Dr.Sumeya
ANTENATAL IMAGING AND
ASSESSMENT OF FETAL WELL-BEING

Obgectives
• The lectures showed the importance and
uses of Ultrasound that is used to date
pregnancies and chart antenatal growth of
the fetus
• To identify congenital abnormalities.
• Doppler can identify placental and fetal blood
• Antenatal tests of fetal well-being .

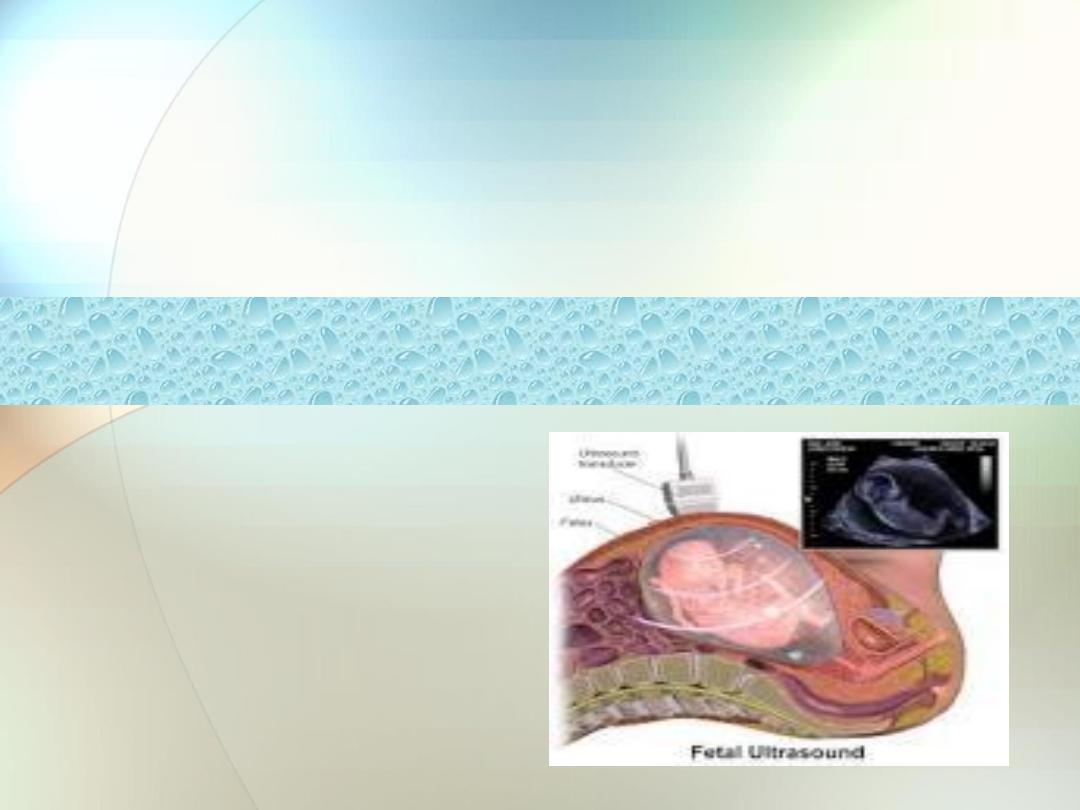
Diagnostic ultrasound in obstetric
practice
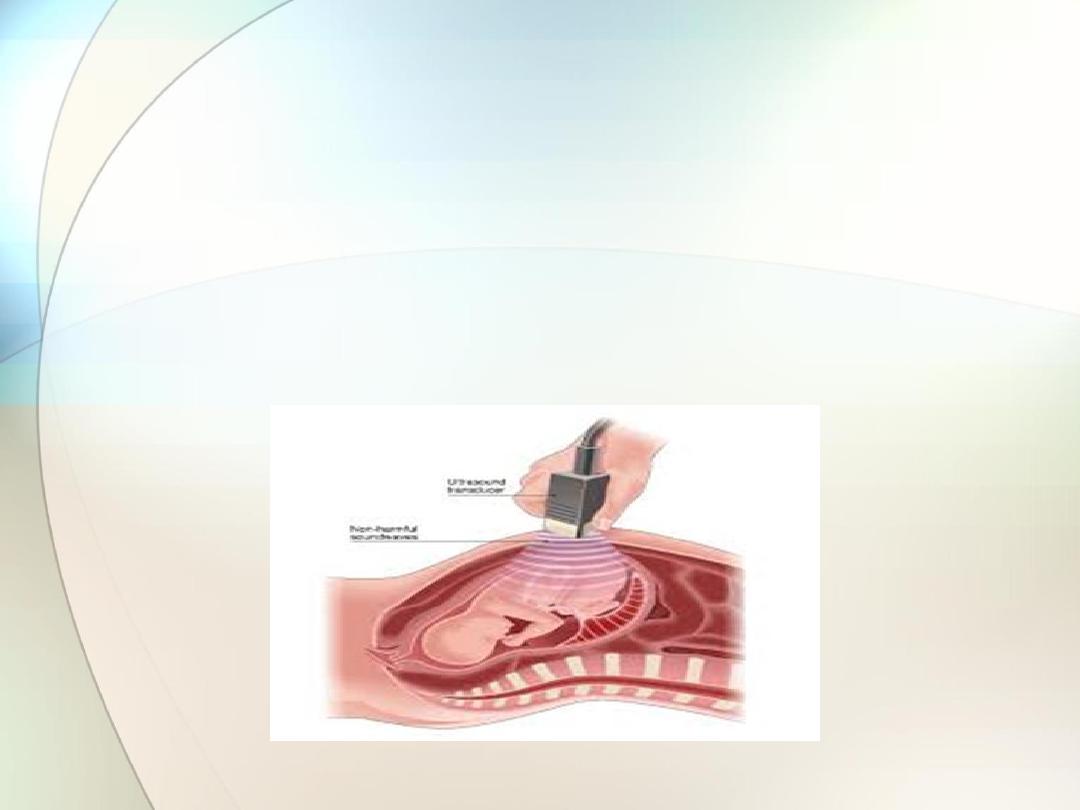
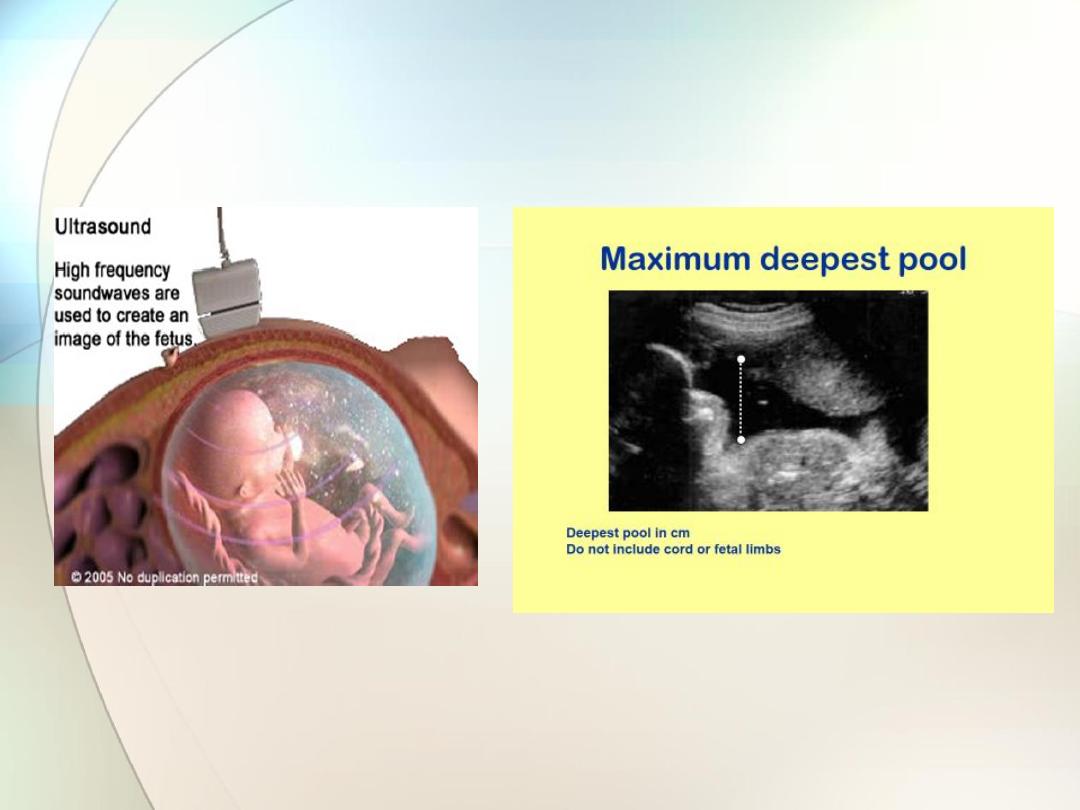
