Ultrasound in the assessment of fetalwell-being
Dr.SumeyaAmniotic fluid volume
The amount of amniotic fluid in the uterus is a guide to fetal well-being in the third trimester..A reduction in amniotic fluid volume is referred
to as ‘oligohydramnios’ and an excess is referred to
as ‘polyhydramnios’.
Definitions of oligohydramnios and polyhydramnios are based on sonographic criteria.
Two ultrasound measurement approaches give an indication of amniotic fluid volume. These are maximum vertical pool and amniotic fluid index.
The maximum vertical pool is measured after a general survey of the uterine contents.
Measurements of less than 2 cm suggest oligohydramnios, and measurements of greater than 8 cm suggest polyhydramnios.The Amniotic Fluid Index (AFI) is measured by dividing the uterus into four ‘ultrasound’ quadrants.
A vertical measurement is taken of the deepest cord free pool in each quadrant and the results summated.
The AFI alters throughout gestation, but in the third trimester it should be between 10 and 25 cm;
values below 10 cm indicate a reduced volume and those below 5 cm indicate oligohydramnios,
while values above 25 cm indicate polyhydramnios.
Amniotic fluid volume is decreased in
fetal growth restriction as a consequence of redistribution of fetal blood away from the kidneys to vital structures such as the brain and heart with a consequent reduction in renal perfusion and urine output.
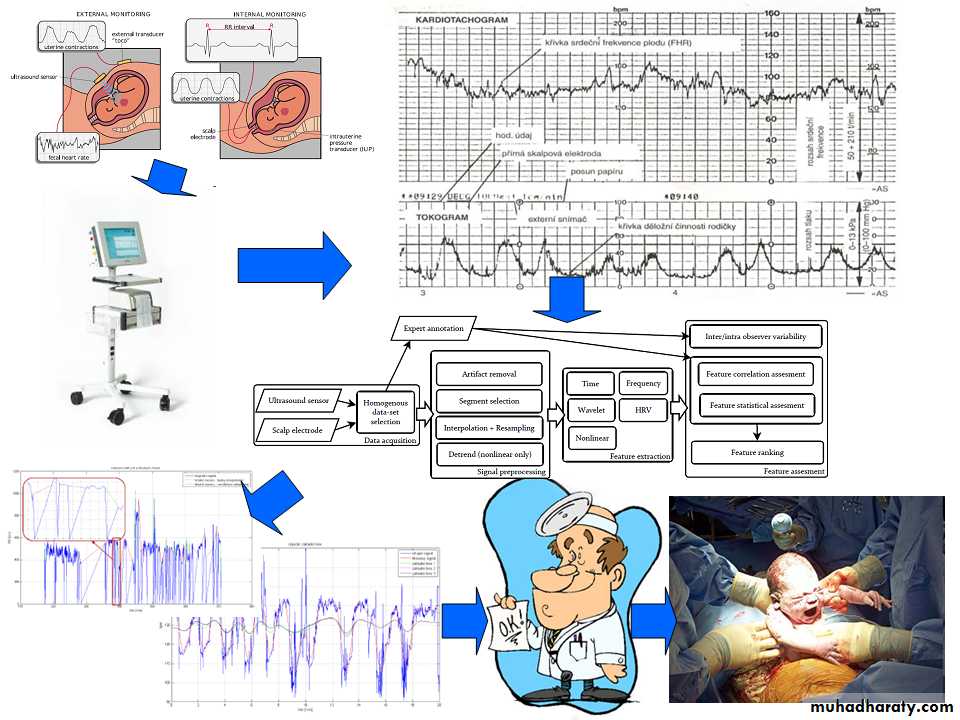
The cardiotocograph
The cardiotocograph (CTG) is a continuous tracing of the fetal heart rate used to assess fetal wellbeing.
The Doppler effect detects fetal heart motion and allows the interval between successive beats to be measured, there by allowing a continuous assessment of fetal heart rate.
