1
Dr.Maha
LEC:3
Hypertrophic Gastropathies
Hypertrophic gastropathies are uncommon diseases characterized by
giant cerebriform enlargement of the rugal folds due to epithelial
hyperplasia without inflammation. As might be expected, the
hypertrophic gastropathies are linked to excessive growth factor release.
The two most well-understood examples are Ménétrier disease and
Zollinger-Ellison syndrome
MÉNÉTRIER DISEASE
Ménétrier disease is a rare disorder caused by excessive secretion of
transforming growth factor α (TGF-α)The disease is characterized by
diffuse hyperplasia of the foveolar epithelium of the body and fundus and
hypoproteinemia due to protein-losing enteropathy.
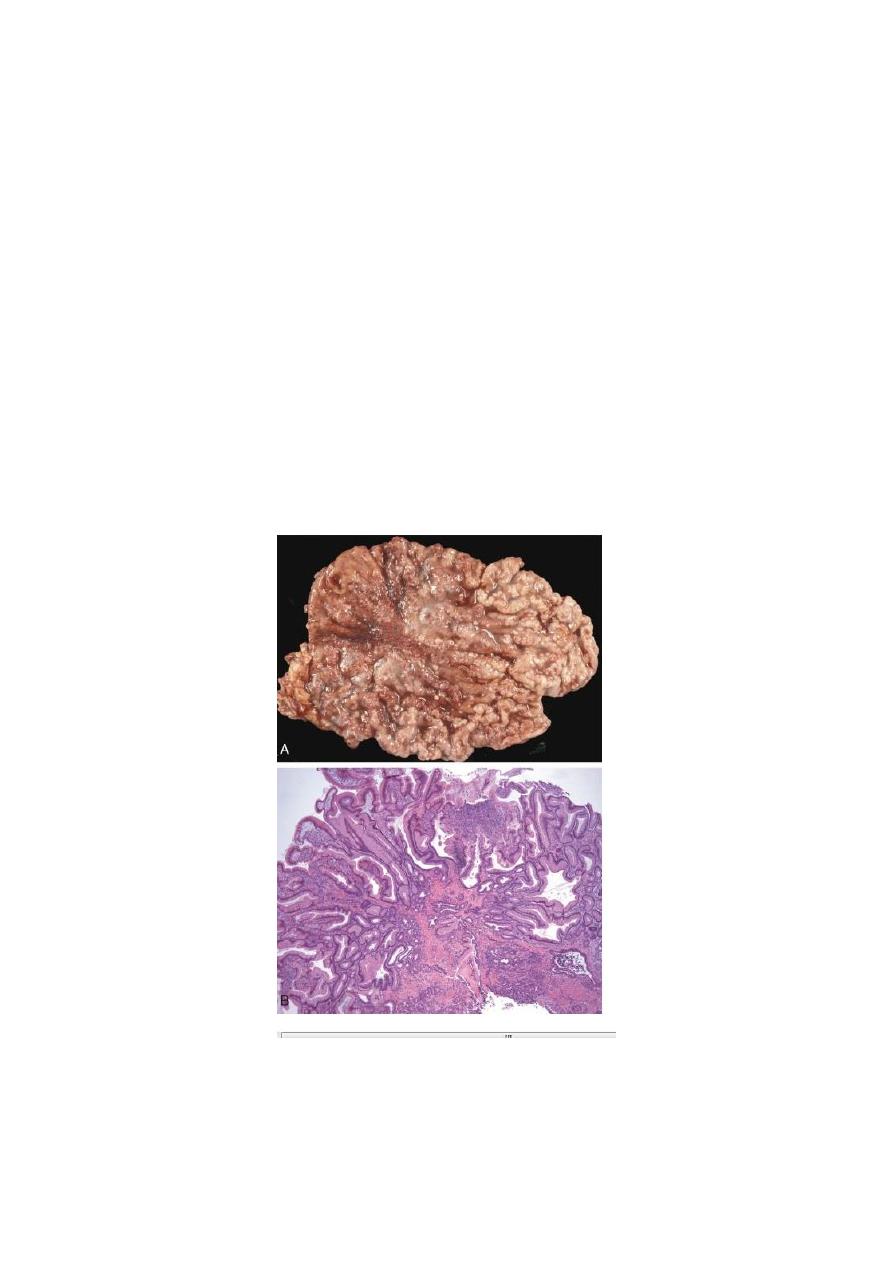
FIGURE Ménétrier disease. A, Marked enlargement of rugal folds. B, Foveolar hyperplasia with
elongated and focally dilated glands.