The ultrasound technique uses very high frequency sound
waves of between
3.5 and 7.0 mega hertz
emitted from a
transducer.
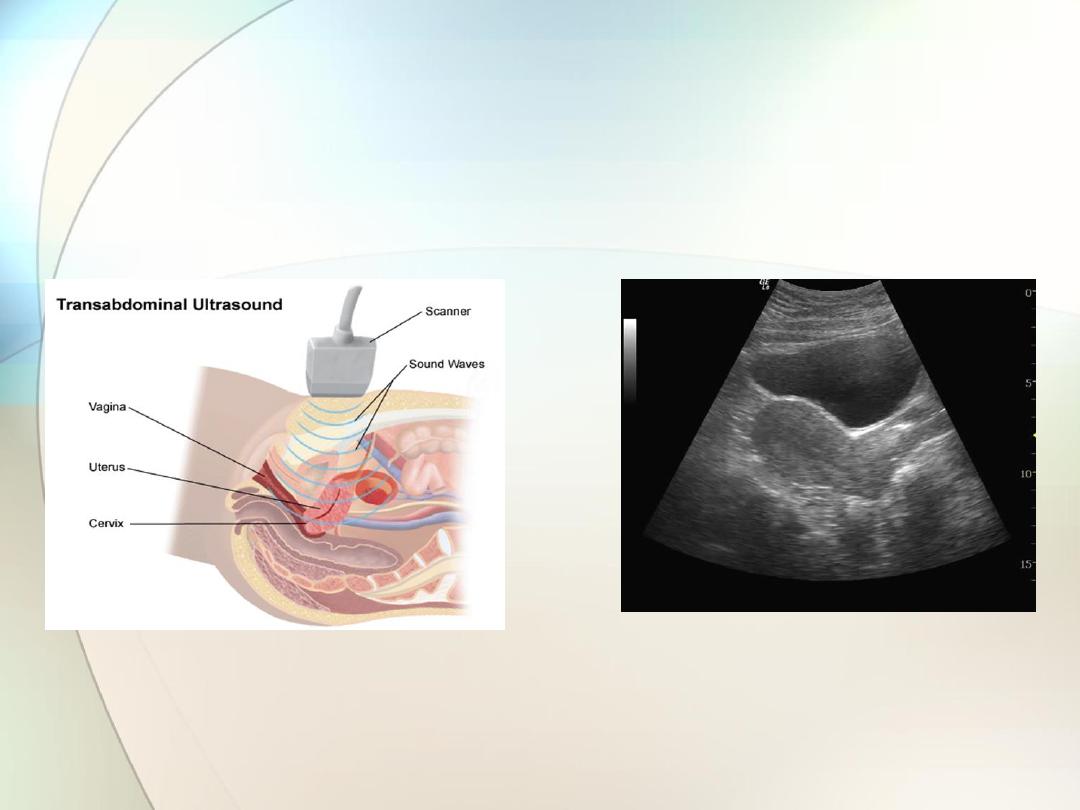
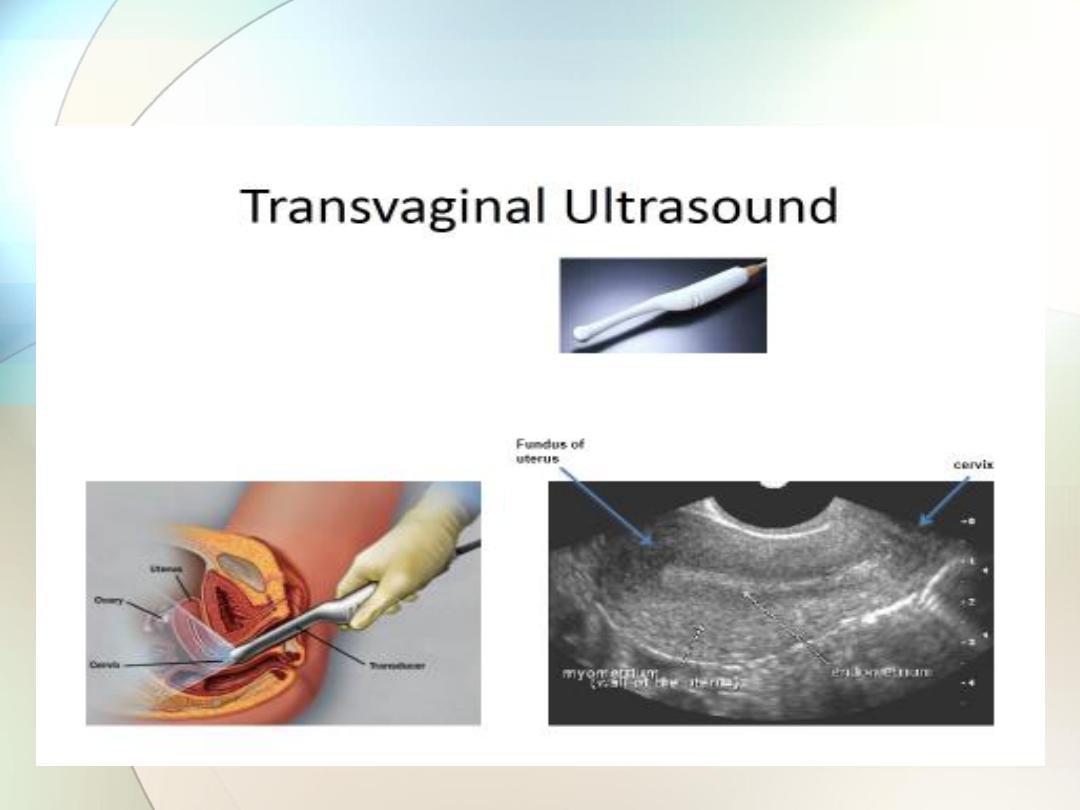
Transducers can be placed and moved across the maternal
abdomen (transabdominal) or mounted on a probe which
can be inserted into the vagina (transvaginal,)
In general, however, after 12 weeks gestation, an
abdominal transducer, which is a flat or curvilinear probe
with a much wider array, is used.