Fetal cardiac behavior is regulated through the autonomic nervous system and by vasomotor, chemoceptor and baroreceptor mechanisms.
Pathological events, such as fetal hypoxia, modify these signals and hence cardiac response including variation in heart rate patterns, which can be detected and recorded in the CTG.
Features which are reported from a CTG to define normality and identify abnormality and potential concern for fetal well-being include the:
baseline rate
• baseline variability• accelerations
• decelerations
Interpretation of the CTG must be in the context of any risk factors, for example suspected FGR
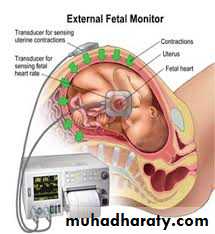
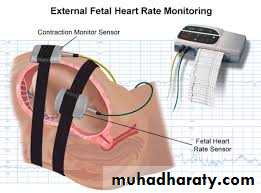
The recording is obtained with the pregnant woman positioned comfortably in a left lateral or semi-recumbent position to avoid compression of the maternal vena cava.
An external ultrasound transducer for monitoring the fetal heart and a tocodynometer (stretch gauge) for recording uterine
activity are secured overlying the uterus.
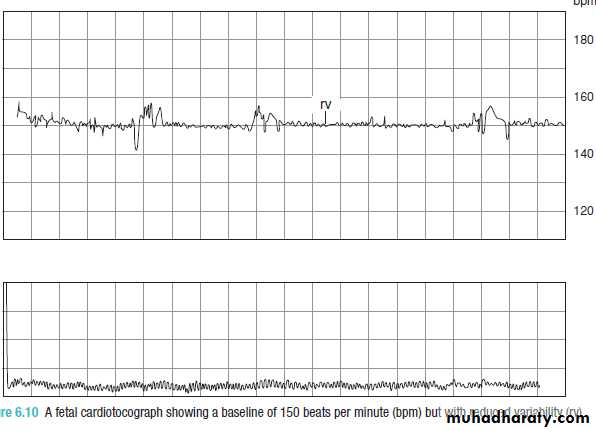
Recordings are then made for at least 30 minutes with the output from the CTG machine producing two ‘lines’, one a
tracing of fetal heart rate and a second a tracing of uterine activity.
Baseline fetal heart rate
The normal fetal heart rate at term is 110–150 bpm.Higher rates are defined as fetal tachycardia and
lower rates fetal bradycardia.The baseline fetal heart rate falls with advancing gestational age as a result of maturing fetal parasympathetic tone and prior to term 160 bpm is taken as the upper limit of normal.
The baseline rate is best determined over a period of 5–10 minutes.
Fetal tachycardias can be associated
with maternal or fetal infection,acute fetal hypoxia,
fetal anaemia and
drugs such as adrenoceptor agonists, for example ritodrine.
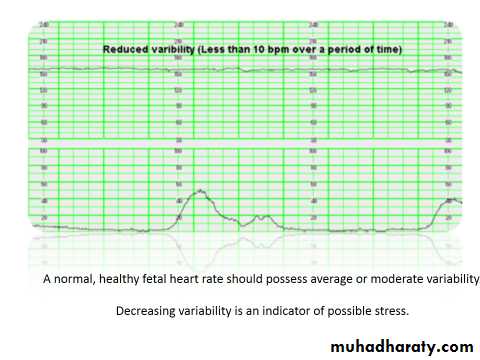
Baseline variability
Under normal physiological conditions, the interval between successive heart beats (beat-to-beat) varies.This is called ‘short-term variability’ and increases with increasing gestational age.
It is not visible on a standard CTG but can be measured with
computer-assisted analysis.
In addition to these beat-to- beat variations in heart rate, there are longer-term fluctuations in heart rate occurring between two
and six times per minute.
This is known as ‘baseline variability’.
Normal baseline variability reflects a normal fetal autonomic nervous system.