ZOLLINGER-ELLISON SYNDROME

2
ZOLLINGER-ELLISON SYNDROME
Zollinger-Ellison syndrome is caused by gastrin-secreting tumors,
gastrinomas, that are most commonly found in the small intestine or
pancreas. Patients often present with duodenal ulcers or chronic diarrhea.
Within the stomach, the most remarkable feature is a doubling of oxyntic
mucosal thickness due to a fivefold increase in the number of parietal
cells.
Although they grow slowly, 60% to 90% of gastrinomas are malignant.
Tumors are sporadic in 75% of patients. These tend to be solitary tumors
and can be surgically resected. The remaining 25% of patients with
gastrinomas have multiple endocrine neoplasia type I. These individuals
often have multiple tumors or metastatic disease .
Gastric Polyps and Tumors
Polyps, nodules or masses that project above the level of the surrounding
mucosa. Polyps may develop as a result of epithelial or stromal cell
hyperplasia, inflammation, or neoplasia. Most common types are:
1-INFLAMMATORY AND HYPERPLASTIC POLYPS
Approximately 75% of all gastric polyps are inflammatory or
hyperplastic polyps. They are most common in individuals between 50
and 60 years of age. These polyps usually develop in association with
chronic gastritis, which initiates the injury and reactive hyperplasia that
leads to polyp growth.. Among individuals with H. pylori gastritis, polyps
may regress after bacterial eradication. Because the risk of dysplasia
correlates with size, polyps larger than 1.5 cm should be resected and
examined histologically.
Morphology:
The majority of inflammatory or hyperplastic polyps are smaller than 1
cm in diameter and are frequently multiple, particularly in individuals
with atrophic gastritis.
Microscopically, polyps have irregular, cystically dilated, and elongated
foveolar glands .
2-GASTRIC ADENOMA
Gastric adenomas represent as many as 10% of all gastric polyps .
Patients are usually between 50 and 60 years of age, and males are
affected three times more often than females. adenomas almost always
occur on a background of chronic gastritis with atrophy and intestinal
3
metaplasia. The risk of adenocarcinoma in gastric adenomas is related to
the size of the lesion and is particularly elevated in lesions greater than 2
cm in diameter.
Overall, carcinoma may be present in up to 30% of
gastric adenomas.
Morphology. Gastric adenomas are usually solitary lesions less than 2
cm in diameter, most commonly located in the antrum. By definition, all
GI adenomas have epithelial dysplasia that can be classified as low or
high grade.
Gastric Carcinoma
Adenocarcinoma is the most common malignancy of the stomach,
comprising over 90% of all gastric cancers. Early symptoms resemble
those of chronic gastritis, including dyspepsia, dysphagia, and nausea. As
a result, these tumors are often discovered at advanced stages, when
symptoms such as weight loss, anorexia, altered bowel habits, anemia,
and hemorrhage trigger further diagnostic evaluation.
Epidemiology and Classification.
Epidemiology.
Gastric cancer incidence varies markedly with geography. In Japan,
Chile, Costa Rica are of high incidence. Mass endoscopic screening
programs can be successful in regions where the incidence is high, such
as Japan, where 35% of newly detected cases are early gastric cancer,
tumors limited to the mucosa and submucosa.
Gastric cancers exhibit two morphologic types, denoted intestinal and
diffuse. The intestinal variant is thought to arise from gastric mucous
cells that have undergone intestinal metaplasia in the setting of chronic
gastritis. This pattern of cancer tends to be better differentiated and is the
more common type in high-risk populations.
In contrast, the diffuse variant is thought to arise de novo from native
gastric mucous cells, is not associated with chronic gastritis, and tends to
be poorly differentiated.
Pathogenesis.
The major factors thought to affect the genesis
of this form of cancer are environmental, as summarized in the
following table.

4
1- Intestinal-Type Adenocarcinoma
◘Diet
Nitrites derived from nitrate.
Smoked foods and pickled vegetables
Excessive salt intake
Decreased intake of fresh vegetables and fruits:
antioxidants present in these foods may be protective
◘Chronic gastritis with intestinal metaplasia
Infection with Helicobacter pylori
Pernicious anemia
◘Altered anatomy
After subtotal distal gasrectomy
2- Diffuse carcinoma
Risk factors undefined
Morphology
Gastric adenocarcinomas are classified according to their location in the
stomach, and most importantly, according to gross and histologic
morphology.
Most gastric adenocarcinomas involve the gastric antrum; the lesser
curvature is involved more often than the greater curvature.
Gastric tumors with an intestinal morphology tend to form bulky tumors
composed of glandular structures, while cancers with a diffuse infiltrative
growth pattern are more often composed of signet-ring cells.
Although intestinal-type adenocarcinomas may penetrate the gastric
wall, they typically grow along broad cohesive fronts to form either an
exophytic mass or an ulcerated tumor. The neoplastic cells often contain
apical mucin vacuoles, and abundant mucin may be present in gland
lumens.
