissue layers.
(6) Lymphoid aggregates scattered through the various tissue
layers and in the extramural fat also are characteristic.
(7) Particularly important in patients with long-standing chronic
disease are dysplastic changes appearing in the mucosal
epithelial cells. It is related to a five-told to six-fold increased
risk of carcinoma, particularly of the colon.
7
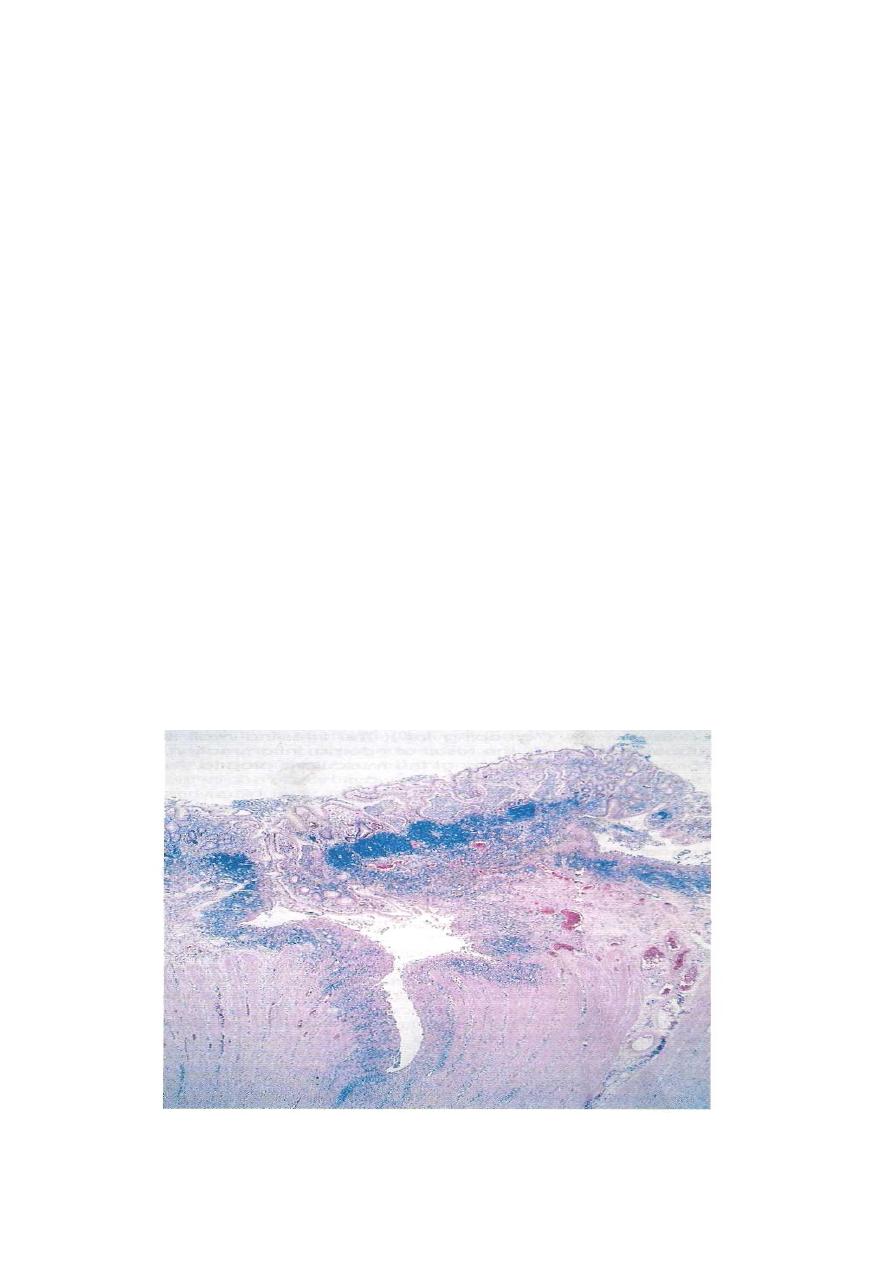
Crohn disease of the colon showing a deep fissure extending into the muscle wall, a second,
shallow ulcer (and relative preservation of the intervening mucosa). Abundant lymphocyte
aggregates are present, evident as dense blue patches of cells at the interface between mucosa and
submucosa
Clinical Features. The presentation of CD is highly variable
and ultimately unpredictable. The dominant manifestations are
recurrent episodes of diarrhea, crampy abdominal pain, and
fever lasting days to weeks.
