the Stomach 2019-20
Dr. Muslim Kandel
1
The stomach
Lecture one
Introduction
Review of Anatomy
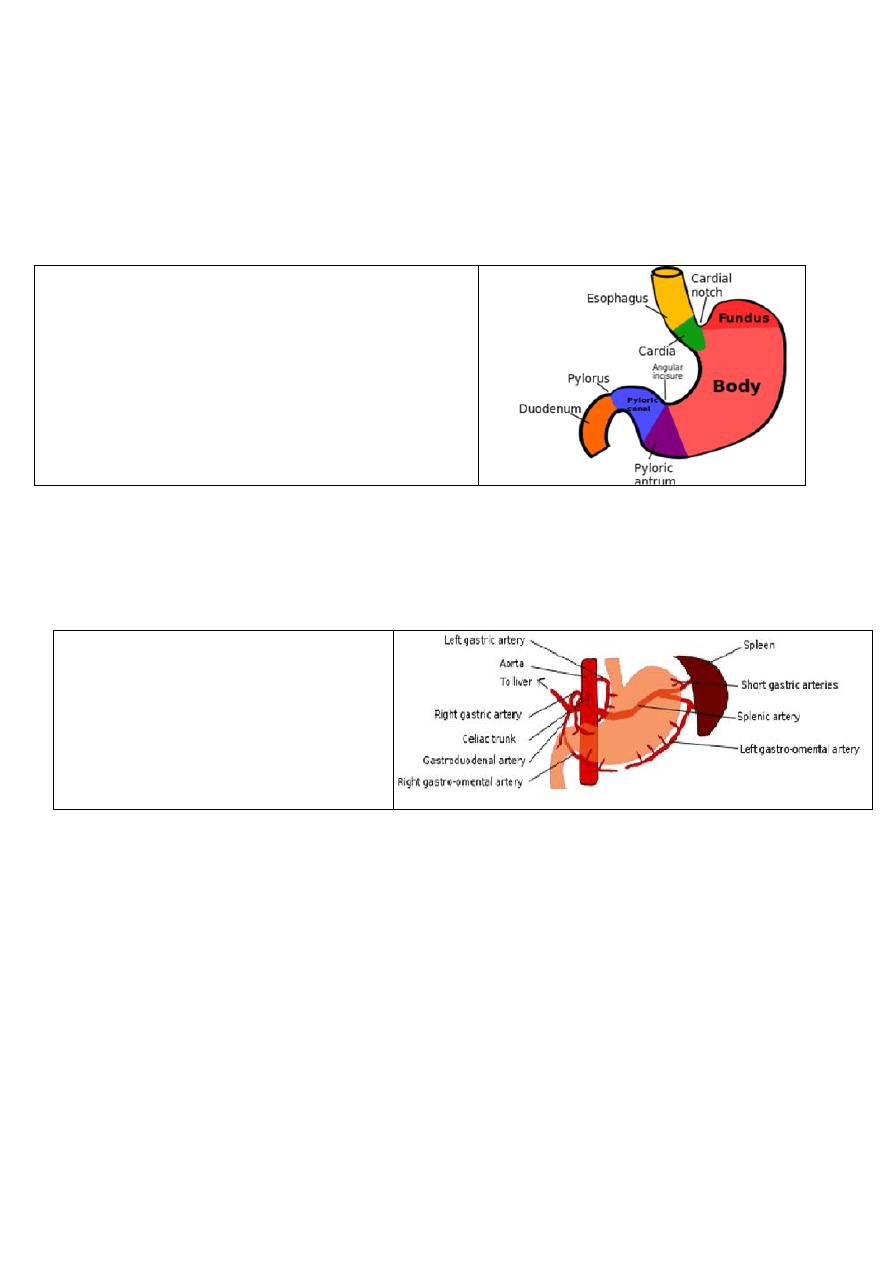
Stomach is “J” shaped flat bag Located in epigastric and , left hypochondriac regions
--Food enters through gastroesophageal (cardiac) sphincter , Food empties into the small intestine at the pyloric
sphincter
Regions of the stomach
1-Cardiac region
2-Fundus
3-Body
4-Pylorus – terminal end
- Lesser curvature is Rt. Border of stomach attached
by lesser omentum to liver
- Greater curvature is Lt border of stomach attached
by greater omentum to colon
Muscles of stomach
1-longtudinal
2-transverse
3- oblique
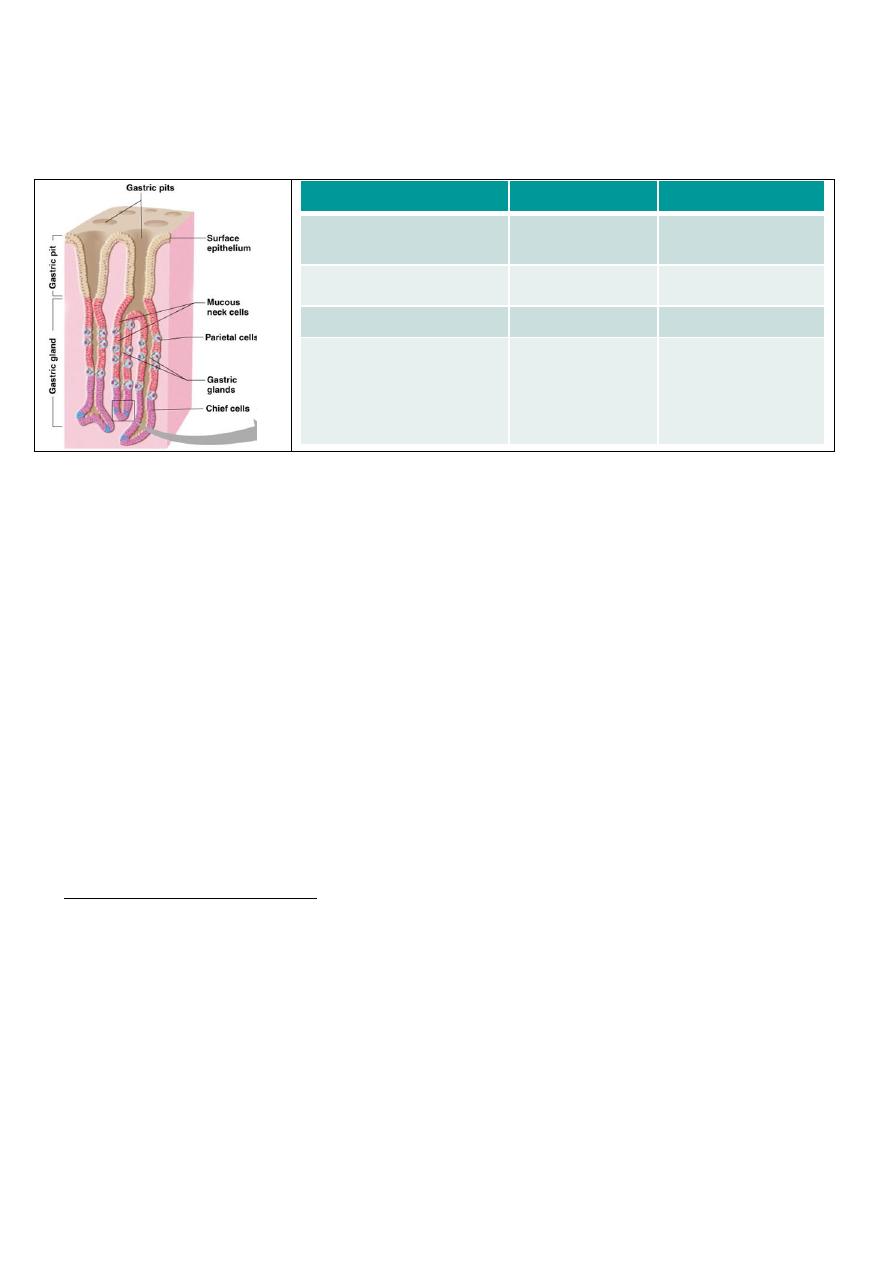
Blood supply
The stomach is richly arterial supply, all arteries which supply stomach , on both lesser and great
curve , arise from caeliac trunk( first major branch of abdominal aorta)
1)-Lt gastric a from caeliac trunk
2) Lt gastroepiploic br. from splenic a
3)Vasa brevia aa br. from
splenic a
4)-Rt gastric a from common
hepatic a
5)Rt gastroepiplioc a from hepatic
Veins
In general the veins are equivalent to the arteries, those along the lesser curve ending in the
portal vein and those on the greater curve joining via the splenic vein.
Rt &Lt gastric vv direct to portal vein
Rt &Lt gastroepiploic vv & short gastric v to Splenic v then to portal v
Lymphatics
The gastric lymph nodes consist of two sets.
1-The Superior set accompany the left gastric artery and are divisible into three groups :
(a) upper, on the stem of the artery;
(b) lower, along the cardiac half of the lesser curvature
c) paracardial around the neck of the stomach. They receive their afferents from the stomach;
their efferents pass to the celiac LN.
