Lec.8
Class : Sporozoa (Coccidia)
Intestinal sporozoa
Cryptosporidium parvum :
Cryptosporidia were first observed in the gastric mucosal crypts of laboratory mice by
Tyzzer in 1907. Its importance as a pathogen causing diarrhoea in animals was recognised in
1971 and the first case of human infection reported in 1976. Cryptosporidium has assumed great
importance as a frequent cause of intractable diarrhoea in AIDS patients. It can lead to acute self-
limited diarrhoea in previously healthy persons and chronic life-threatening diarrhoea in
immunocompromised subjects.
Morphology :
The parasite shows six distinct morphological forms during its life cycle: oocyst, sporozoite,
trophozoite, meront, microgamont, and macrogamont.
1- Oocyst : Cryptosporidium oocyst is the smallest coccidian known to cause infection in man. It
is colourless, spherical to oval and measures 4.5 to 6 µm in diameter. It does not stain with iodine
and is acid-fast. The cyst is surrounded by thin cyst wall. Each oocyst contains up to four slender
bow-shaped sporozoites and many small granules. The oocysts are excreted in small numbers in
the faeces. The number of oocysts excreted bears no relationship with the severity of illness. The
oocysts which sporulate inside the host are of two types: Thick-walled and Thin-walled. The
thick-walled sporulating oocysts are infectious to susceptible human hosts, whereas thin-walled
oocysts always cause autoinfection in the same host only.
!1
Coll. Medicine \3
rd
stage
Parasitology
.Dr. Amal KH. KH
2- Sporozoite : The sporozoite is slender, crescent-shaped and measures 1.5 to 1.75 µm in
diameter. The anterior end is pointed but the posterior end that contains a prominent nucleus is
rounded. The sporozoites numbering four remain always parallel to each other within an oocyst ,
with apical complex and are released only after partial digestion of the oocyst.
3-Trophozoite : It is the intracellular transitional form of the parasite. It is round or oval and
measures 2 to 2.5 µ m in diameter. Each trophozoite consists of a large nucleus (1 to 1.3µm in
diameter) with or without a conspicuous nucleolus .Unlike in the sporozoites and merozoites, the
apical complex is not present in the trophozoite.
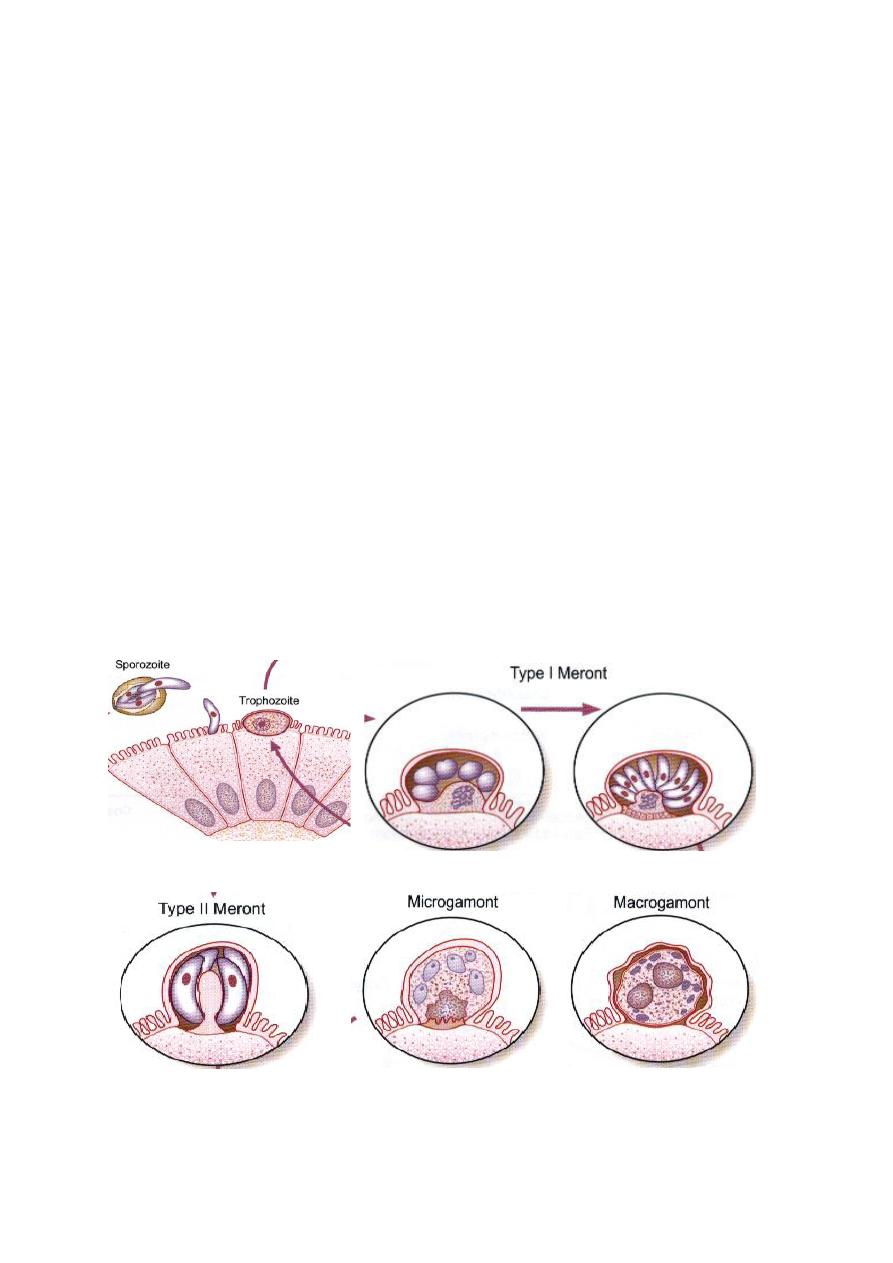
4- Meront : It is of two types: type I and type Il meronts. These two forms morphologically are
indistinguishable form each other. They are crescent-shaped and measure 1 to 5µm in diameter
showing rounded anterior and posterior ends .