In contrast, diffuse gastric cancer is generally composed of discohesive
cells that do not form glands but instead have large mucin vacuoles that
5
expand the cytoplasm and push the nucleus to the periphery, creating a
signet-ring cell morphology. These cells permeate the mucosa and
stomach wall individually or in small clusters, which makes tumor cells
easy to confuse with inflammatory cells, such as macrophages, at low
magnification.
Extracellular mucin release in either type of gastric cancer can result in
formation of large mucin lakes that dissect tissue planes.
A mass may be difficult to appreciate in diffuse gastric cancer, but these
infiltrative tumors often evoke a desmoplastic reaction that stiffens the
gastric wall and may provide a valuable diagnostic clue. When there are
large areas of infitration, diffuse rugal flattening and a rigid, thickened
wall may impart a leather bottle appearance termed linitis plastica . Breast
and lung cancers that metastasize to the stomach may also create a linitis
plastica–like appearance.
all gastric carcinomas eventually penetrate the wall to involve the serosa,
spread to regional and more distant lymph nodes, and metastasize widely.
For obscure reasons, the earliest lymph node metastasis may
sometimes involve a supraclavicular lymph node (Virchow’s node).
Another somewhat unusual mode of intraperitoneal spread in females is
to both the ovaries, giving rise to the so-called Krukenberg tumor.
6
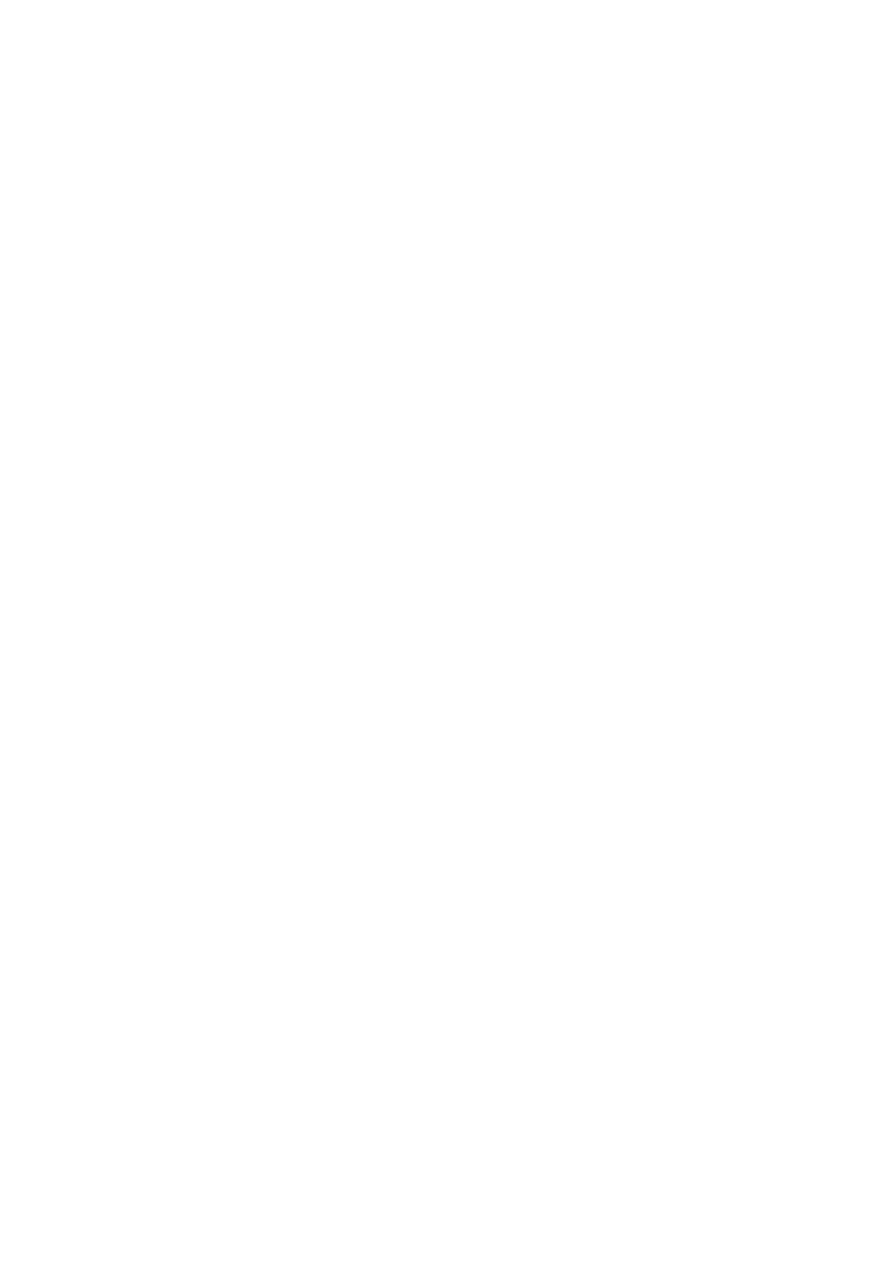
FIGURE Gastric adenocarcinoma. A, Intestinal-type adenocarcinoma consisting of an elevated mass
with heaped-up borders and central ulceration. B,Linitis plastica. The gastric wall is markedly
thickened, and rugal folds are partially lost.