2-The Inferior set , four to seven in number, along the pyloric half of the greater curvature of the stomach
Innervation
As with all of the GIT , the stomach and duodenum possess both intrinsic and extrinsic nerve supplies.
a- Intrinsic :
Ganglionic cells ( fundus , antrum)which act as pace maker
Myenteric plexus (Aurbach ) & Sub mucosal plexus . (Meissner)
the Stomach 2019-20
Dr. Muslim Kandel
2
b- Extrinsic :
Parasympathetic ---vagus n(ant , post)
Sympathetic ----caeliac ganglion near caeliac plexus
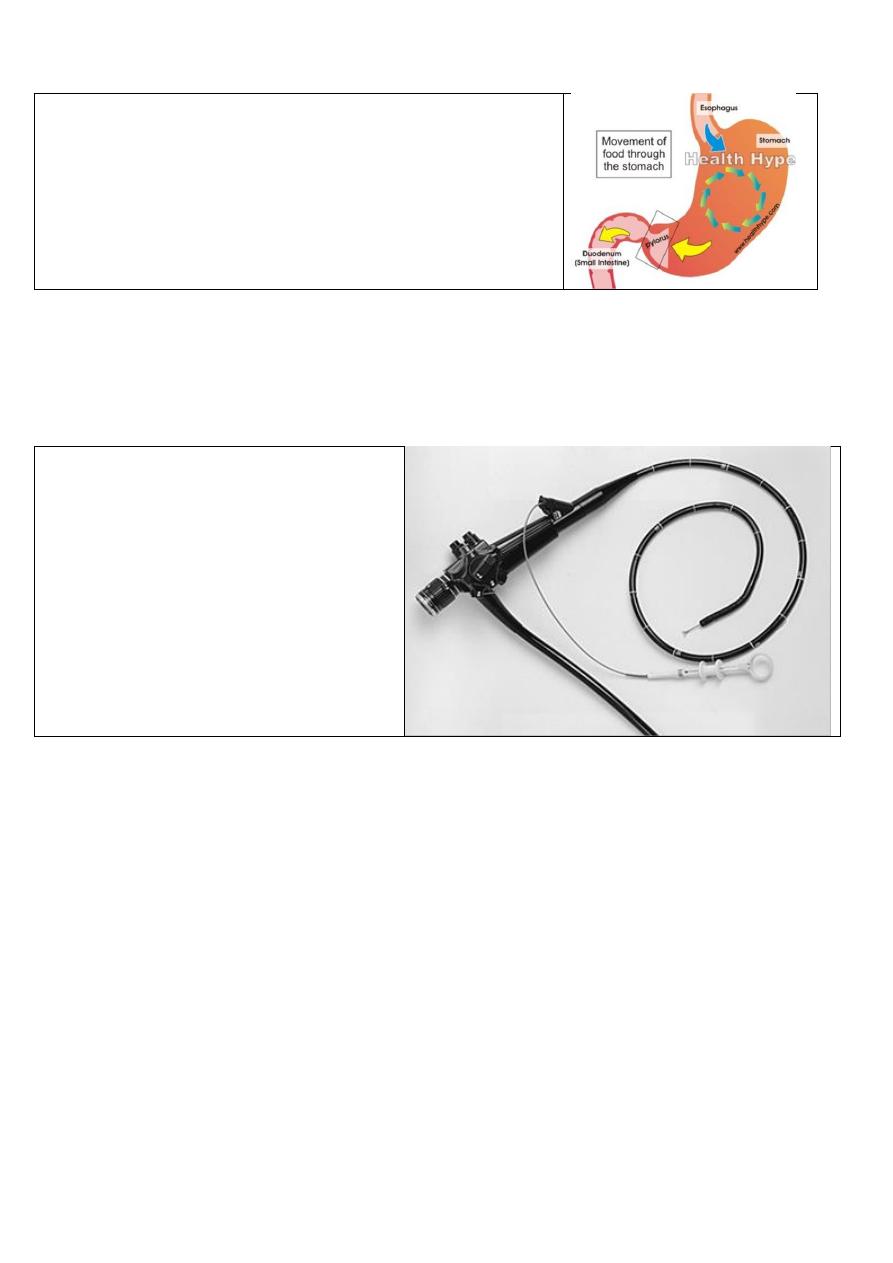
Histological anatomy
Stomach
site
secretion
Type of cell
whole stomach
( mucous
1-Epith cell
(columnar)
distally
HCl)
2- Parietal cell
proximall
(pipsinogen
3-Chief cells
Antrum
whole stomach
body
(gasrten )
somatostatin
(histamin)
4-Endocrin cells:
-G cells
-D cell
-ECL
(entrochromafin
in doudenum
Bruuner glands secrete enzymes (CCK ,secreten)
.
Review of
Physiology
The stomach act as a reservoir for ingested food , which is ingested with in minutes then released
over period of hours , after undergoing pipsin and acid , pass chime into duodenum
Functions of the stomach
reservoir for ingested food
-
--
--- break down foodstuffs mechanically by milling action of peristalsis
--- commence of food digestion by secreasion of acid & pipsin
---protection of mucosa due to these processes
passed these products on into the duodenum.
---
When the chyme that passes into the duodenum. Endocrine cells in the duodenum secrete:
1 --cholecystokinin that stimulates the pancreas to produce trypsin and the gall bladder to contract.
2 --Secretin which inhibits gastric acid secretion and promotes production of bicarbonate by the pancreas.
1- Gastric acid secretion
There is a multiple factors that can act on the parietal cell to produce gastric juice HCl from parietal cell by the
proton pump mechanism
--- stimulatory by vagus and histamine, which acts via the H 2 receptor.
--- inhibitory by gastrin is inhibited by acid, creating a negative-feedback loop.
Acid secretion pass in 3 phases :-
Cephalic phase (vagus) thinking , smell + increase secretion
Gastric phase (food ) by histamine & pp + increase secretion
By gastrin _ inhibit secretion
Intestinal phase (CCK ,secretin ,VIP) _ inhibit secretion
2- Gastric mucus and the gastric mucosal barrier
The gastric mucous layer is essential to the integrity of the gastric mucosa. It is a viscid layer of
mucopolysaccharides produced by the mucus-producing cells of the stomach and the pyloric glands.
Factors break down of this gastric mucous barrier:-
-bile
-,nonsteroidal anti-inflammatory drugs (NSAIDs),
-alcohol,
-trauma and shock.
the Stomach 2019-20
Dr. Muslim Kandel
3
3 –Gastric emptying (Gastroduodenal motor activity)
the migrating motor complex (MMC) start from fundus into pylorus.
Most of the peristaltic activity is found in the distal stomach (the
antral mill) and the proximal stomach demonstrates only tonic activity.
The antral contraction against the closed sphincter is important in the
milling activity of the stomach.
The pylorus, allows only a few milliliters of chime through at a
time.
Motility is influenced by numerous factors including
1- mechanical stimulationof food
2- neuronal
3- endocrine influences
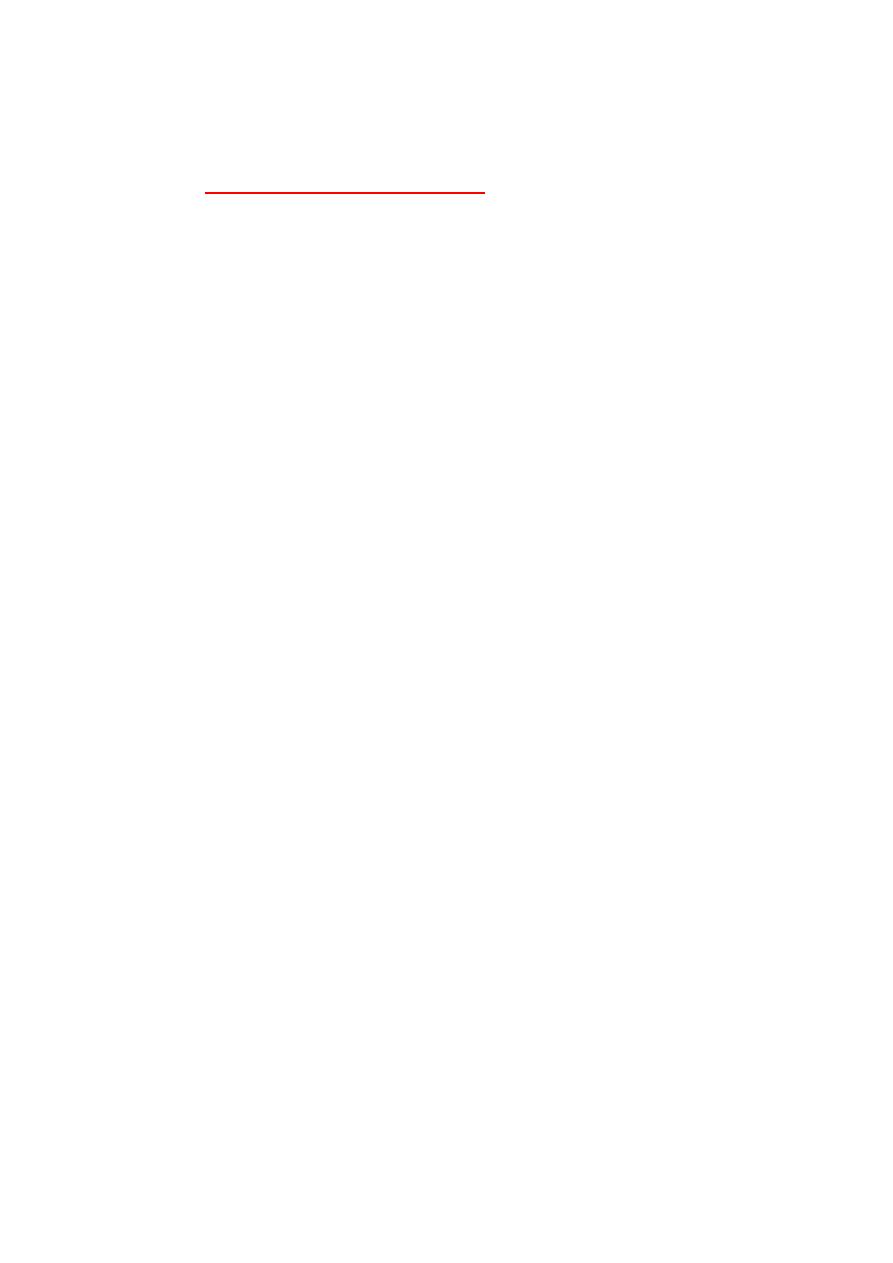
Investigation of the stomach and duodenum
1- Flexible endoscopy
2types
1- fibre-optic old style
2- camera at tip of device The main advantage
of this modern instruments is:-
--not need the fragile fibre optic fibre bundle to
transmit the image.
--use monitor rather than an eyepiece,
This is useful when taking biopsies or
performing interventional
techniques, and also
facilitates teaching and training
.
2-Endoluminal ultrasound with endoscopy now available in many centres
3- Contrast radiology
Now less used as in previous years because endoscopy is a more sensitive
but its better than endoscope in some cases :-
--large hiatus hernias of the rolling type and chronic gastric volvulus
--Linitus plastica may be missed by endoscopists as the mucosal aspect of the stomach may looked
normal.
Ultrasonography
-
4
In patients with neoplasia. Thickening of the gastric wall can be seen in malignancy, some assessment
made of local invasion, and liver and peritoneal disease is often detected
endoluminal ultrasound and laparoscopic ultrasound are probably the most sensitive
5- Computerised tomography (CT) scanning and magnetic resonance imaging (MRI
It is much less accurate in ‘ T ’ staging than endoluminal ultrasound.