Crystals within the transducer
emit a focused ultrasound
beam in a series of pulses and then receive the reflected
signals from within the uterus between the pulses.
The
strength
of the reflected sound wave depends on the
difference in
‘
acoustic impedance
’ between adjacent
structures.
The acoustic impedance of a tissue is related to
its density;
the greater the difference in acoustic impedance between
two adjacent tissues the more reflective will be their
boundary

The returning signals are transformed into
visual signals
and
generate a
continuous picture of the moving fetus
. Movements
such as fetal heart beat and malformations in the fetus can be
assessed and measurements can be made accurately on the
images displayed on the screen.
Such measurements enable the assessment of gestational
age, size and growth in the fetus.
Ultrasound images obtained can also be processed with
computer software
to produce
three-dimensional (3D)
images
and
even four-dimensional
(moving 3D images) which provide
more detail on fetal anatomical structure and the identification
of anomalies.
Transvaginal ultrasonography is useful in
1- early pregnancy, for examining the cervix.
2-for identifying the lower edge of the placenta.
3-It is also useful in early pregnancy in women with significant
amounts of abdominal adipose tissue .

Ultrasound scanning is currently considered to
be a
1-safe,
2-non-invasive,
3-accurate and
4-cost-effective
investigation in the fetus.

Ultrasound probe; abdominal

Ultrasound probe; trans vaginal
Clinical applications of ultrasound
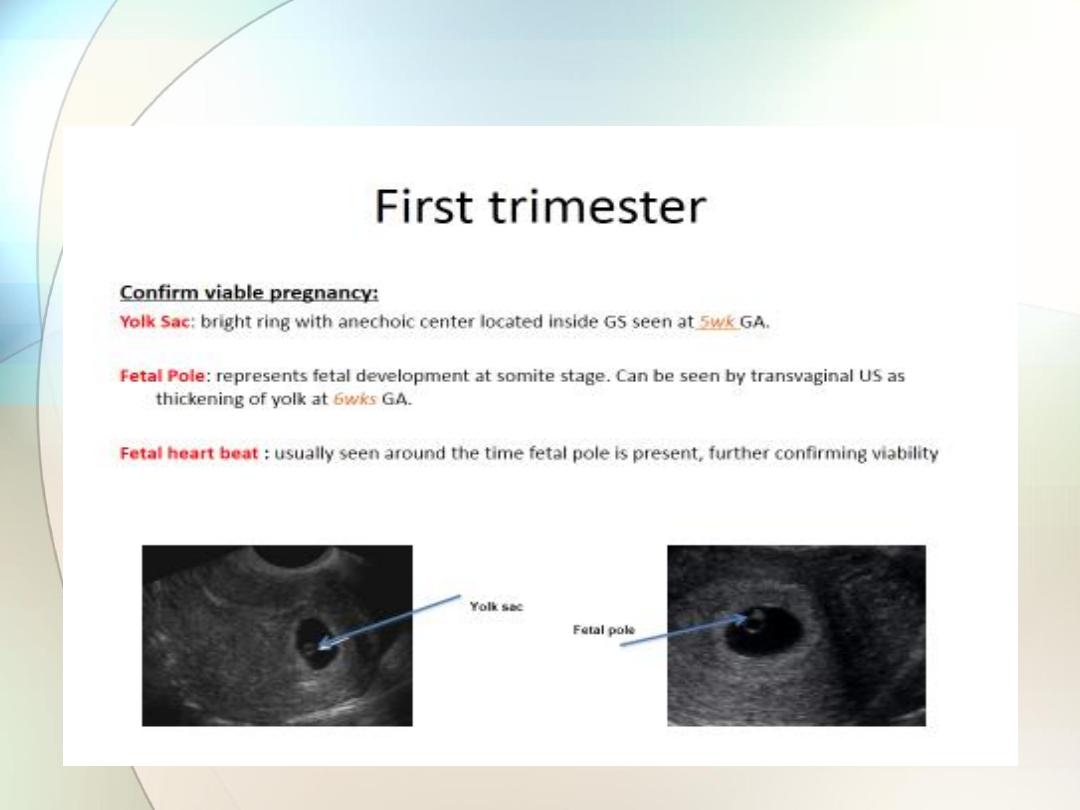
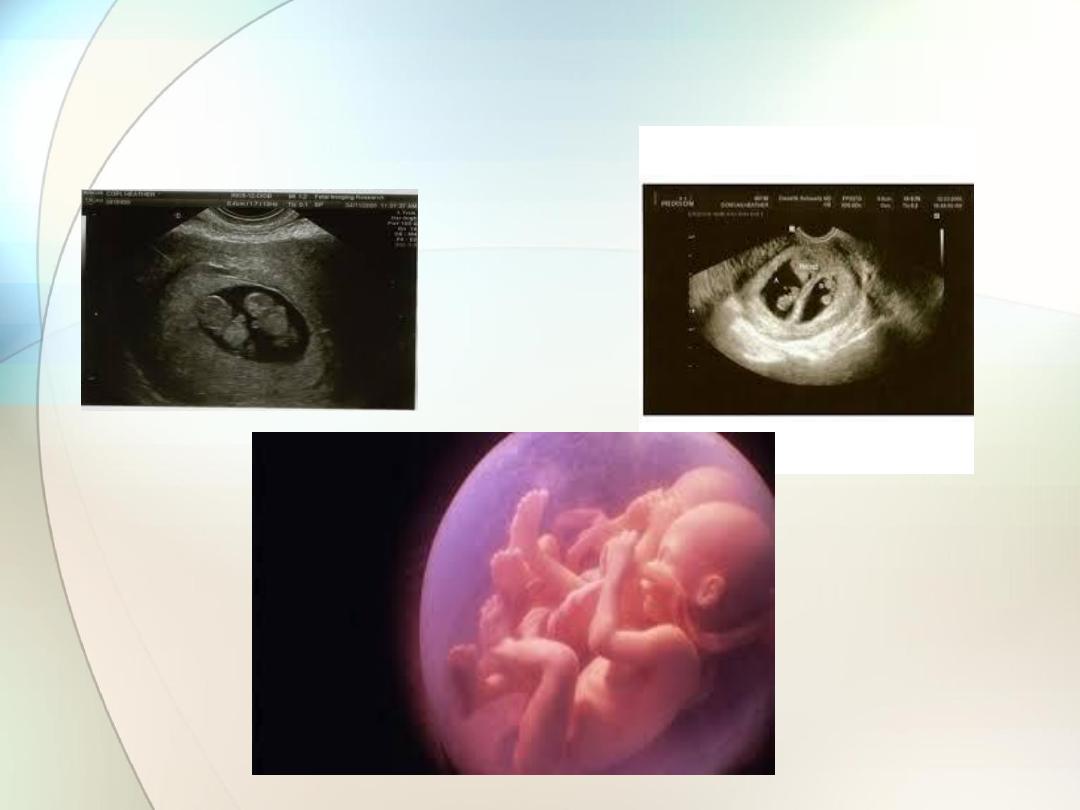
Diagnosis and confi rmation of viability in
early pregnancy
The
gestational sac
can be visualized from as early
as
4
–5 weeks
of gestation and the
yolk sac
at about
5 weeks.
The
embryo
can be observed and measured at
5
–6
weeks
gestation.
A visible
heartbeat
can be visualized by about
6 weeks