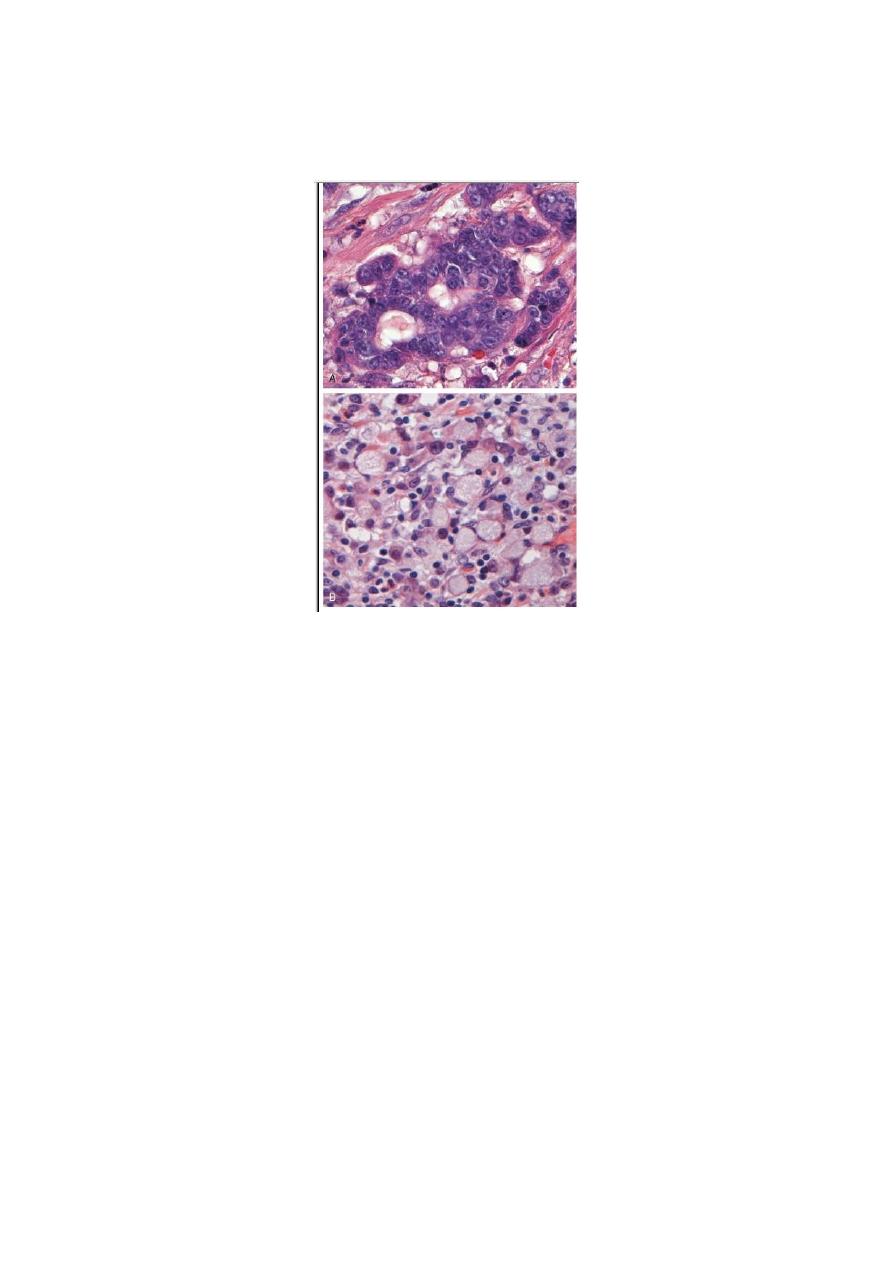
FIGURE Gastric adenocarcinoma. A, Intestinal-type adenocarcinoma composed of columnar, gland-
forming cells infiltrating through desmoplastic stroma. B, Signet-ring cells can be recognized by their
large cytoplasmic mucin vacuoles and peripherally displaced, crescent-shaped nuclei.