6-Laparoscopy for diagnostic and therapeutic
7- Gastric emptying studies
In gastric dysmótility problems, particularly those that follow gastric surgery. Use a radioisotope-
labelled liquid and solid meal are ingested by the patient and the emptying of the stomach is followed on a
gamma camera.
8-Tests of gastric acid secretion and of pH monitoring
a-direct . A nasogastric tube is passed into the stomach, the basal secretion collected
b-indirect (Hollander) test ) use The insulin to induction of hypoglycemia
the Stomach 2019-20
Dr. Muslim Kandel
4
9-Measurement of plasma gastrin
The measurement of plasma gastrin by radioimmunoassay is of use in the diagnosis of gastrinoma
(Zollinger—Ellison syndrome). In most assays the normal fasting gastrin level is about 50 ng/litre, but in
gastrinomas very high levels, sometimes many thousands of ng/litre, can be found.
Acid peptic disease
Lecture tow
Its group of diseases associated with high acid secretion & pepsin such as Gastritis& Peptic
ulcer
Gastritis : inflammation of mucosa of stomach ( either acute or chronic)
Peptic ulcer :extended through sub mucosa &muscular layer may cause hemorrhage. Or
perforation
Helicobacter pylori
Its regarded the aetiology of a number of common GIT diseases such as chr. gastritis DU & gastric tu.
The organism is spiral shaped and is fastidious in its requirements, being difficult to culture outside the
mucous layer of the stomach. One of the characteristics of the organism is its ability to hydrolyse urea,
resulting in the production of ammonia, ( which is a strong alkali.) that stimulat the antral G cells is to
cause increase gastrin induce HCL hypersecretion.
The organism difficult to culture so diagnosis done by its obligate urease activity , there are various
tests used to detect the presence of the organism, including the C 13 and C 14 breath tests and the CLO test
(Campylobacter-like organism test) It is a rapid diagnostic test for diagnosis of H. pylori , The basis of the test
is the ability of H. pylori to secrete the urease enzyme, which catalyzes the conversion of urea to ammonia
and carbon dioxide
Gastritis
type A
: due to autoimmune disease affect Parietal cell , causes atrophy of the parietal cell mass
that will decrease of HCl (achlorhydria. ) + intrinsic factor IF deficiency so the absorption of
vitamin B 12 will affected causes (prencious anemia)
the Antrum not affected, so hypochlorhydria will increase gastrine from G cell and hypertrophy of
the ECL cells microadenomas (Very rarely these tumours can become malignant)
Type B
: due to H pylori affects the antrum, -pangastris, DU , intestinal metaplasia
associated with dysplasia has significant malignant
Reflux gastritis due to Reflux of bile : post gastric operation ( so Bile chelating agents may be
useful in treatment )
Erosive gastritis
This is caused by agents which disturb the gastric mucosal barrier; NSAIDs and alcohol are common
causes. ; NSAIDs inhibit the cyclo-oxygenase type 1 (Cox 1) receptor enzyme, hence reducing the
production of cytoprotective prostaglandins in the stomach.
Stress gastritis
This is a common sequel of serious illness or injury such as burn , head injury and is
characterised by a reduction in the blood supply to superficial mucosa of the stomach.
Others rare (Ménétrier ’ s disease, Phlegmonous gastritis eosenophlic gastritis, Lymphocytic
gastritis
Ménétrier ’ s disease is premalignant condition, characterised by gross hypertrophy of the gastric
mucosal folds, mucus production and hypochlorhydria.
Phlegmonous gastritis is a rare bacterial infection of the stomach
Peptic ulcer
The ulcer occurs at a junction between different types of epithelia, the ulcer occurring in the epithelium
least resistant to acid attack. Common sites for peptic ulcers are
--the first part of the duodenum
-- the lesser curve of the stomach,
--on the stoma following gastric surgery
the Stomach 2019-20
Dr. Muslim Kandel
5
--the oesophagus and even in a Meckel ’ s diverticulum, which contains ectopic gastric epithelium.
Malignancy in peptic ulcer
-- Chronic duodenal ulcers are not associated with malignancy and,
gastric ulcers 5% regarded malignant. Multiple biopsies should always be taken
--prepyloric and pyloric ulcers may be malignant, and biopsy is essential.
--Stomal ulcers occur after a gastroenterostomy or a gastrectomy of the Billroth II type. The ulcer is usually found
on the jejunal side of the stoma.
Clinical features of peptic ulcers
hi acid
No malig
devloped c
hi social
Young
Common
DU
low acid
<5%
developing c
low social
Old
Less
GU
Pain
The pain is epigastric, often described as gnawing and may radiate to the back. Eating may sometimes
relieve the discomfort. The pain is normally intermittent rather than intractable.
Periodicity
One of the classical features of untreated peptic ulceration is periodicity. Symptoms may disappear for
weeks or months to return again. This periodicity may be related to the spontaneous healing of the
ulcer.
Vomiting, it is not a notable feature unless the stenosis has occurred.
Alteration in weight
Weight loss or, sometimes, weight gain may occur. Patients with gastric ulceration are often underweight
but this may precede the occurrence of the ulcer.
Bleeding
All peptic ulcers may bleed. The bleeding may be chronic and presentation with anaemia is not
uncommon. Acute presentation with haematemesis and melaena is discussed later
Investigation
Gastroduodenoscopy
--.In the stomach any abnormal lesion should be multiply biopsied,
--a CLO test performed to determine the presence of H. pylori.
--A ‘ U ’ manoeuvre should be performed to exclude ulcers around the gastro-oesophageal junction.
--if a stoma is present, for instance after gastroenterostomy or Billroth II gastrectomy, it is important to
enter both afferent and efferent loops..
-- Attention should be given to the pylorus
Barium study
For any filling difect , mucosal irrigularity
Treatment of peptic ulceration
A) Medical treatment
1--modifications to the patient ’ s lifestyle, particularly the cessation of cigarette smoking.
2--H 2 - receptor antagonists
Most duodenal ulcers and gastric ulcers can be healed by a few weeks of treatment with these drugs The
problem with H 2 -receptor antagonists is that relapse once treatment is discontinued
3--Proton pump inhibitors(PPI)
All ulcers will heal on proton pump inhibitors, such as omeprazole, lansoprazol the majority within 2
weeks. Symptom relief rapidly, most patients being asymptomatic within a few days. Like H 2
antagonists, omeprazole is safe and relatively devoid of serious side effects. And relapse following
cessation of therapy
4--Eradication therapy
Eradication therapy is now routinely given to patients when suggests that patient has a peptic ulcer and
H. Pylori is the principal aetiological factor (amoxicillin or clarthromycin &metronidazol with PPI )
for 2 weeks then continue other 4 w PPI
B) Surgical treatment of uncomplicated peptic ulceration
Now surgery for uncomplicated peptic ulceration has fallen markedly
Indication : doubt histology

the Stomach 2019-20
Dr. Muslim Kandel
6
Pyloric . prepyloric
Failure of medical Mx
Complication
5y unhealed ulcer
Aims of op : --decrease of acid (so PPI &H2anigonist replace action of operation )
--diversion of acid from ulcer
--both
Operations for GU&DU
1- Billroth I
Distal gastrectomy involve ulcer
2-Gastrojojenostomy with roux en Y
3- Vagotomy :--vagus n section with biopsy of ulcer
a-- truncal v+ drainage to avoid gastric stasis:--
b--selective v
c --highly selective v.
4- Billroth II(Polya)
distal gasrectomy .,duodenum is closed with .gastrojejnostomy with roux en Y
5- Excition of ulcer + vagotomy & drainage
Sequelae
(
Complication
) of peptic ulcer surgery
Early :- 1 -heamorrhage. ,
2-paralytic ileus (truncal vagotomy )
3 -doudenal fistula due to leaking from suture lines
4-stomal obstruction may be due to many causes :-
Oedema ,retrograde intussusption, technical , atonic stomach ,
5-acut pancreatitis
Late :-1) recurrence
2)Gastro-jujeno- colic fistula which causes diarrhea after eating &vomiting of feacal meterial
3)postgastroctomy syndrome
a-small stomach so should be treated by small frequent meals
b-dumping syndrome
early dumping which causes hypotention after eating due to rapid stomach evacuation
late dumping which causes hypoglycaemia after eating due to rapid absorption )
c- Bilios vomiting due to afferent loop obstruction
4)-postvagotomy diarrhea
5)malignent changes
6)malnutrition , Anaemia may be due to either iron or B 12 deficiency.
7)Intestinal Obestruction due to adhesion
8)Gallstone disease due to stasis after vagotomy
the Stomach 2019-20
Dr. Muslim Kandel
7
Lecture tow
The complications of peptic ulceration
The common complications of peptic ulcer are perforation, bleeding and stenosis. ( Gastric outlet obstruction )
I ) Perforated peptic ulcer
)
perforations most commonly occur in elderly female patients.
NSAIDs appear to be responsible for most of these perforations.
--the most common site of perforation is the anterior aspect of the duodenum. However, the anterior or
incisural gastric ulcer may perforate,
--gastric ulcers may perforate into the lesser sac, which can be particularly difficult to diagnose. These
patients may not have obvious peritonitis.
Clinical features
-
Classic presentation is:
**
The patient, have a history of peptic ulceration, develops sudden onset severe generalised abdominal pain
due to the irritant effect of gastric acid on the peritoneum.
shocked with a tachycardia but a pyrexia is not usually observed until some hours after the event.
The abdomen exhibits a board-like rigidity and the patient is disinclined to move because of the pain. The
abdomen does not move with respiration.
-
The less dramatic presentation occur in :
**
1-- elderly patient who is taking NSAIDs specially potent anti-inflammatory drugs.
-- younger athletic patients The rigidity seen in the abdomen of may also not be observed
2
3 --when the leak from the ulcer may not be massive.
*S& S of acute appendicitis due to the fluid may track down the right paracolic gutter.
*Sometimes perforations will seal owing to the inflammatory response and adhesion within the
abdominal cavity and so the perforation may be self-limiting.