Transvaginal ultrasound
Transvaginal ultrasound
plays a key role in the
diagnosis of disorders of early pregnancy, such as
incomplete or missed miscarriage, blighted ovum
where no fetus is present and ectopic pregnancy.
In a
missed miscarriage
, for example, the fetus can be identifi
ed, but with an absent fetal heart and in
a
blighted ovum
, the absence of fetal development results in
the presence of a gestational sac which is empty.
An ectopic pregnancy
is suspected if, in the presence of a
positive pregnancy test, an ultrasound scan does not identify a
gestation sac within the uterus, there is an adnexal mass with
or without a fetal pole, or there is fluid in the pouch of Douglas.
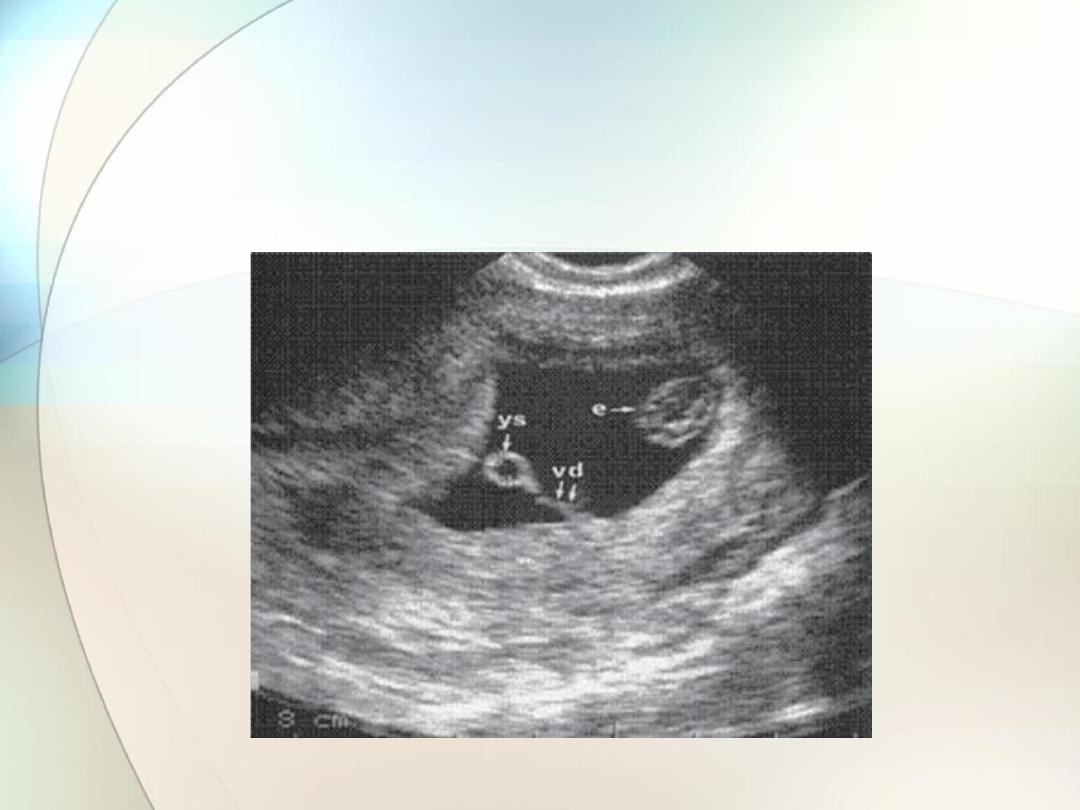
Ultrasound sac showing yolk sac (ys) and
embryo (e) with the vitelline duct (vd)