Ulcerative Colitis
Ulcerative colitis (UC) is an ulceroinflammatory disease affecting the
colon but limited to the mucosa and submucosa except in the most severe
cases. UC begins in the rectum and extends proximally in a continuous
fashion, sometimes involving the entire colon. Like CD, UC is a systemic
disorder associated in some patients with migratory polyarthritis,
sacroiliitis, ankylosing spondylitis, uveitis, erythema nodosum, and
hepatic involvement (pericholangitis and primary sclerosing cholangitis).
There are several important differences between UC and CD:
• In UC, well-formed granulomas are absent.
• UC does not exhibit skip lesions.
• The mucosal ulcers in UC rarely extend below the submucosa, and there
is surprisingly little fibrosis.
• Mural thickening does not occur in UC, and the serosal surface is
usually completely normal.
• Patients with UC are at greater risk for carcinoma.
Epidemiology
.
UC is somewhat more common than CD in the United States and Western
countries, but it is infrequent in Asia, Africa, and South America.
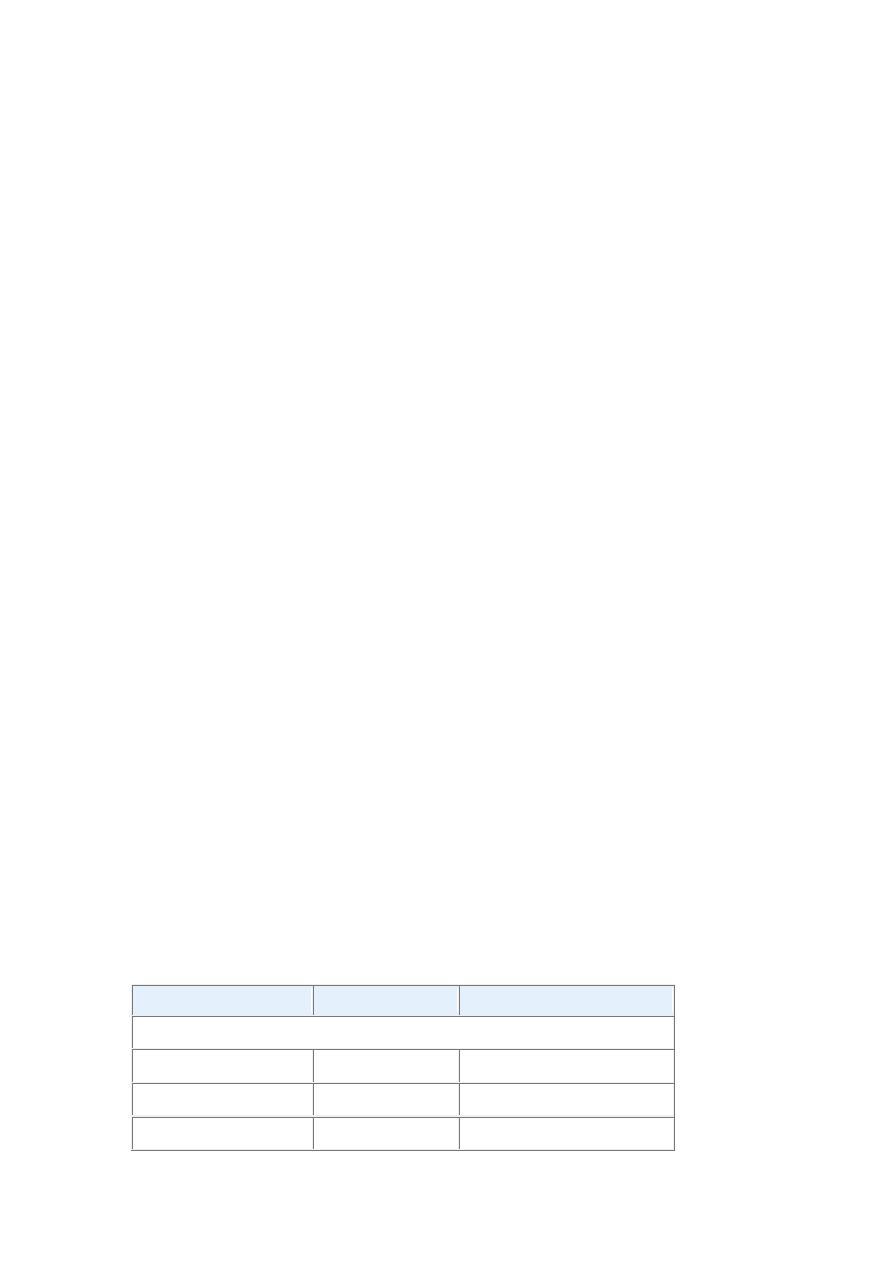
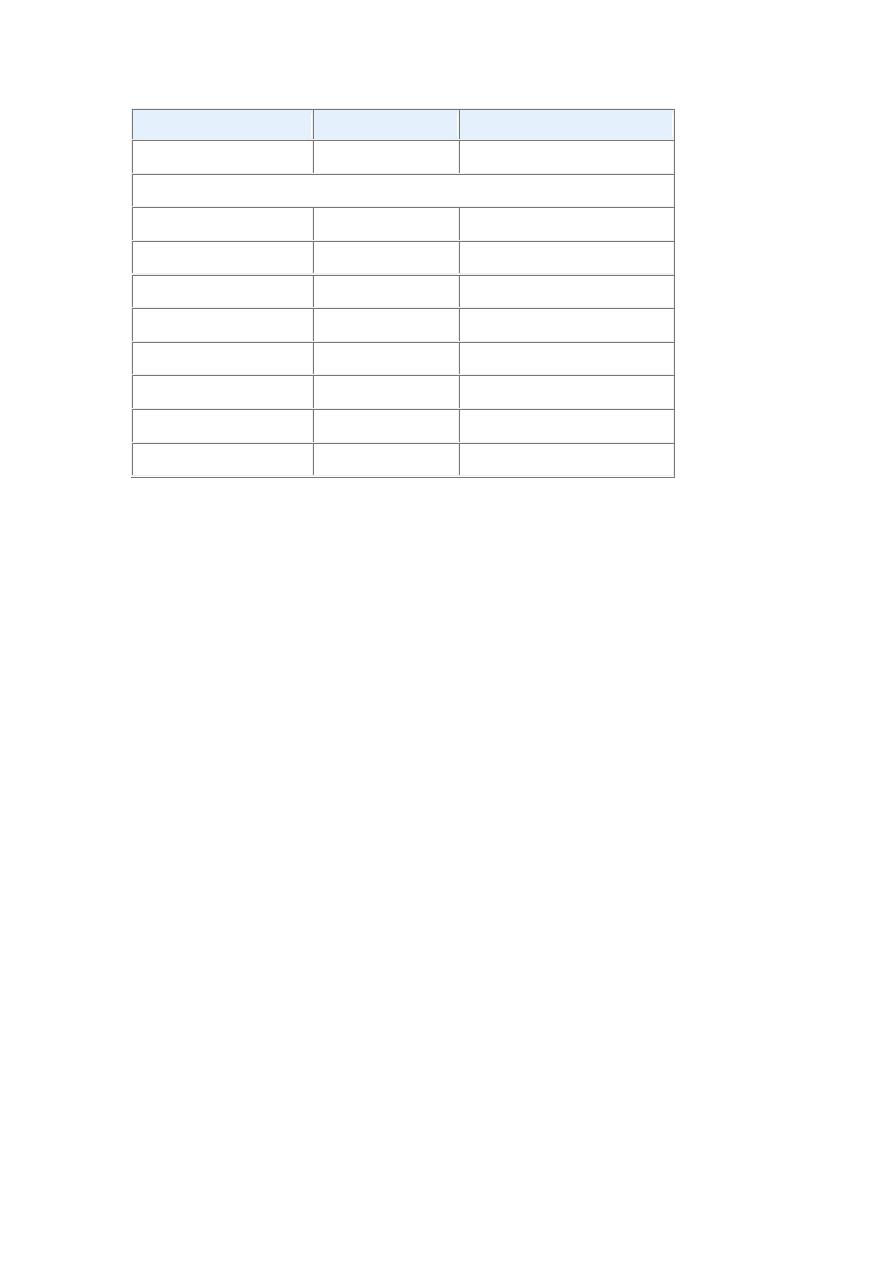
Features That Differ between Crohn Disease and Ulcerative Colitis
Feature
Crohn Disease Ulcerative Colitis