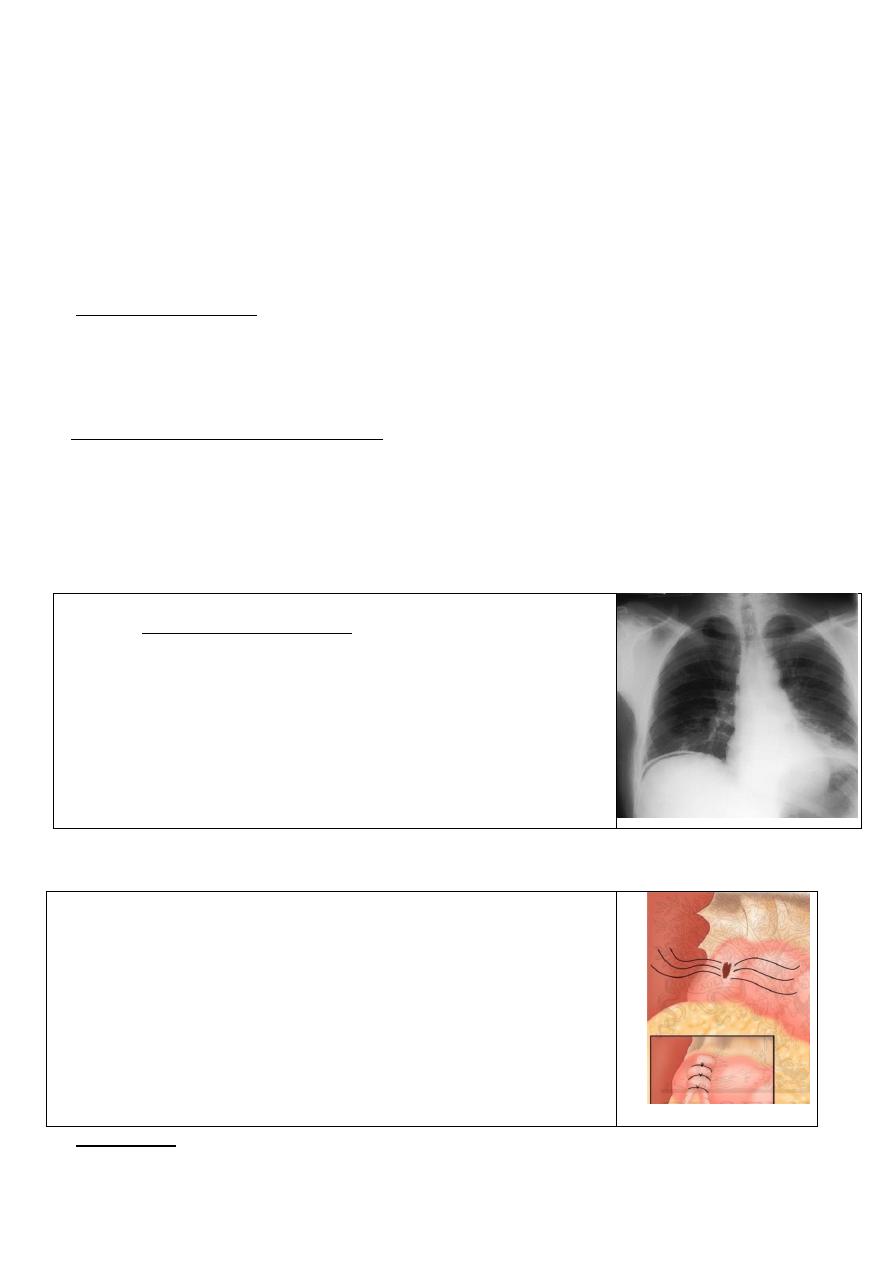
Investigations
1- erect plain chest radiograph
in excess of 50 per cent of cases
free gas under the diaphragm
will reveal
with perforated peptic ulcer
2- serum amylase should performed, as distinguishing between peptic ulcer,
perforation and pancreatitis It can be elevated following perforation of a
peptic ulcer although, fortunately, the levels are not usually as high as the
levels commonly seen in acute pancreatitis.
Several other investigations are useful if doubt remains.
3 - Diagnostic peritoneal lavage will usually easily distinguish between perforation and pancreatitis,
4-ultrasound
5-- CT scan will normally be diagnostic in both conditions, although this is seldom necessary.
Treatment
The initial priorities are resuscitation The analgesia. avoided (which may
mask sign & symptoms) Following resuscitation and the diagnosis being
established the treatment is principally surgical.
Laparotomy is performed usually through an upper midline incision.
laparoscopy may be employed.
The most important component of the operation is a thorough peritoneal
toilet to remove all of the fluid and food debris.
the perforation is in the duodenum it can usually be closed by several well-
placed sutures, with omentoplasty(place an omental patch over the
perforation) the sutures should not be tied so tight that they tear out.
luded.
s should, if possible, be excised and closed, so that malignancy can be exc
Gastric ulcer
--
the Stomach 2019-20
Dr. Muslim Kandel
8
duodenal or gastric perforation such that simple closure is impossible and in these patients a
massive
If
--
Billroth II gastrectomy is a useful operation.
All patients should be treated with systemic antibiotics and there may be some advantage in washing out
the abdominal cavity with tetracycline, 1 g in 1 litre of isotonic saline.
Following operation gastric antisecretory agents should be started immediately(H2 antigonist or PPI).
( In the past many surgeons performed definitive procedures such as either truncal vagotomy and
pyloroplasty , nowadays surgery is omit the peptic ulcer treated medically )
It is important that the stomach be kept empty postoperatively by nasogastric suction, and gastric
antisecretory agents commenced to promote healing in the residual ulcer.
---- In patients with Helicobacter-associated ulcers, eradication therapy is appropriate.
----Patients on NSAIDs, , should have the drug withdrawn and another analgesic substituted.
(II) Bleeding peptic ulcers
the most common causes of haematemesis and melaena is bleeding peptic ulcer 60%, while other
causes like multiple erosions 26% , Mallory—Weiss tear 4% and bleeding oesophageal varices(portal
hypertention) 4% Ca stomach 0.5%,
principles of management
--
resuscitateion
-- IV fluid , blood and fresh frozen plasma ,
--NG tube , urine catheter
--urgently OGD to determine the cause and site of the bleeding.
Medical and minimally interventional treatments
-- H 2 antagonist or a proton pump antagonist,
--tranexamic acid, an inhibitor of fibrinolysis, reduces the rebleeding
rate.
-- Octreotide,( a somatostatin analogue), has not proved effective.
-- endoscopic devices can be used to achieve haemostasis( lasers or
injection apparatus.)
Surgical treatment
Indication of surgery.
-- A patient who continues to bleed
-- A patient who has required more than 6 units of blood in general needs surgical treatment.
--On OGD if Patients have a visible vessel or spurting vessel or an ulcer with a clot in the base
prucedure
The most common site of bleeding from a peptic ulcer is the duodenum: -
-- the duodenum and pylorus are opened longitudinally as in a pyloroplasty. This allows good
access to the ulcer, which is usually found posteriorly or superiorly.
--Accurate haemostasis is important , sutures which under run the vessel.
--in bleeding gastric ulcers the same. The stomach is opened at an appropriate position anteriorly
and the vessel in the ulcer under run. If the ulcer is not excised then a biopsy of the edge needs to be
taken to exclude malignant transformation.
Management of other causes of upper GIT bleeding
Stress ulcer
This commonly occurs in patients with major injury or illness, burn, who have undergone major
surgery or who have major comorbidity.
--The use of prophylaxis. Ranitidine reduce the incidence of stress ulceration,
-- the nasogastric administration of sulcrafate.
There is no doubt that the prevention of this condition is far better than trying to treat it once it occurs.
-- Endoscopic means of treating stress ulceration may be ineffective and operation required. The
principles of management are the same as for the chronic ulcer.
the Stomach 2019-20
Dr. Muslim Kandel
9
Dieulafoy ’ s disease
This is essentially a gastric arterial venous malformation that has a characteristic histological
appearance. Treatment of bleeding due to this malformation is one of the most difficult causes of
upper gastrointestinal bleeding.
The lesion itself is covered by normal mucosa and, when not bleeding, it may be invisible. If it can
be seen whilst bleeding all that may be visible is profuse bleeding coming from an area of apparently
normal mucosa.
Treatment : -
If its seen by OGD injection sclerotherapy
If it is identified at operation a local excision is necessary.
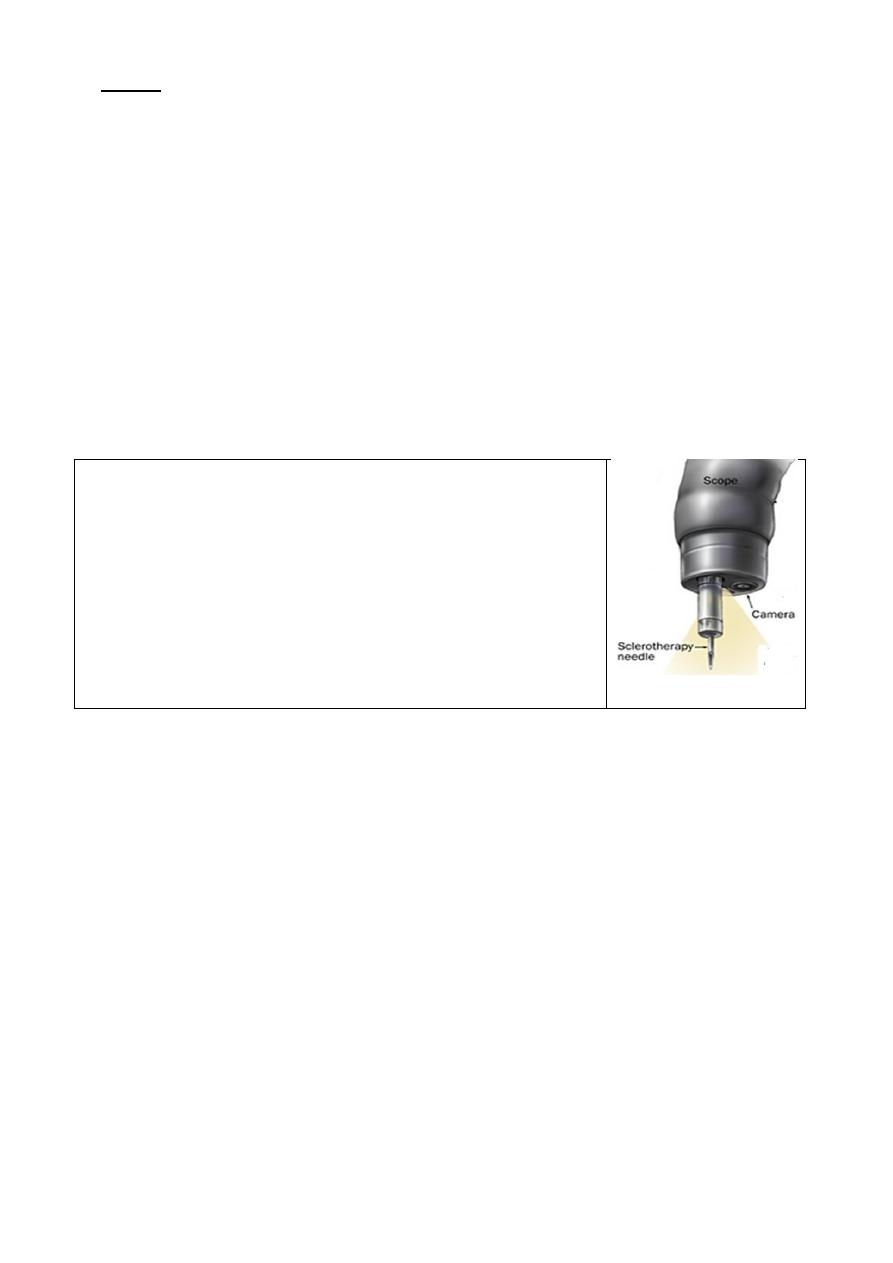
oesophageal varices
due to portal hypertension if suspected should use a Sengstaken may be inserted before an
endoscopy has been carried out.