5- Microgamont :Microgamonts are the male sexual forms. These are wedge-shaped, 0.2 to 0.7
µm in length and are covered by a double layered membrane. Each microgamont contains a large
compact nucleus and a polar ring. A single microgamont gives 1 to 4 microgametocytes.
6- Macrogamont : Macrogamonts are the female sexual forms. These are spherical, measure 3 to
5 µm and are covered by a double layer membrane. Each macrogamont consists of a single large
nucleus and endoplasmic reticulum. The old macrogamonts characteristically contain dense
polysaccharide granules.
!2

Life cycle :
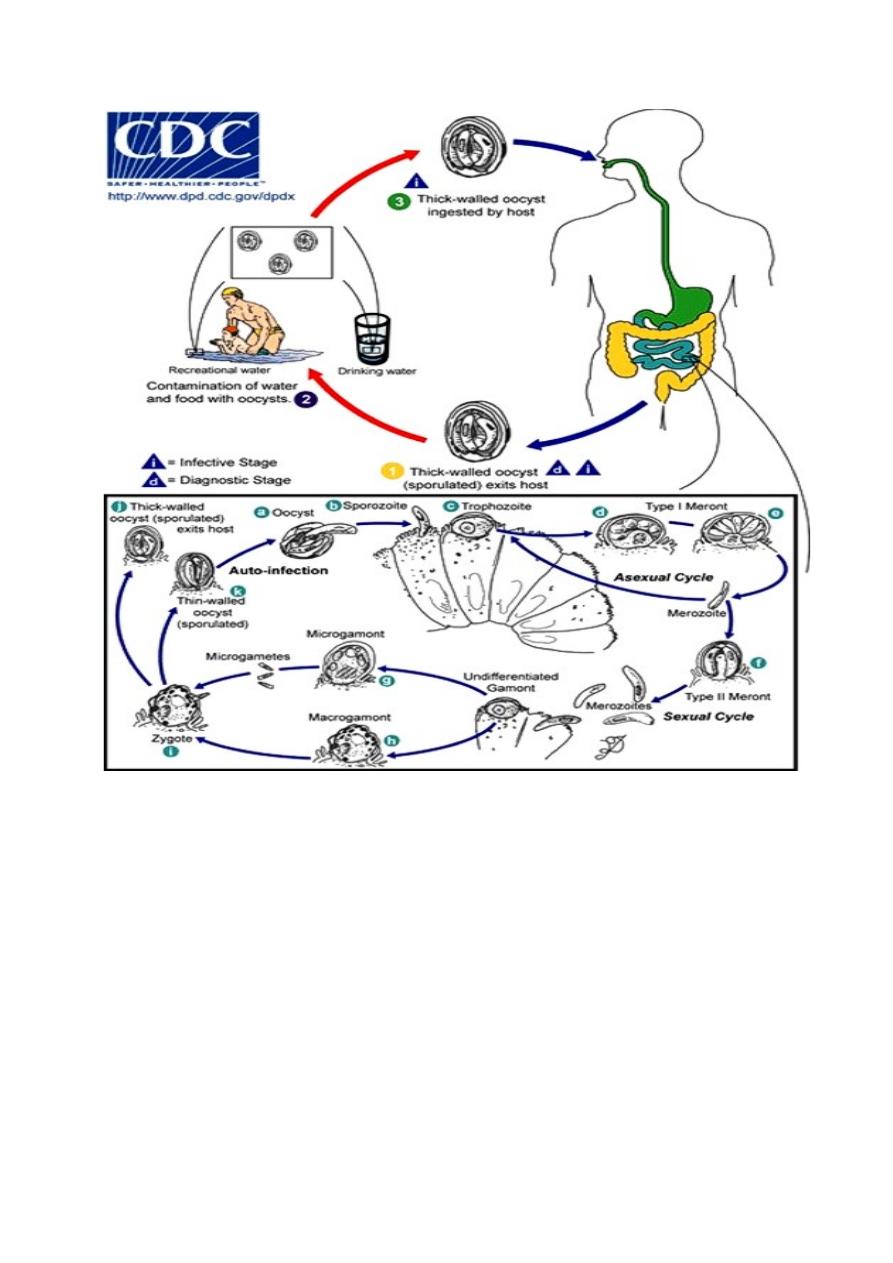
C. parvum has a simple life cycle . the infective form of the parasite is oocyst . Humans are
infected by peroral ingestion of infective oocysts. Cryptosporidium completes its life cycle
through the stages of asexual generation (schizogony) and sexual generation (gametogony) in a
single host .All these stages of the parasite are truly intracellular and are being surrounded by a
host cell membrane, which is extra-cytoplasmic. Man acquires infection on ingestion of food or
drink contaminated with the faeces, containing sporulated thick-walled oocysts of
C'ryptosporidium. On ingestion, the infective sporozoites after being released from the oocysts in
the small intestine, invade the epithelial cells in which they parasitise. Inside the epithelial cells,
the sporozoites subsequently differentiate into intracellular trophozoites. These trophozoites
multiply asexually by nuclear division to produce two types of meronts, type I and type II . Each
type I meront produces six to eight type I merozoites, which develop into type II meronts. These
in turn produce four merozoites each, which are known as type II merozoites. Some of the type II
merozoites invade new host ceils and initiate sexual replication (gametogony). Inside the host
cells, they differentiate either into female (macrogamont) or male (microgametocyte) forms. Each
microgametocyte produces 16 sperm-like microgametes, which fertilize the macrogamonts
resulting in the formation of oocysts (zygote). Four sporozoites are formed inside each oocyst in
situ. The sporulating oocysts are of two types, thin or thick-walled. The thin-walled oocysts
release the sporozoites inside the lumen of the intestine and cause auto- infection in the same host
by repeating the cycle of schizogony and gametogony. The thick-walled oocysts excreted in the
faeces are infective to other human hosts. The cysts under favourable conditions remain viable
and infectious relatively for a long time. These cysts, when taken up by other susceptible human