MACROSCOPIC
Bowel region
Ileum ± colon
Colon only
Distribution
Skip lesions
Diffuse
Stricture
Yes
Rare
8
Feature
Crohn Disease Ulcerative Colitis
Wall appearance
Thick
Thin
MICROSCOPIC
Inflammation
Transmural
Limited to mucosa
Pseudopolyps
Moderate
Marked
Ulcers
Deep, knife-like Superficial, broad-based
Lymphoid reaction Marked
Moderate
Fibrosis
Marked
Mild to none
Serositis
Marked
Mild to none
Granulomas
Yes (
∼35%)
No
Fistulae/sinuses
Yes
No
Morphology.
Grossly:
ulcerative colitis always involves the rectum and extends
proximally in a continuous fashion to involve part or all of the
colon.
Skip lesions are not seen .
Disease of the entire colon is termed pancolitis ,while left-sided
disease extends no farther than the transverse colon. Limited distal
disease may be referred to descriptively as ulcerative proctitis or
ulcerative proctosigmoiditis.
The small intestine is normal, although mild mucosal
inflammation of the distal ileum, backwash ileitis, may be present
in severe cases of pancolitis.
Grossly, involved colonic mucosa may be slightly red and granular
or have extensive, broad-based ulcers
Isolated islands of regenerating mucosa often bulge into the lumen
to create pseudopolyps
. Unlike Crohn disease, mural thickening is not present, the
serosal surface is normal, and strictures do not occur.
However, inflammation and inflammatory mediators can damage
the muscularis propria and disturb neuromuscular function leading
9
to colonic dilation and toxic megacolon, which carries a
significant risk of perforation.
Histologic features:
inflammatory infiltrates, crypt abscesses .
the inflammatory process is diffuse and generally limited to the
mucosa and superficial submucosa .
In severe cases, extensive mucosal destruction may be
accompanied by ulcers that extend more deeply into the
submucosa, but the muscularis propria is rarely involved.
Submucosal fibrosis, mucosal atrophy, and distorted mucosal
architecture remain as residua of healed disease but histology may
also revert to near normal after prolonged remission.
Granulomas are not present in ulcerative colitis.
The most serious complication of UC is the development of
colon carcinoma. Two factors govern the risk: duration of the
disease and its anatomic extent. It is believed that with 10 years
of disease limited to the left colon the risk is minimal, and at 20
years the risk is on the order of 2%, With pancolitis, the risk of
carcinoma is 10% at 20 years and 15% to 25% by 30 years.