Baseline variability is considered abnormal when it is less than 10 beats per minute (bpm).As well as gestational age, baseline variability is
modified by1- fetal sleep states and activity
2-hypoxia,
3-fetal infection
4-drugs suppressing the fetal central nervous system, such as opioids, and hypnotics (all of which reduce baseline
variability).
As fetuses display deep sleep cycles of
20–30 minutes at a time, baseline variability may benormally reduced for this length of time, but should
be preceded and followed by a period of trace with
normal baseline variability.
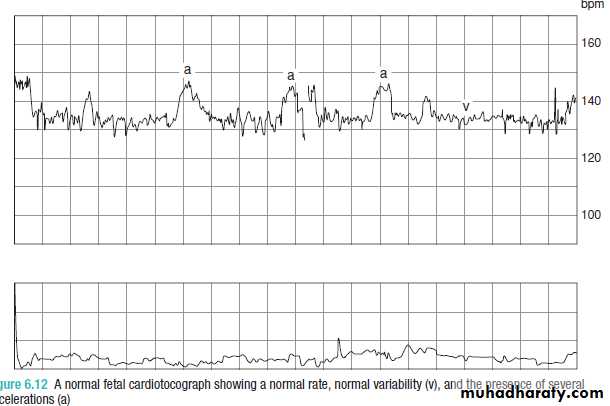
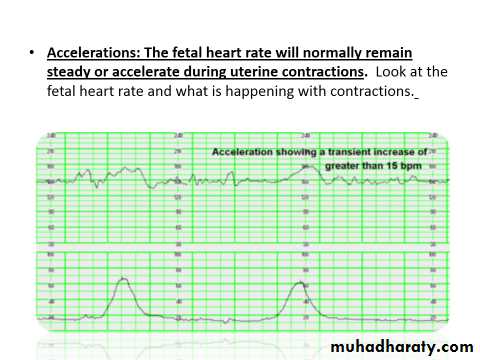
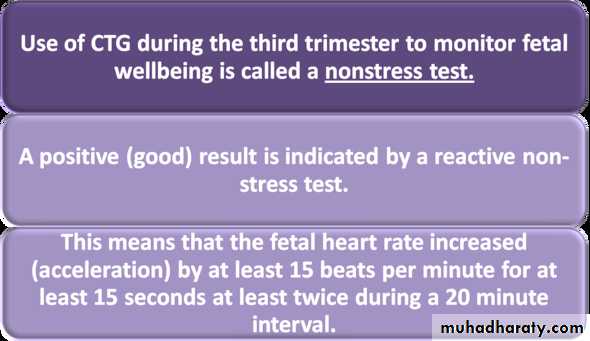
Fetal heart rate accelerations
These are increases in the baseline fetal heart rateof at least 15 bpm, lasting for at least 15 seconds.
The presence of two or more accelerations on a 20–30-minute CTG defines a reactive trace and is indicative of a non-hypoxic fetus, i.e. they are a positive sign of fetal health.