Gastric erosions
Erosive gastritis especially NSAIDs. Although there is a diffuse erosive gastritis, but fortunately,
most such bleeding settles spontaneously after anti acid
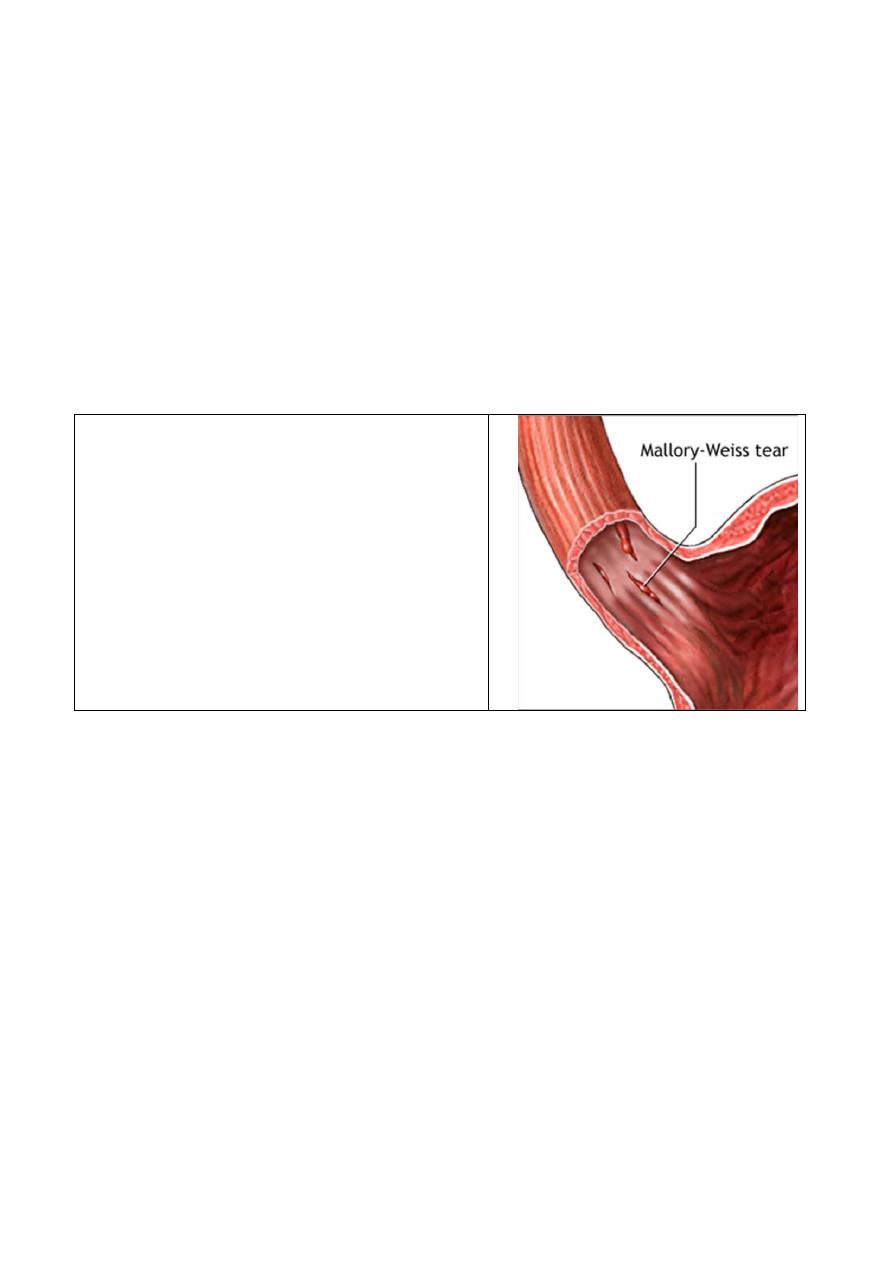
Mallory—Weiss tear
This is a longitudinal tear just below the gastro-
oesophageal junction, which is induced by
repetitive and strenuous vomiting. Sometime cause
of haematemesis
Occasionally these lesions continue to bleed and
require surgical treatment
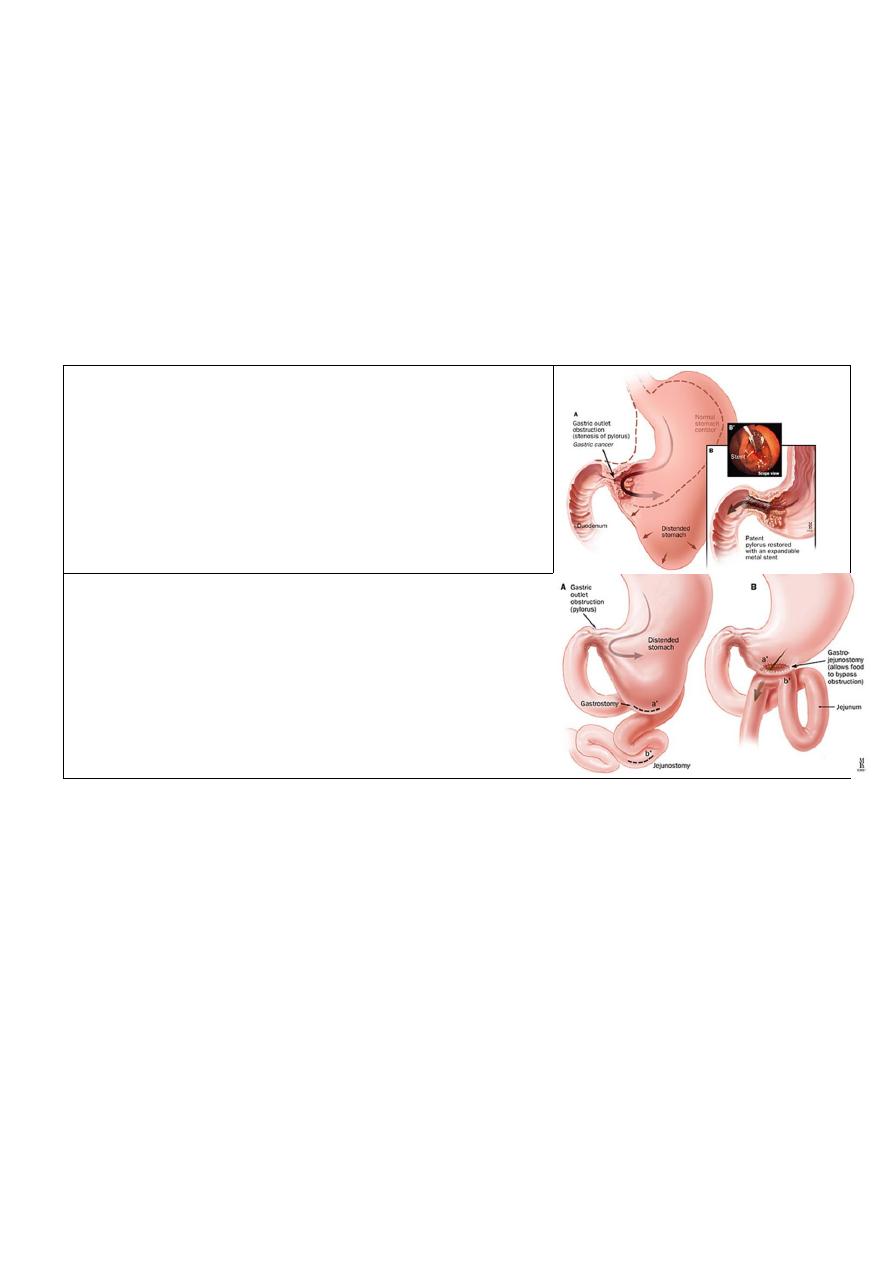
( III )Gastric outlet obstruction
The two common causes of gastric outlet obstruction are gastric cancer and pyloric stenosis secondary to
peptic ulceration.
gastric outlet obstruction should be considered malignant until proven otherwise, at least in the West. Because
decrease in the incidence of peptic ulceration and the advent of potent medical treatments,
Clinical features
there is usually a long history of peptic ulcer disease.
--the pain may become unremitting and in other cases may largely disappear.
--The vomitus is characteristically unpleasant in nature and is totally lacking in bile. Very often it is possible to
recognise foodstuff taken several days previously.
--losing weight, and appears unwell and dehydrated.
-- distended stomach and a succussion splash may be audible on shaking the patient ’ s abdomen.
Metabolic effects
The vomiting of hydrochloric acid results in hypochloraemic alkalosis.