Ultrasound image showing empty gestation sac
in a case of blighted ovum

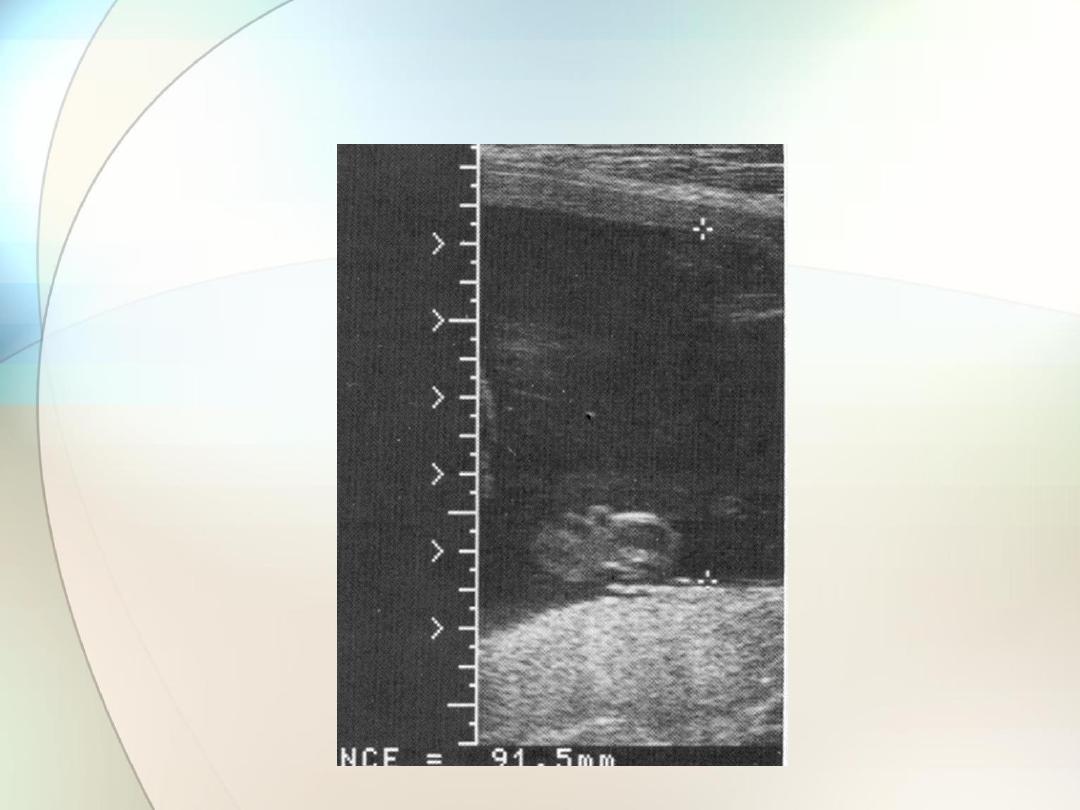
Determination of gestational age and
assessment of fetal size and growth
Up to approximately 20 weeks gestation
the range of values
around the mean for measurements of fetal length, head size
and long bone length is narrow and hence assessment of
gestation based on these measures is accurate.
The
crown-rump length (CRL
) is used up to 13 weeks + 6
days, and the
head circumference (HC
) from 14 to 20 weeks
gestation.
The
biparietal diameter (BPD
) and
femur length (FL)
can
also be used to determine gestational age

Essentially, the earlier the measurement is made, the more
accurate the prediction
In the latter part of pregnancy, measuring fetal
abdominal circumference
(AC)
and
HC
will allow assessment
of the size and growth of the fetus and will assist in the
diagnosis and management of
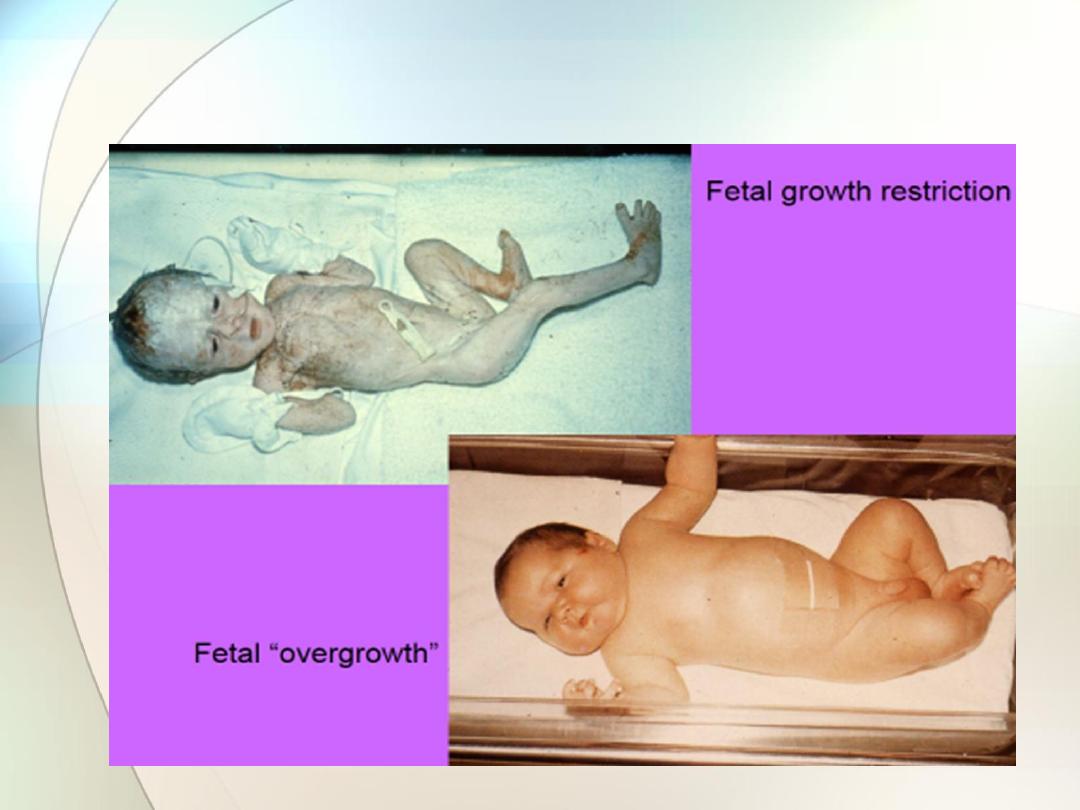
fetal growth restriction
.
In addition to
AC
and
HC
,
BPD
and
FL
, when combined in an
equation, provide a more accurate
estimate of fetal weight
(EFW) than any of the parameters taken singly.