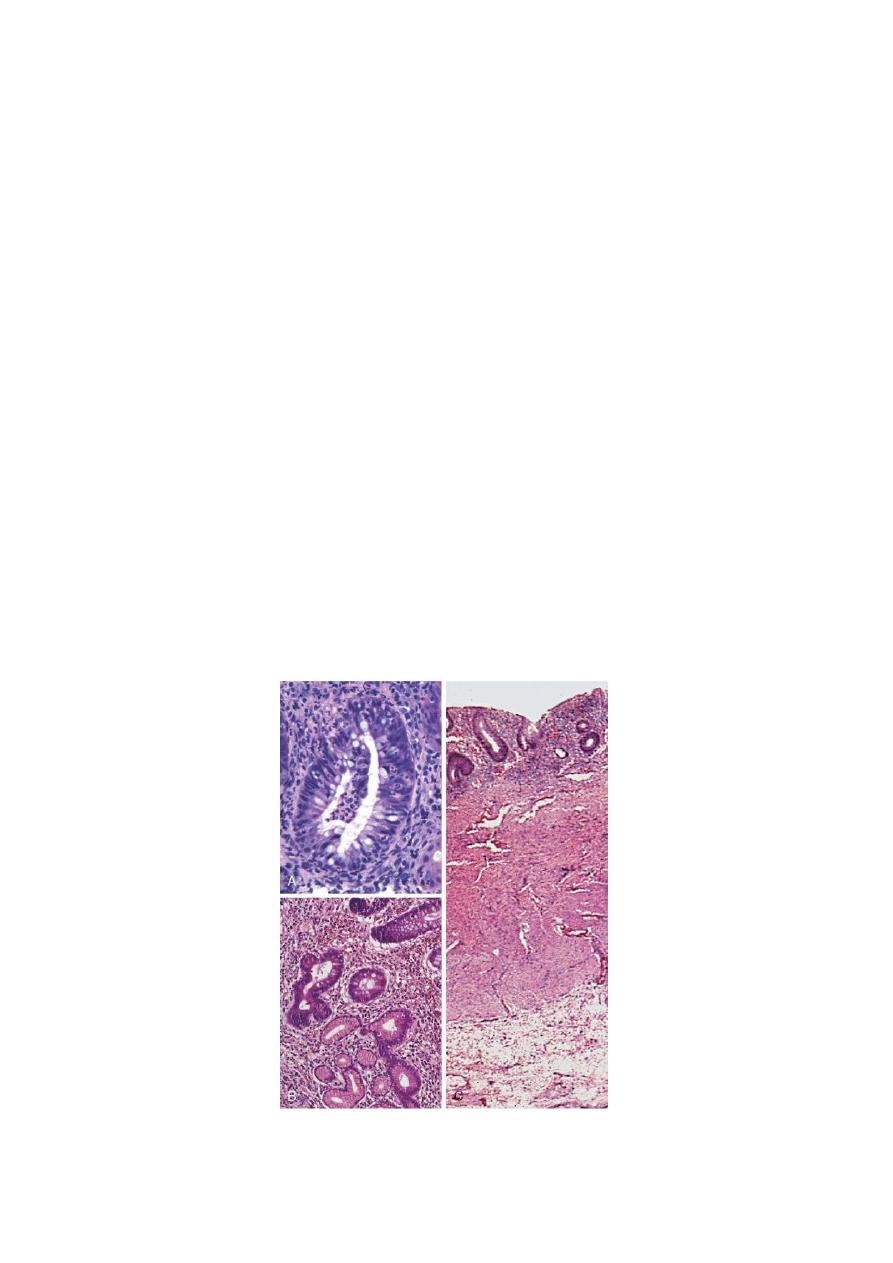
A, Crypt abscess. B, Pseudopyloric metaplasia (bottom).
C, Disease is limited to the mucosa

10
.
Clinical Features.
UC is a chronic relapsing and remitting disorder marked by
attacks of bloody mucoid diarrhea that may persist for days,
weeks, or months and then subside, only to recur after an
asymptomatic interval of months to years or even decades.
Extraintestinal
manifestations,
particularly
migratory
polyarthritis, are more common with UC than with CD.
Uncommon but life-threatening complications include:
severe diarrhea and electrolyte derangements, massive
hemorrhage, severe colonic dilation (toxic megacolon) with
potential rupture, and perforation with peritonitis. Inflammatory
strictures of the colorectum.
Diagnosis can usually be made by endoscopic examination and
biopsy. The most feared long-term complication of UC is
cancer.