Initially the urine has a low chloride and high bicarbonate content reflecting the primary metabolic
abnormality. This bicarbonate is excreted along with sodium, and so with time the patient becomes
progressively hyponatraemic and more profoundly dehydrated. Because of the dehydration, a phase of
sodium retention follows and potassium and hydrogen are excreted in preference. This results in the
urine becoming paradoxically acidic and hypokalaemia ensues. Alkalosis leads to a lowering in the
circulating ionised calcium, and tetany can occur.
the Stomach 2019-20
Dr. Muslim Kandel
10
Management
Conservative
*Early cases may settle with conservative treatment, presumably as the oedema around the ulcer
diminishes as the ulcer is healed.
--correcting the metabolic abnormality
rehydrated with intravenous isotonic saline with potassium supplementation. Replacing the sodium
chloride and water allows the kidney to correct the acid—base abnormality.
-- treat anaemic,( the haemoglobin being spuriously high on presentation.)
-- A large nasogastric tube (NG tube) The stomach should be emptied. and lavage the stomach until it
is completely emptied.
-- endoscopy and contrast radiology. Biopsy of the area around the pylorus is essential to exclude
malignancy.
--antisecretory agent such as ranitidine, given initially intravenously to ensure absorption
.
Endoscopic treatment
with balloon dilatation has been practised and may be most
useful in early cases. This treatment is, however, not devoid of
problems. Dilating the duodenal stenosis may result in
perforation. The dilatation may have to be performed several
times and sometimes may not be successful in the long term.
bypass surgery
severe cases are treated surgically, usually with a
gastroenterostomy rather than a pyloroplasty. The addition of
a vagotomy in these circumstances may be appropriate
.
Other causes of gastric outlet obstruction
.
Adult pyloric stenosis
This is a rare condition , usually have a long history of problems with gastric emptying. It is commonly
treated by pyloroplasty rather than pyloromyotomy
Pyloric mucosal diaphragm is unknown .cause, usually apparent middle life ,treated simple excision
of the mucosal diaphragm
the Stomach 2019-20
Dr. Muslim Kandel
11
Lecture three
Neoplesia of stomach
a- Benign :-gastric polyps: -
-- metaplastic P ( common) associated with ( H pylori )
--inflammatory P(common)
-- fundic gland P associated. with excessive use PPI & familial polyposis disease.)
--Adenomatous P (tubular or villous)premalig. 10% malignant --
-- carcenoid P increase of (ECL cells) cause precious . anemia
-- Hamartamatous P
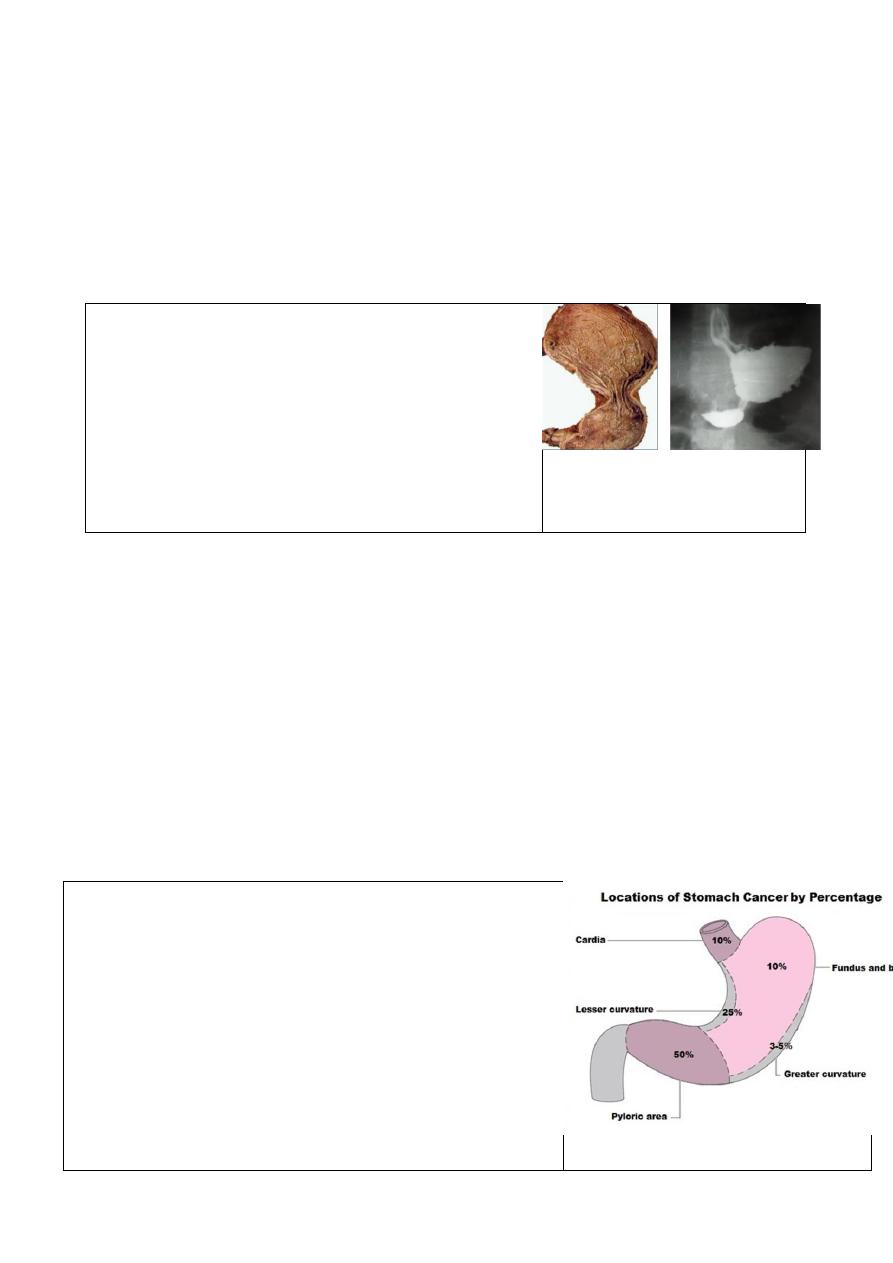
b- Malignant tu.:-
hour glass deformity
1:--Carcinoma ( common)
-- colloid Ca (infiltration of all layers with areolar tissues
,contain geltenous substances , Give classical
Krukenberg phenomenon
--lentis plastica proliferation of fibrous tissues. Specialy
submucosa so in OGD mucsa look normal while Ba
meal look small &distorded
there are 2 types
–generlise which give tea pot , hour glass deformity
--localised causes pyloric obstruction
2--sarcoma
a)--lymphoma ( either primary or part of generalized lymphoma) ,
the Primary lymphoma 2types
--MALT(mucosa Ass. Lymph tissues ) caused by H pylori so treated by eradicated of H pylori
--GALT (gut ass. Lymph tissues )
b)--stroma tu.-- leomyosarcoma –vascular tu.
-- neurofibrosarcoma --fibrosacoma
Carcinoma of stomach
Carcinoma of the stomach has been described as one of the ‘ Captains of the men of death,
Causes :-
its may be environmental disease., its common In Japan approximately 70 per 100 000 per year, and the
incidence is double in small geographical areas in China
1- Premalignent :
-polyp (multiple > single)
-Pernicious Anemia
-dysplesia (Menetrier s dis )gaint rugal hypertrophy
-gastric ulcer
2-Smocking & dust dysplasia
3- Carcinogenic Diet :-
-low anti oxidant(protective )
Aspirin, Diet (high fresh fruit
and vegetable intake, Vitamin C
- High N- nitrous compounds(produced by bacteria)
- spirit
- smocked fish ,dried salted fish(secondary amines)
-common in areas where potatoes major part of diet
-talc treated rice (Japan)
the Stomach 2019-20
Dr. Muslim Kandel
12
4- H. pylori :-
--
H.pylori is cause atrophic gastritis and intestinal metaplasia
that association with to carcinoma of the body and distal stomach
-- its associated with gastric lymphoma.
5--
Family history may increase risk due to
Genetic cause as
blood gr A - Japanies
6- duodenal or jejenal reflux may causes dysplasia as in
drainage procedures (such as Billroth II or Polya gastrectomy,
gastroenterostomy or pyloroplasty )are at approximately four times
the average risk
Clinical features :-
gastric cancer has no specific features to distinguish it symptomatically from benign dyspepsia.
Different presentations Clinical groups
A- new dyspepsia after 40 y
B-insidious onset (tired , weak , anemia , asthenia )
C- lump
D-silent ( body ) obstr. J , ascites , troisieres S trousseures S ,
E-pyloric obstruction
Common presentation
1--early satiety, bloating, distension and vomiting may occur.
2-- anaemia The tumour frequently bleeds resulting in iron deficiency anaemia.
3-- dysphagia, epigastric fullness or vomiting.
4 -- gastric outlet obstruction When pyloric involvement, although the alkalosis is usually less
pronounced or absent compared to when duodenal ulceration leads to obstruction.
