
Cellular Events:
)Leukocyte Recruitment and Activation)
an important function of the inflammatory response is to deliver leukocytes to the
site of injury and to activate them. Leukocytes ingest offending agents, kill bacteria
and other microbes, and eliminate necrotic tissue and foreign substances. A price
that is paid for the defensive potency of leukocytes is that, once activated, they
may induce tissue damage and prolong inflammation, since the leukocyte products
that destroy microbes can also injure normal host tissues. Therefore, key to the
normal function of leukocytes in host defense is to ensure that they are recruited
and activated only when needed (i.e., in response to foreign invaders and dead
tissue)
Leukocyte Recruitment
The sequence of events in the recruitment of leukocytes from the vascular
lumen to the extravascular space consists of
(1) margination, adhesion to endothelium, and rolling along the vessel wall.
(2) firm adhesion to the endothelium;
(3) transmigration between endothelial cells; and
(4) migration in interstitial tissues toward a chemotactic stimulus .
Rolling, adhesion, and transmigration are mediated by the binding of
complementary adhesion molecules on leukocytes and endothelial surfaces.
Chemical mediators-chemoattractants and certain cytokines-affect these
processes by modulating the surface expression or avidity of the adhesion
molecules and by stimulating directional movement of the leukocytes .
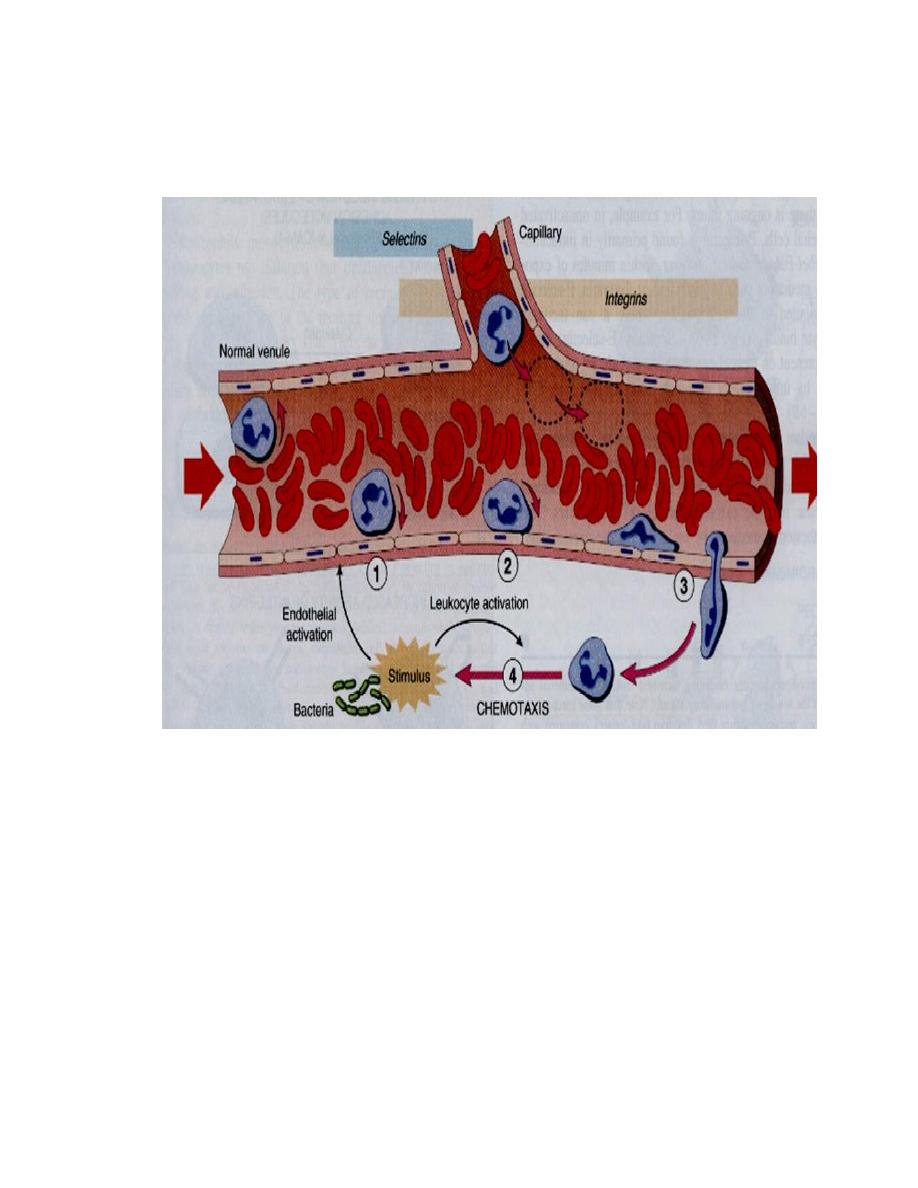
Emigration of neutrophils
Sequence of events in leukocytes emigration in inflammation:
1. Margination 2. rolling 3. adhesion 4. transmigration and movement
toward injurious agent (stimulus)
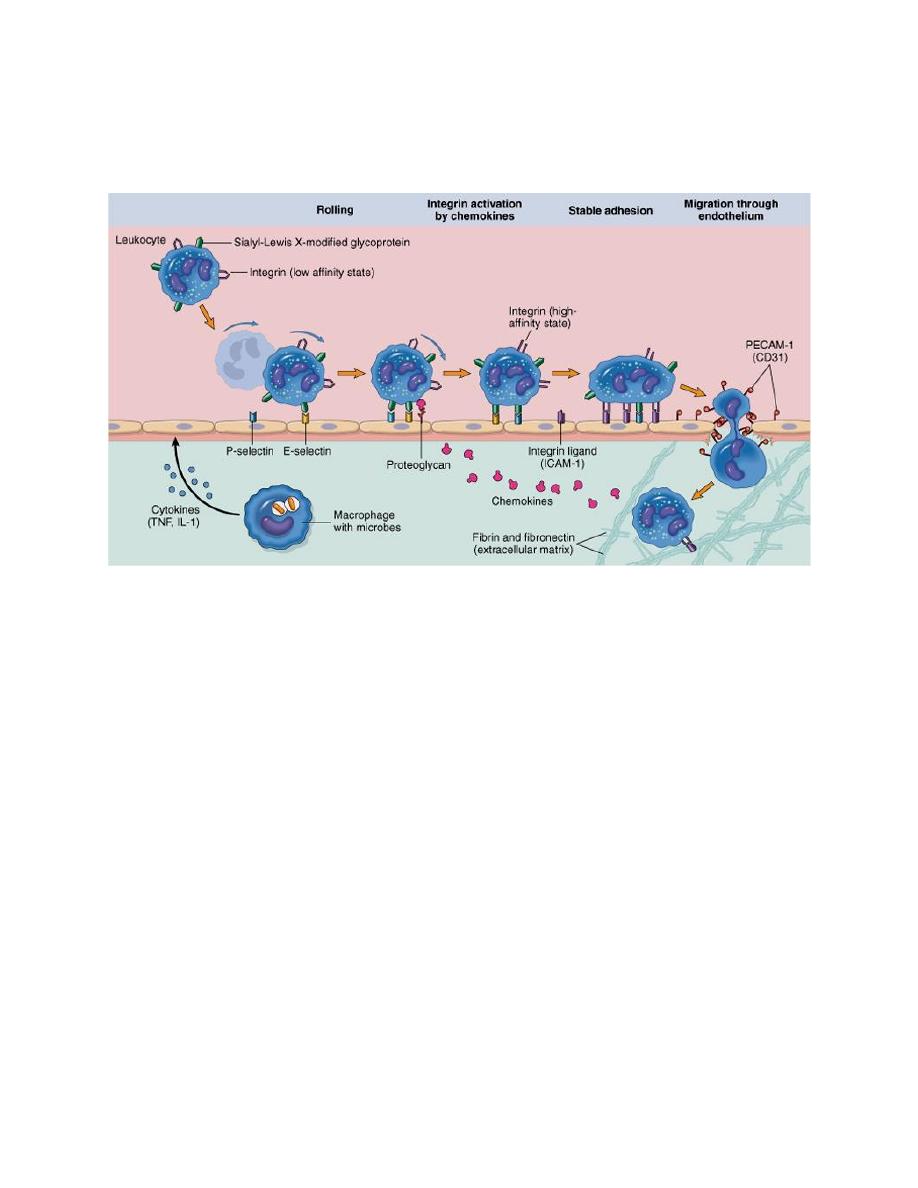
Leukocyte (neutrophil) migration through blood vessels