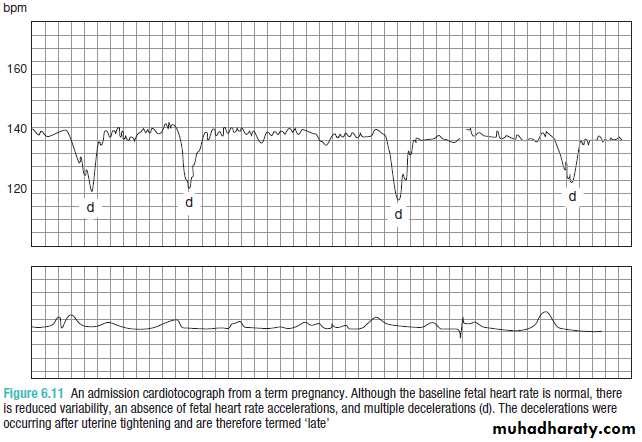
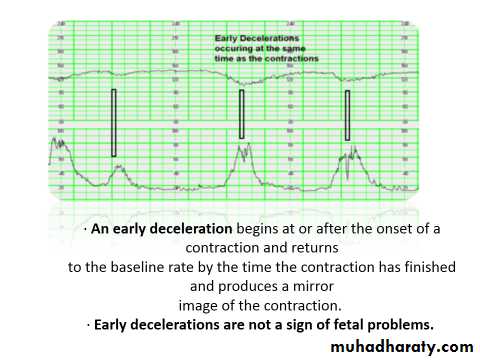
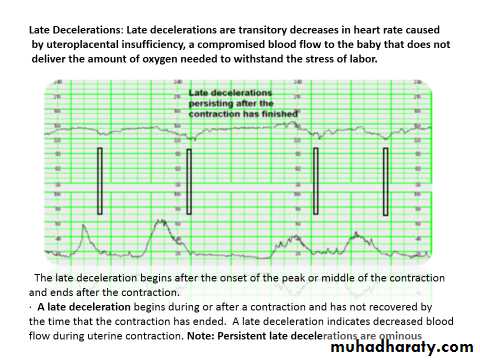
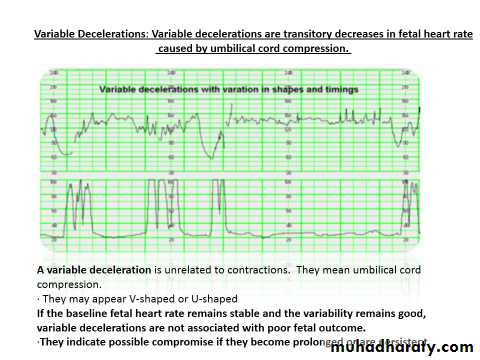
Fetal heart rate decelerations
These are transient reductions in fetal heart rate of 15 bpm or more, lasting for more than 15 seconds.Decelerations can be indicative of
1-fetal hypoxia2-umbilical cord compression.
There is a higher chance of hypoxia being present if there are additional abnormal features such as reduced variability or
baseline tachycardia.
normal antepartumfetal CTG
From the above descriptions, a normal antepartum
fetal CTG can therefore be defined as a1- baseline of 110–150 bpm,
2-baseline variability exceeding 10 bpm3-more than one acceleration being seen in a 20–30 minute tracing.
suspicious features
1-Reduced baseline variability,2-absence of accelerations and
3-the presence of decelerations.
A suspicious CTG must be interpreted within the clinical context.
A-If many antenatal risk factors have already been identified, a suspicious CTG may warrant delivery of the baby,
B-where no risk factors exist, a repeated investigation later in the day may be more appropriate
The computerized cardiotocograph
Computerized CTG interpretation packages have been developed.These packages have been shown to be equal (or superior) to human interpretation in differentiating normal from abnormal outcome.