5--
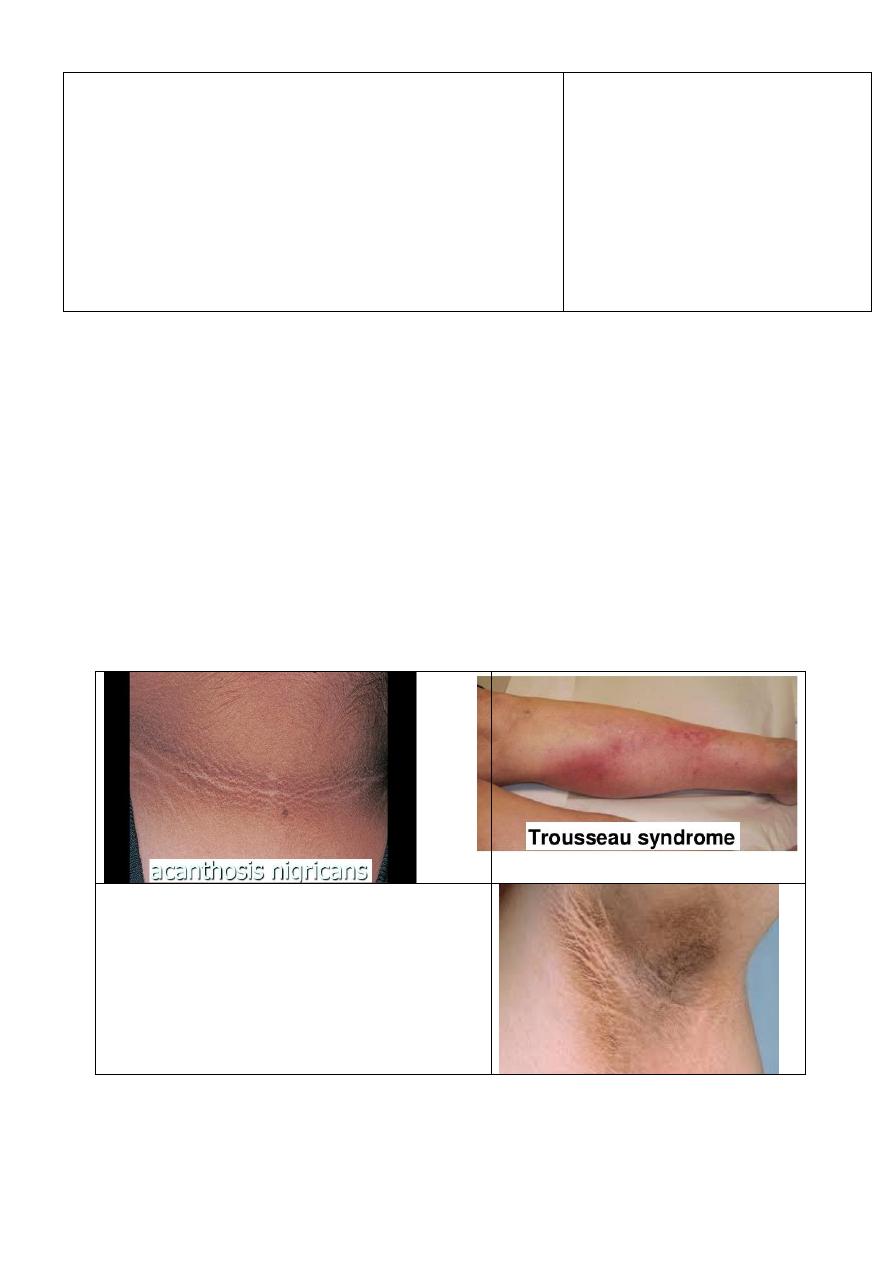
Paraneoplastic syndrome (Nonmetastatic effects )
This a syndrome is not due to the local presence of cancer cells .Is mediated by humoral factors
(by hormones or cytokines) excreted by tumor cells or by an immune response against the tumor
.
Trousseau’s syndrome vessel inflammation due
to
blood clot (thrombophlebitis ) The location of the
clot is tender and the clot can be felt as a nodule
under the skin
–
hyperpigmentation of axilla and groin
;
--
acanthosis nigricans
--
peripheral neuropathy
6-Signs of distant metastasis:
A-Hepatomegally / ascites
B- Krukenbergs tumor refers to a malignancy in the ovary that metastasized from a primary site,
classically the gastrointestinal tract
the Stomach 2019-20
Dr. Muslim Kandel
13
C- Blummers shelf (metastatic tumor felt on PR rectal examination, with growth in the recto uterine
/recto vesical space).
D- Virchow’s node lymph node in the left supraclavicular fossa (the area above the left clavicle)
E-Sister Joseph node at umbilicus (pathognomonic of advances disease)
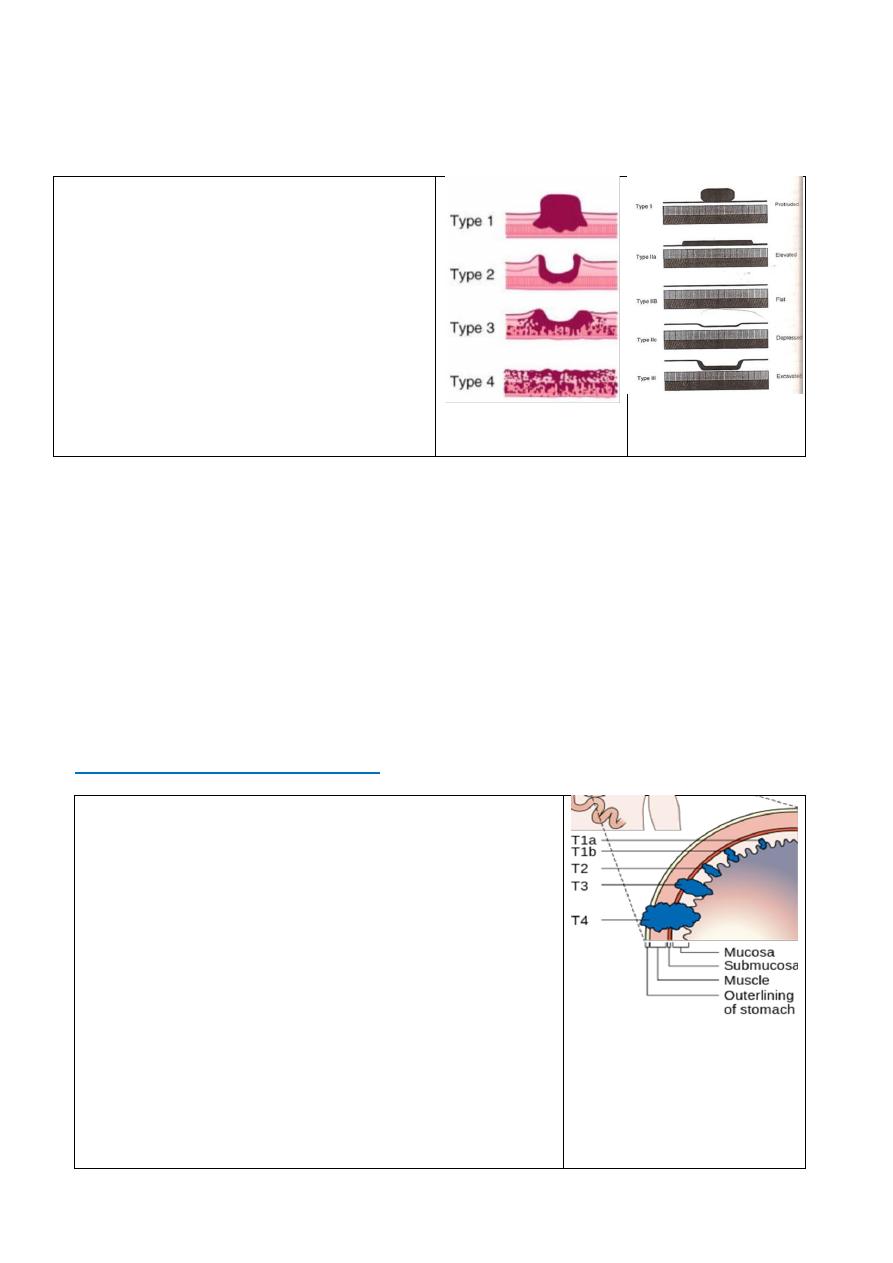
classification
Japanese
classification
Bormann
* Early gastric cancer
the Japanese classification
is defined as cancer
limited to the mucosa and submucosa with or
without lymph node involvement (Ti, any N)
The key to improving the outcome of gastric
cancer is early diagnosis
So in Japan they do OGD for :-
--any new dyspepsia, however mild, in a patient
over 40 years of age.
-- any age with persistent dyspepsia or any
unusual feature.
* advanced gastric cancer appearances have been classified by
Bormann
into four types , gastric
cancer involves the muscularis
Types III and IV are commonly incurable.
Investigations
1--Endoscopy OGD ( with tissue biopsy &US) GOLD STANDARD
- Best pre-operative staging - Needle aspiration of mass under US guidance
-
- Can even give preop neoadjuvant treatment
-
so all Pt >40y with new dyspepsia ,biopsy from any suspicious lesion
2-CT scan (intravenous and oral contrast):
For pre-operative staging
-
--CBP = Hb %PCV,ESR
--Ba study (lintis plastica usually look normal OGD)
-- gastric secretary study (achlorhydria)
-- Diagnostic laparoscopy
STAGING CARCINOMA STOMACH
TNM staging
T categories of stomach cancer
Tis:-Cancer cells are only in the top layer of cells of the mucosa
T1: into the next layers
below the lamina propria,
sub mucosa
.
T1a:
muscularis mucosa
.
T1b:
muscularis propria layer
.
T2:-
subserosa layer
.
T3:
T4:nearby organ (spleen, intestines , pancreas, kidney, etc
N categories of stomach cancer
No spread to nearby lymph nodes
.
N0:
:
1 to 2 nearby lymph nodes
.
N1
:
3 to 6 nearby lymph nodes
.
N2
7 or more nearby lymph nodes
.
N3
7 to 15 nearby lymph nodes
.
N3a
:
16 or more nearby lymph nodes
.
N3b
M categories of stomach cancer
M0:No distant metastasis
.
M1: Distant metastasis
the Stomach 2019-20
Dr. Muslim Kandel
14
Spread :-
--direct abd. Wall ,adjacent structure.
-- lymphatic tiers of LN [N1=LN near stomach 6 gr.,
N2=LN along branches of caecal a 5gr
N3 =LN more distal LN15 gr]
--blood spread liver , spleen …
-- transperitonial (Krukenberg disease ) metastasis to ovary ,colon through peritoneum spread
--Retrograde (downward) spread may occur if the upper lymphatics are blocked. Many centres in the
West now perform surgery that involves a radical lymphadenectomy, but in others both the staging and
surgery are inadequate.