The leukocytes first roll, then become activated and adhere to endothelium, then
transmigrate across the endothelium, pierce the basement membrane, and migrate
toward chemoattractants emanating from the source of injury. Different molecules
play predominant roles in different steps of this process - selectins in rolling;
chemokines (usually displayed bound to proteoglycans) in activating the
neutrophils to increase avidity of integrins; integrins in firm adhesion; and CD31
(PECAM-1) in transmigration. ICAM-1, intercellular adhesion molecule 1; IL-1,
interleukin 1; PECAM-1, platelet endothelial cell adhesion molecule 1; TNF,
tumor necrosis factor.
Chemotaxis
After extravasating from the blood, leukocytes migrate toward sites of infection
or injury along a chemical gradient by a process called chemotaxis
.
Both exogenous and endogenous substances can be chemotactic for leukocytes,
including
(1)
bacterial products,

(2)
cytokines, especially those of the chemokine family;
(3)
components of the complement system, particularly C5a; and C3a
.These mediators are produced in response to infections and tissue damage and
during immunologic reactions. Leukocyte infiltration in all these situations results
from the actions of various combinations of mediators.
Leukocyte Effector Mechanisms
Leukocytes can eliminate microbes and dead cells by phagocytosis, followed by
their destruction in phagolysosomes. Destruction is caused by free radicals (ROS,
NO) generated in activated leukocytes and lysosomal enzymes. Enzymes and ROS
may be released into the extracellular environment. The mechanisms that function
to eliminate microbes and dead cells (the physiologic role of inflammation) are
also capable of damaging normal tissues (the pathologic consequences of
inflammation).