In pregnancies at high risk of fetal growth restriction (FGR),
serial measurements are plotted on the normal reference
range.
Growth patterns are helpful in distinguishing between different
types of growth restriction (symmetrical and asymmetrical).
Asymmetry between head measures (BPD, HC) and AC can be
identified in FGR, where a brain-sparing effect will result in a
relatively large HC compared with the AC .
The opposite would occur in a diabetic pregnancy
, where the
abdomen is disproportionately large due to the effects of insulin
on the fetal liver and fat stores.
Cessation of growth is an ominous sign of placental failure.
Gestational age cannot be accurately calculated
by ultrasound after 20 weeks gestation because of the
wider range of normal values of AC and HC around
the mean.

Biparietal diameter (BPD)

Femur length (FL)
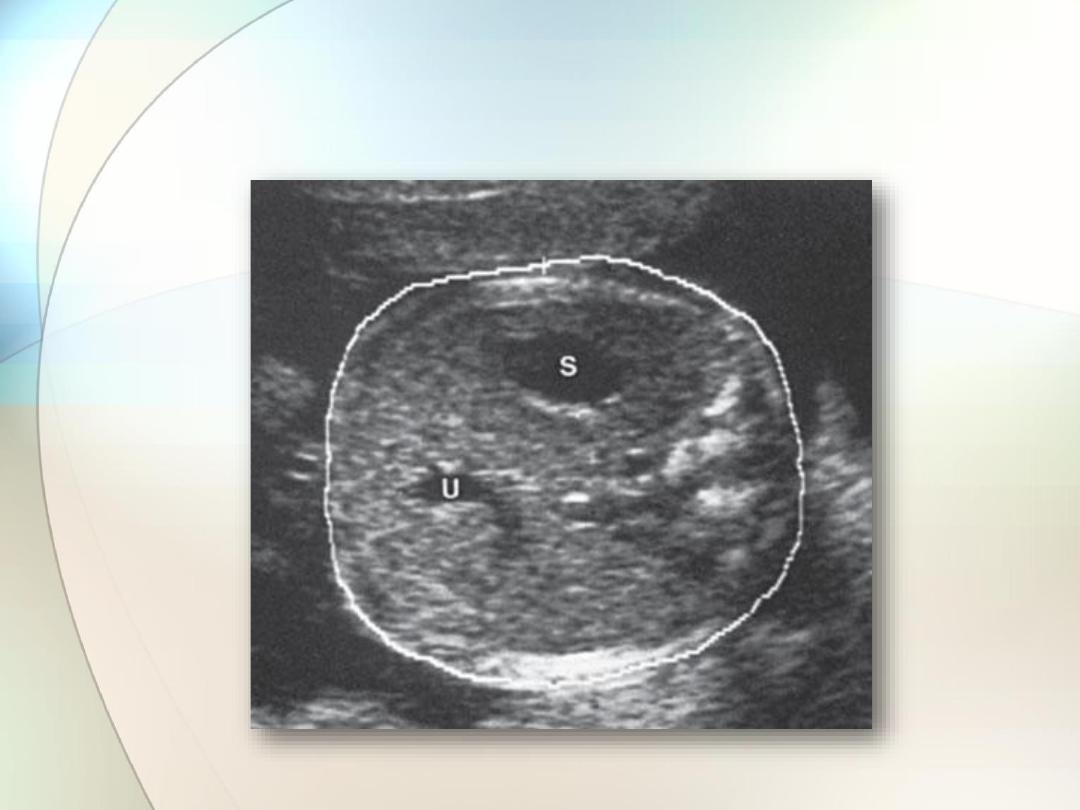
Abdominal circumference (AC) measurement
demonstrating the correct section showing the stomach (S)
and the umbilical vein (U)

crown rump length (CRL)

Multiple pregnancy
Ultrasound is now the most common way in which
1-multiple pregnancies are identified
2-determine the chorionicity of the pregnancy.
Monochorionic
twin pregnancies (i.e. those who
‘share’ a
placenta) are associated with an increased risk of pregnancy
complications and a higher perinatal mortality rate than
dichorionic twin pregnancies.
It is therefore clinically useful to be able to determine
chorionicity early in pregnancy

1-The dividing membrane
in
monochorionic
twins is formed by
two layers of amnion and in
dichorionic
twins by two layers of
chorion and two of amnion.
Dichorionic t
wins therefore have thicker membranes than
monochorionic twins and this can be perceived qualitatively on
ultrasound.
Ultrasonically,
dichorionic
twin pregnancies in the first trimester
of pregnancy have a thick inter-twin separating membrane
(septum).
This is in contrast to a
monochorionic
twin pregnancy, which on
two dimensional ultrasound has a very thin inter-twin septum.

2-Another method of determining chorionicity in the first
trimester
uses the appearance of the septum at its origin from
the placenta.
On ultrasound, atongue of placental tissue is seen within the
base of dichorionic membranes and has been termed the
‘
twin
peak
’ or ‘lambda’ sign
.
The optimal gestation at which to perform such ultrasonic
chorionicity determination is 9
–10 weeks.
3- Dichorionicity will also be confirmed by the identification of
two
placental masses
and later in pregnancy by the presence
of
4-different-sex fetuses.
Ultrasound is also invaluable in the management
of twin pregnancy in terms of confirming
1- fetal presentations, which may be difficult on abdominal
palpation,
2-evidence of growth restriction,
3- fetal anomaly and
4- the presence of placenta praevia, all of
which are more common in this type of pregnancy,
and any suggestion
5-of twin-to-twin transfusion
syndrome.

Early twin dichorionic pregnancy; note the
‘peaked’ inter twin membrane



Diagnosis of fetal abnormality
Major structural abnormalities occur in 2
–3 per
cent of pregnancies and many can be diagnosed by
an ultrasound scan at
around or before 20 weeks
gestation.
Common examples include
1-spinabifida and 2- hydrocephalus, 3-skeletal abnormalities
such as achondroplasia, 4-abdominal wall defects such as
exomphalos and gastroschisis, 5-cleft lip/palate and 6-
congenital cardiac abnormalities.