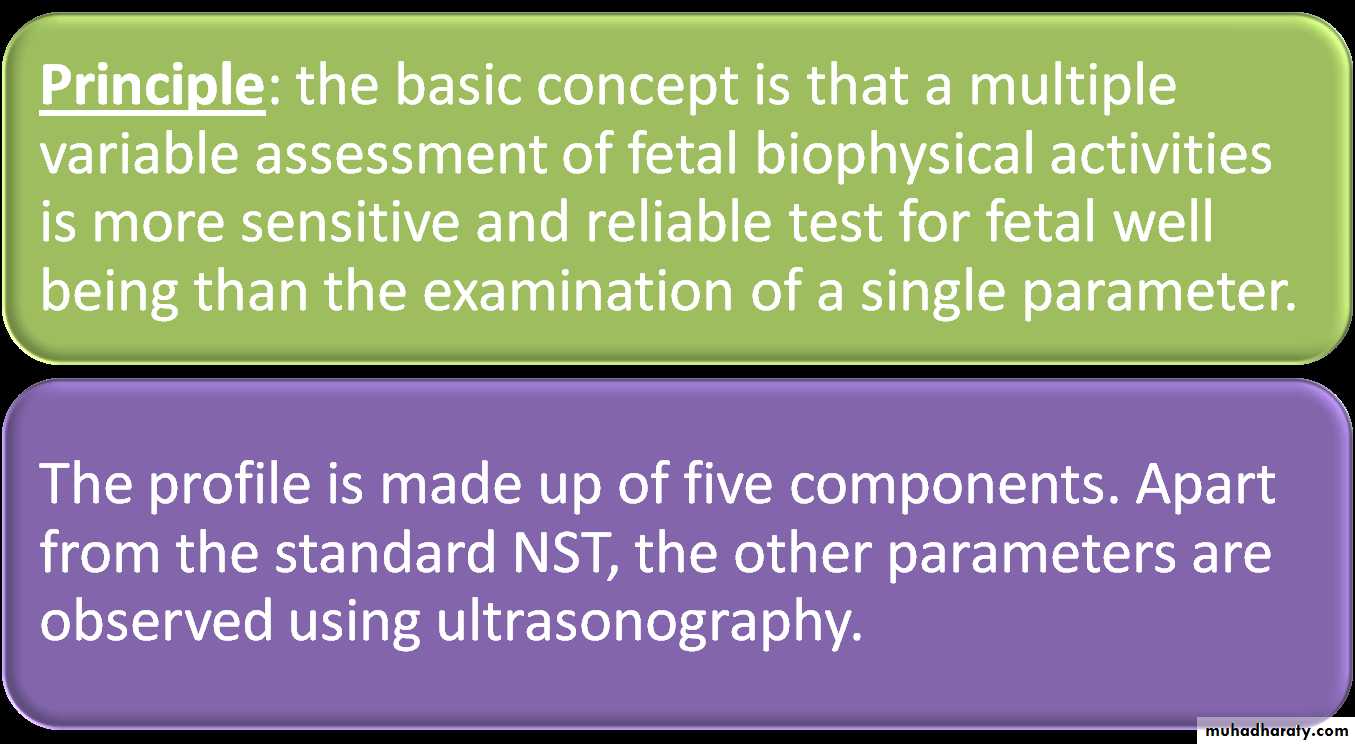
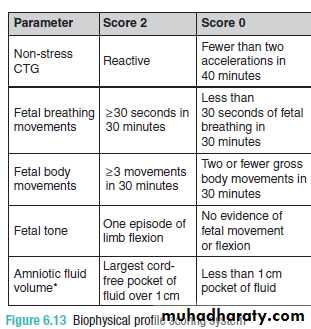
By assigning each of the active variables, and also amniotic fluid volume and the CTG scores of either 2 (normal) or 0 (suboptimal), it is possible to assign an individual fetus score of between 0 and 10.
A score of 0, 2 or 4 is considered abnormal and a score of 8 or 10 normal.
A score of 6 is equivocal and requires repeat within a reasonable timescale (hours) to exclude a period of fetal sleep as a cause
Problems with BPPs
1-Biophysical profiles can be time consuming. Fetuses spend approximately 30 per cent of their time asleep, during which time they are not very active and do not exhibit breathing movements.
2- Another problem with fetal BPPs is that by the time a fetus develops an abnormal score prompting delivery, it is likely to already be severely hypoxic.
Doppler investigation
Waveforms can be obtained from both the umbilicaland fetal vessels.
Data obtained from the umbilical artery provide indirect information about placenta function, whereas data from the fetal vessels provide information on the fetal response to hypoxia.
Umbilical artery
Waveforms obtained from the umbilical artery provide information on placental resistance to blood flow and hence indirectly placenta ‘health’ and function.An infarcted placenta secondary to maternal hypertension, for example, will have increased resistance to flow
Normal umbilical arterial Doppler waveform
Reverse end diastolic flow in the umbilical arteryusing this technique in clinical practice have looked at resistance to flow, which is reflected in the diastolic component.