Phagocytosis
Phagocytosis of a particle (e.g., a bacterium) involves (1) attachment and binding
of the particle to receptors on the leukocyte surface, (2) engulfment and fusion of
the phagocytic vacuole with granules (lysosomes), and (3) destruction of the
ingested particle. NOS, Inducible nitric oxide synthase; NO, nitric oxide; ROS,
reactive oxygen species.
Outcome of acute inflammation
1.Resolution.
When the injury is limited or short-lived, when there has been no or minimal tissue
damage, and when the tissue is capable of replacing any irreversibly injured cells,
the usual outcome is restoration to histologic and functional normalcy.
2.Progression to chronic inflammation
may follow acute inflammation if the offending agent is not removed. In some
instances, signs of chronic inflammation may be present at the onset of injury (e.g.,
in viral infections or immune responses to self-antigens). Depending on the extent
of the initial and continuing tissue injury, as well as the capacity of the affected
tissues to regrow, chronic inflammation may be followed by restoration of normal
structure and function or may lead to scarring.
3. Scarring or fibrosis
results after substantial tissue destruction or when inflammation occurs in tissues
that do not regenerate. In addition, extensive fibrinous exudates (due to increased
vascular permeability) may not be completely absorbed and are organized by
ingrowth of connective tissue, with resultant fibrosis.
4. Abscesses
may form in the setting of extensive neutrophilic infiltrates or in certain bacterial
or fungal infections (these organisms are then said to be pyogenic, or "pus
forming"). Because of the underlying tissue destruction (including damage to the
ECM), the usual outcome of abscess formation is scarring.