Detection rates of between 40 and 90 per cent have been
reported. This means that a
‘normal scan’ is not a guarantee of
a normal baby.
A number of factors can influence the success of detecting an
abnormality
.
1-Some are very difficult to visualize.
2- Some conditions, for example hydrocephalus, may not have
been obvious at the time of early scans.
3- The position of the baby in the uterus will influence
visualization of organs such as the heart, face and spine.
Repeat scans are sometimes required if visualization is a
problem.
First trimester ultrasonic
‘soft’ markers for chromosomal
abnormalities such as the absence of fetal nasal bone, an
increased fetal nuchal translucency (the area at the back of the
neck) are now in common use to enable detection of fetuses at
risk of chromosomal anomalies such as
Down
’s syndrome.

Thickened Nuchal Tanslucency (NT):

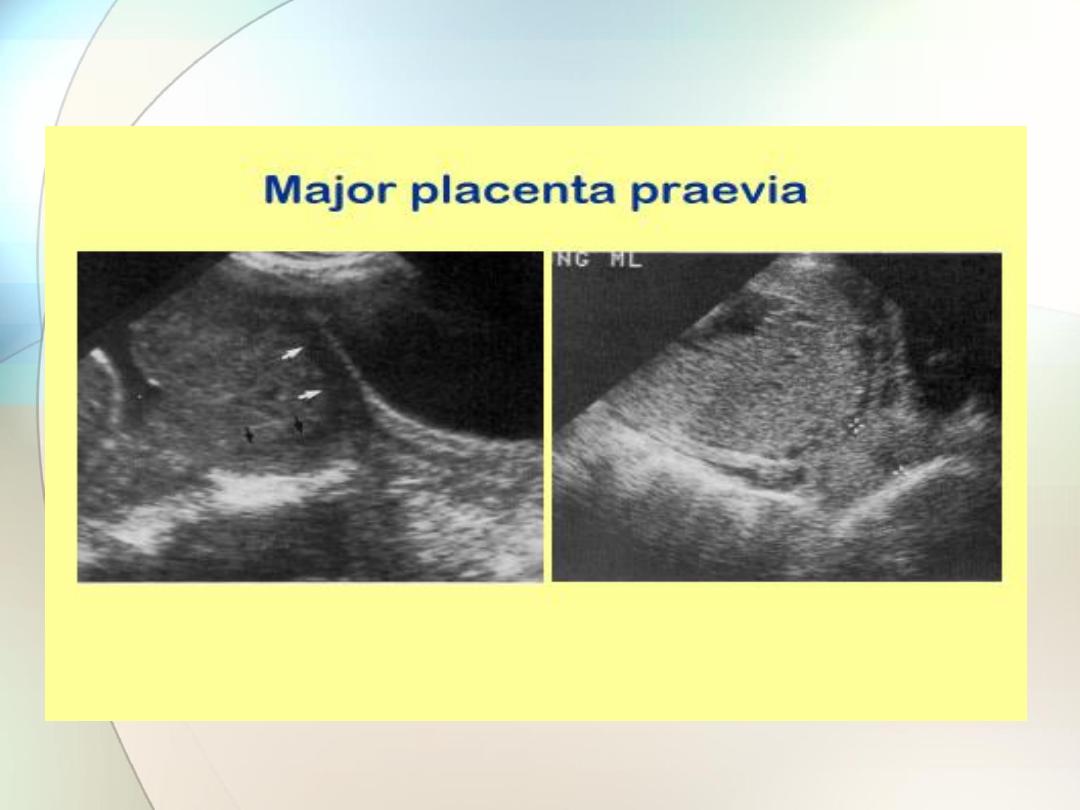
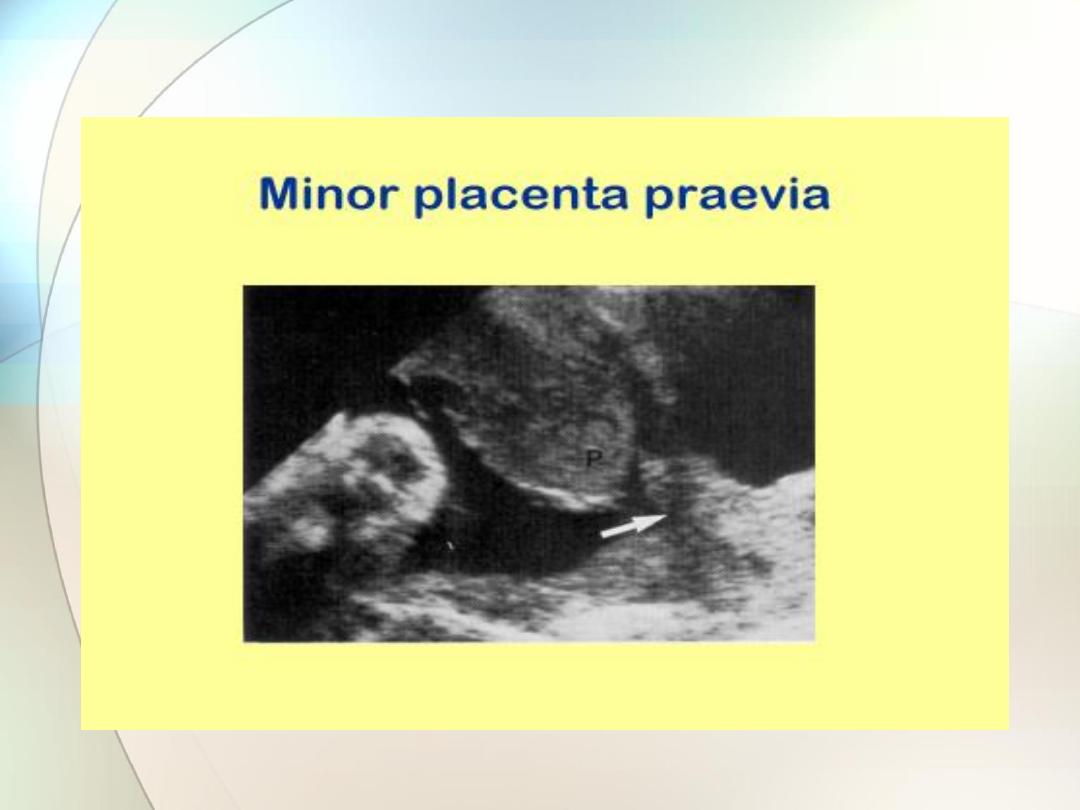
Placental localization
Placenta praevia
can cause life-threatening haemorrhage
in pregnancy.
ultrasonographic identification of the lower edge of the placenta
to exclude or confirm placenta praevia as a cause for
antepartum haemorrhage is now a
part of routine clinical
practice
.
The
transvaginal approach, undertaken with caution,
can be helpful in clearly identifying the lower placental
edge if not seen clearly with an abdominal probe.