hosts, cause infection and the cycle are repeated.
!3
Pathology and clinical features :
Infection begins with the firm attachment of Cryptosporidium to the mucosal surface of the
intestine followed by invasion of epithelial cells. The specific mechanism by which the parasite
causes illness in man is not known but cause cholera-like voluminous watery diarrhea, Reduction
in the mucosal surface and decrease in the mucosal enzymes frequently seen in this condition also
may contribute to pathophysiology of osmotic diarrhea by lowering the absorbing capacity of the
small intestine.
Bacterial fermentation of sugars and fatty acids of the unabsorbed nutrients present in the lumen
of the intestine, cause offensive and foul smelling stool, characteristically seen in
Cryptosporidium diarrhea. Cryptosporidium is found attached to tile brush border of the small
intestine particularly the jejunum . In the immunocompromised hosts, the parasites are also found
in the uncommon sites such as pharynx, oesophagus, stomach, gall bladder, ileum, colon or
!4

rectum. Incubation period ranges from 2 to 14 days. The prepatent period (time between infection
and oocysts shedding) ranges from 5 to 21 days in man. The patent period (duration of oocysts
shedding) may last for more than 30 days in an immunocompetent host. The clinical
manifestations of Cryptosporidium infection vary depending upon the immune status of the host
and the symptoms that accompany diarrhea are abdominal cramps , weight loss , flatulence and
malaise.
Diagnosis :
In C . parvum diarrhea feces show oocysts . The oocysts are difficult to visualize in unstained
wet preparation . So used Modified Ziehl-Neelson stain readily identifies C. parvum oocysts. The
four sporozoites present in oocysts are difficult to visualize by the above mentioned methods .So
staining with other stains to visualize them .
❑ Concentration techniques are useful when C. parvum oocysts are not seen even examining
three fecal smears .
❑ Intestinal biopsy and enterotest are useful to demonstration the oocysts .
Treatment :
The only drug with efficacy against Cryptosporidium is Nitazoxanide. management of patients
include supportive care with fluids and electrolyte replacement is require .
Prevention and control :
➢ Hygienic precautions when handling oocysts excreters (humans, animals) and diagnostic
specimens.
➢ Improvement of community drinking water processing in some areas. The oocysts are
resistant to the standard concentrations of chlorine or ozone in drinking water, but can be
killed by heat (>70 Cᵒ) in a few minutes.
!5