A small amount of diastolic flow implies high resistance downstream to the vessel being studied and implies low perfusion .
A high diastolic component indicates low downstream resistance and implies high perfusion.
A measure of the amount of diastolic flow relative to systolic is provided by several indices, such as the pulsatility index or resistance index, which essentially compare the amount of diastolic flow to systolic flow.
When these indices are high, this indicates high resistance to flow; when the indices are low, resistance to flow is low.
Reduced end diastolic flow in umbilical arterycompared to normal
Normally, diastolic flow in the umbilical artery increases (i.e. placental resistance falls) throughout gestation. Absent or reversed end-diastolic flow in the umbilical artery is a particularly serious development with a strong correlation with fetal distress and intrauterine death.
Doppler ultrasound benefit
1- in high risk pregnancy (especially those complicated by hypertension or presumed impaired fetal growth) was associated with a trend to a reduction in perinatal deaths.
2-The use of Doppler ultrasound was also associated with fewer inductions of labour and fewer admissions to hospital without reports of adverse effects.
Fetal vessels
Falling oxygen levels in the fetus result in a redistribution of blood flow to protect the brain, heart and adrenal glands, and vasoconstriction in all othervessels.
Several fetal vessels have been studied, and reflect this ‘centralization’ of flow.
Doppler ultrasound and the prediction ofadverse pregnancy outcome
Doppler studies of the uterine artery during the firstand early second trimester have been used to predict
pregnancies at risk of adverse outcome, particularly
pre-eclampsia.
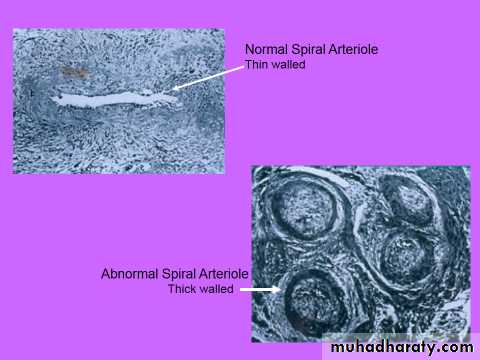
The proposed pathogenic model of pre-eclampsia is one of incomplete physiological invasion of the spiral arteries by the trophoblast, with a resultant increase in uteroplacental vascular
Resistance
Uterine artery waveform with diastolic notch
This is reflected in the Doppler waveforms obtained from the maternal uterine circulation.Doppler ultrasound studies of the uterine arteries may demonstrate markers of increased resistance to flow including the diastolic ‘notch’ in the waveform in early diastole, thought to result from increased vascular resistance in the uteroplacental bed.
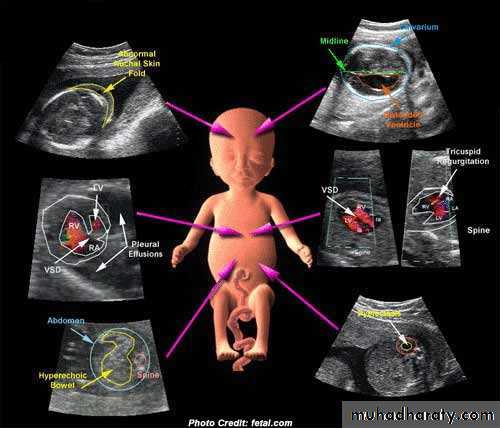
Ultrasound and invasive procedures
Ultrasound is used to guide invasive diagnosticprocedures such as amniocentesis, chorion villus
sampling and cordocentesis, and therapeutic
procedures such as the insertion of fetal bladder
shunts or chest drains.
If fetoscopy is performed, the endoscope is inserted under ultrasound guidance.
This use of ultrasound has greatly reduced the possibility of fetal trauma, as the needle or scope is visualized throughout the procedure and guided with precision to the appropriate place.