At the 20 weeks scan
, it is customary to identify
women who have a low-lying placenta.
At this stage, the lower uterine segment has not yet formed and
most low-lying placentas will appear to
‘migrate’ upwards as
the lower segment stretches in the late second and third
trimesters.
About
5 per cent
of women have a
low-lying placenta at 20
weeks,
and only
5 per cent
of this group will eventually be shown to
have a
placenta praevia
.

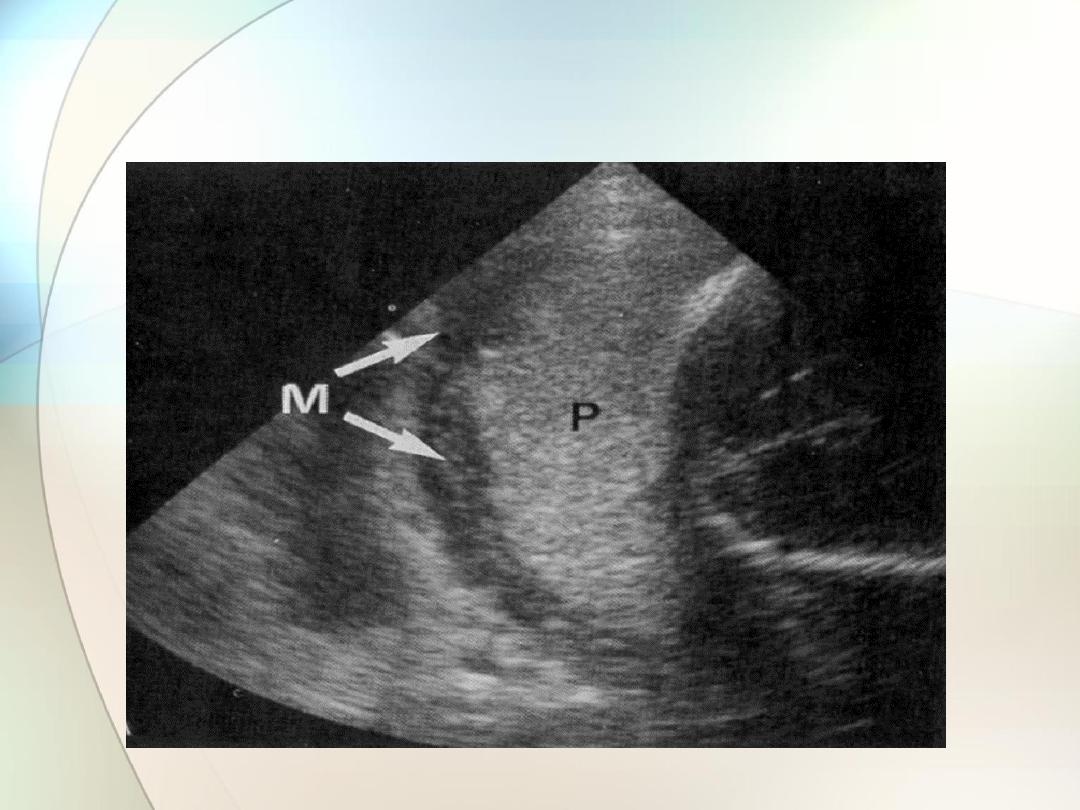
Fundal placenta


Amniotic fl uid volume assessment
Ultrasound can be used to identify both increased and
decreased amniotic fluid volumes.
The fetus has a role in the control of the volume of amniotic fl
uid.
It swallows amniotic fl uid, absorbs it in the gut and
later excretes urine into the amniotic sac.
A-
Congenital abnormalities
that impair the fetus
’s ability to
swallow, for example anencephaly or oesophageal atresia, will
result in an increase in amniotic fluid.
B
-Congenital abnormalities that result in a failure
of urine production or passage, for example renal
agenesis and posterior urethral valves, will result
in reduced or absent amniotic fluid.
Fetal growth restriction
can be associated with reduced
amniotic fluid because of reduced renal perfusion and hence
urine output.

Oligohydramnios
Polyhydramnios
Assessment of fetal well-being
Ultrasound can be used to assess fetal well-being by
evaluating fetal movements, tone and breathing in the
Biophysical Profile.
Doppler ultrasound can be used to assess placental function
and identify evidence of blood flow redistribution in the fetus,
which is a sign of hypoxia.

Measurement of cervical length
Evidence suggests that approximately 50 per cent of
women who deliver before 34 weeks gestation will
have a short cervix.
The length of the cervix can be assessed using transvaginal
scanning.
Other uses
Ultrasonography is also of value in other obstetric
conditions such as:
• confirmation of
intrauterine death;
• confirmation of
fetal presentation
in uncertain cases;
• diagnosis of uterine and pelvic abnormalities
during pregnancy, for example
fibromyomata and ovarian cysts
.

Scanning schedule in clinical
practice
The National Institute for Health and Clinical Excellence (NICE)
recommend that all pregnant women should be offered scans
at between
10 and 14 weeks and 18 and 21 weeks gestation
).

Summary of the
aims of obstetric
ultrasound

The early pregnancy scan (11
–14 weeks)
The principal aims of this scan are:
• to confirm fetal viability;
• to provide an accurate estimation of gestational age;
• to diagnose multiple gestation, and in particular
to determine chorionicity;
• to identify markers which would indicate an
increased risk of fetal chromosome abnormality
such as Down
’s syndrome;
• to identify fetuses with gross structural abnormalities.

The 20 week scan (18
–22 weeks)
The principal aims of this scan are:
• to provide an accurate estimation of gestational
age if an early scan has not been performed;
• to carry out a detailed fetal anatomical survey
to detect any fetal structural abnormalities or
markers for chromosome abnormality;

• to locate the placenta and identify the 5 per cent of
women who have a low-lying placenta for a repeat
scan at 34 weeks to exclude placenta praevia;
• to estimate the amniotic fluid volume.
Also, in some centres:
• to perform Doppler ultrasound examination of
maternal uterine arteries to screen for adverse
pregnancy outcome, for example pre-eclampsia;
• to measure cervical length .

Ultrasound in the third trimester
The principal aims of ultrasound in the third
trimester are:
• • to assess fetal growth;
• • to assess fetal well-being.
Evidence suggests that routine ultrasound in early pregnancy
appears to1- enable better gestational age assessment,2-
earlier detection of multiple pregnancies and3- earlier detection
of clinically unsuspected fetal malformation at a time when
termination of pregnancy is possible.