Treatment :-
Management of Ca stomach usually by multidisciplinary team depend on
1- type and stage of cancer, 2- possible side effects ,
3-patient’s preferences and 4- overall health
Surgical treatment
A) Endoscopic Resection of Gastric Carcinoma
Criteria of tumor
< 2cm in size Node negative
-
or Tumor confined on the mucosa Nodes metastasis is < 1cm
-
or tumor < 3 cm No mucosal ulceration No lymphatic invasions
B) Radical resection . resect all tumors, negative margins (5cm) and:-
- adequate lymphadenectomy
- Enbloc resection of adjacent organ is done if needed.
operability :- signs of inoperability which indicate Palliative Mx
–fix to pancreas or post . Abd wall
--gross local involvement
--secondary involvement
--Peritoneal seading
Radical surgery is treatment of choice for gastric cancer Except:
1-unoperable pateint Can’t tolerate abdominal surgery
2-unoperable tumor Overwhelming metastasis
Radical surgery Its curative treatment for gastric cancer
resect all tumors, negative margins (5cm) and adequate lymphadenectomy Enbloc resection of adjacent
organ is done if needed
1) --total gastrectomy ,:-usually indicated in upper
gastric tumor
--Oesophagus will be resected 9cm proximal to. tumor
--Resection of stomach in bloc with greater &lesser
omentum
--Close of duodenum .
-- oesophago-jejenostomy or stomach reservoir (S or W )
-- lymphodenectomy(LN clearance) prepyloric ,
subpyloric , along hepatic art. ,splenic hilum

the Stomach 2019-20
Dr. Muslim Kandel
15
2) --subtotal gasterctomy( distal tu.)
Billoruth I, II with LN clearance this surgery should not done if patient
-
1-Can’t tolerate abdominal major surgery
-
2-Overwhelming metastasis of tu
C) Palliation surgery for non-resective tumors (bypass) gastrojejonostomy used for non-resectable tu.:-
–fix to pancreas or post . wall
--gross local involvement
--secondary involvement
--Peritoneal seading
#other treatment modalities
1- radiotherapy palliative for painfull bone metasteses
2- chemotherapy5FU, cisplatenium epirepucin
In Japan use mitocin C imperegnated charcoal
Prognosis :
5y survival 90% in Japan , 70 % inUK

the Stomach 2019-20
Dr. Muslim Kandel
16
Lecture four
Duodenal tumours
Benign duodenal tumours
Duodenal villous adenomas
occur principally in the periampullary region., they are often found in patients with familial
adenomatous polyposis. Indeed, malignant transformation in such adenomas is the commonest cause
of death in patients with polyposis
as they have malignant potential, should be locally excised with histologically clear margins.
Endocrine tumours
A number of endocrine neoplasms occurs in the duodenum. It is a common site for primary
gastrinoma (Zollinger—Ellison syndrome). Other endocrine tumours include carcinoid tumours,
Zollinger—Ellison syndrome
gastrin-producing endocrine tumour is often found in the duodenal loop(, although it also occurs in
the pancreas, especially the head.) It is a cause of persistent peptic ulceration. Before the
development of potent gastric antisecretory agents the condition was recognised by the sometimes
fulminant peptic ulceration which did not respond to gastric surgery
its part of multiple endocrine neoplasia (MEN) type I
24hr PH study a very high basal acid output but no marked response to pentagastrin, as the
parietal cell mass was already near maximally stimulated by pathological levels of gastrin. The
advent of proton pump inhibitors such as omeprazole has rendered this extreme endocrine condition
fully controllable, but also less easily recognized
Duodenal (periampulary ) adenocarcinoma
.
is term used for juxta-pancreatic carcinomas. They are three forms:-
Carcinoma of the ampulla of Vater
Carcinoma of the lower CBD
Duodenal carcinoma
Clinical Features
--obstructive jaundice ( common )due to Direct involvement in the ampulla of Vater (CBD
obstruction )
It is characteristically painless jaundice but may be associated with nausea and epigastric discomforlart.
Courvoisier law (painless jaundice with an enlarge of gall bladder (periampullary or pancreatic
tumor )
--anorexia and weight loss.
-- anaemia due to ulceration of the tumour
-- intestinal obstruction ( in advance cases) as the polypoid neoplasm begins to obstruct the duodenum.
-- ascitis due to metastases are commonly to regional lymph nodes and the liver
Investigation
liver function test (liver enzymes)
TSB (bilirubin) direct &indirect ,
alkaline phosphetase SGOT, SGPT
--Clotting study (bleeding time INR )
--ultrasound scan
--contrast enhanced spiral CT scan This will determine whether or not the bile duct is dilated.
endoscopic ERCP ,
--
Diagnostic to determine site of obstruction
Therapeutic jaundice can be relieved by stent
Management
the Stomach 2019-20
Dr. Muslim Kandel
17
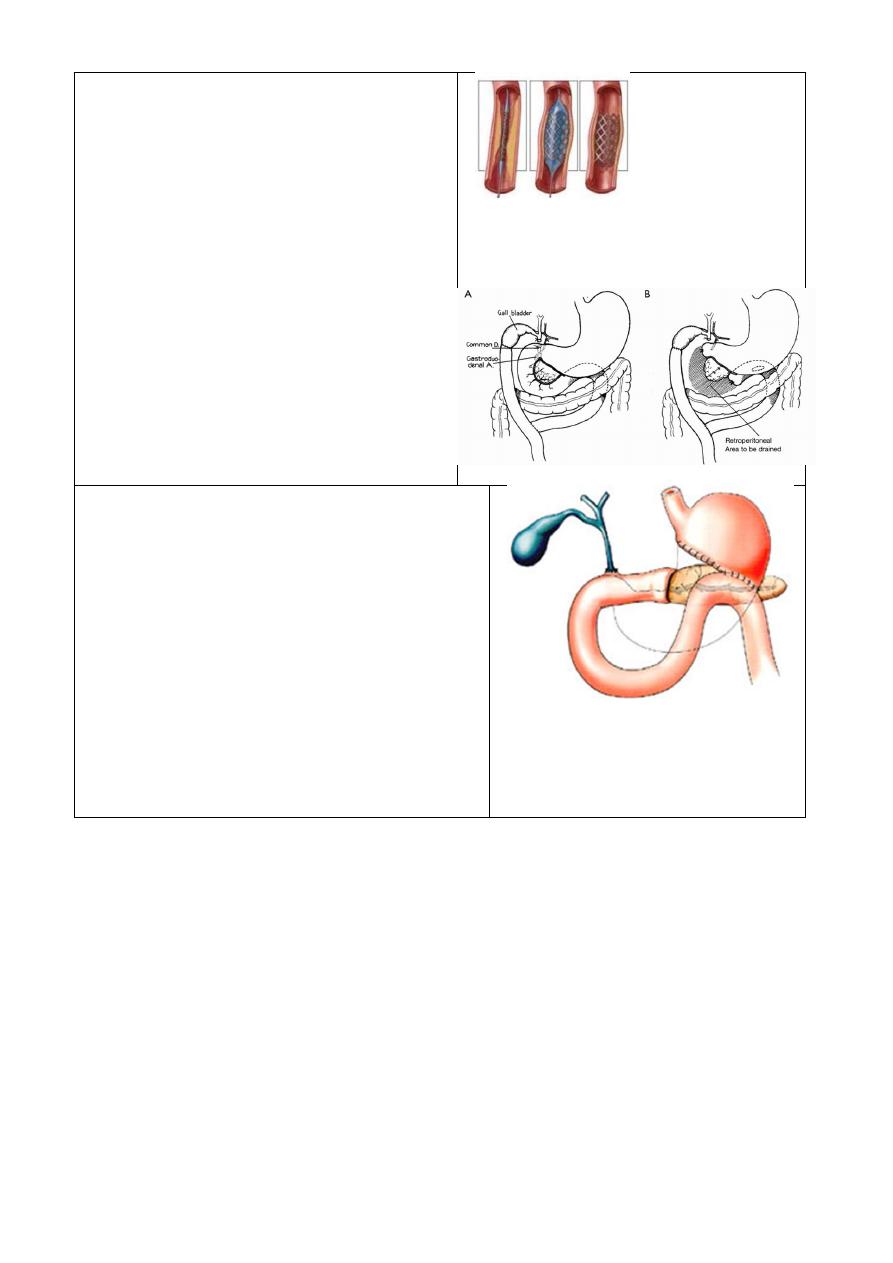
stent
At presentation:
>50% with metastatic disease
40% locally advanced
>90% unresectable tumor palliative Mx
<10% confined disease resectable
I - Palliative Mx: (for unresectable)
For obstructed Jaundice
-- ERCP
(plastic or metal stent )
= occlusion rate of stent 42%
-- bypass surgery
Hepaticojejunostomy
Choledochojejunostomy
Choledochoduodenostomy
Cholecystojejunostomy
II-Resection of tumor :-
pancreaticoduodenectomy (Wipple procedure)
preoperative management.
1- relieve the jaundice
if possible by stent.
assessment of operability of tumour ( locally or LN
metastesis).
2- The clotting study and give vit. K 10mg.
3- adequate hydration IV fluid
4- manitol 10% to avoid hepatorenal syndrome
(precipitation of billirubin in glomeruli)
5-antibiotic
6-A full explanation to the patient is aware of the
diagnosis, the gravity of the operation and the risks
involved, and consent taken
Duodenal obstruction
-- cancer of the head of pancreas is the most common cause.
treated by endoscopic stenting or by gastroenterostomy
--other malignancies can cause duodenal obstruction including metastases from colorectal and
gastric cancer.
-- Primary duodenal cancer is much less common as a cause of obstruction than these other
malignancies.
--Annular pancreas may rarely cause duodenal obstruction.
--follows an attack of pancreatitis
--Arteriomesenteric compression is an ill-defined condition in which it is proposed that the fourth
part of the duodenum is compressed between the superior mesenteric artery and the vertebral
column. Where it is convincingly demonstrated and causing weight loss duodenojejunostomy may
be performed.

the Stomach 2019-20
Dr. Muslim Kandel
18
Other gastric conditions
ACUT GASTRIC DILATATION
It s represent poor post op .care, inadequate treated paraletic ileusgasteric retentionlarge
volume of fluid requisted hypovol. Shock
Fluid &electrolyte disturbances
Vomiting spell into lung (Mendelson syndrome)
Treatment : NG tube , IV fluid
VOLVOLUS OF STOMACH
Rotation occur in around 2 fixed points (cardia & pylorus )
Rotation occur in horizontal (organoaxial ) or vertical (mesntroaxial)due to move of colon upward
to lie under the capula of Lt. diaphragm, the predisposing factor is evanteration of diaphragm
so the colon move up and take stomach with it
CF:- small food cause pain &retching
Dx:- Ba meal
NG tube not inter stomach
Treatment:-
Greater curvature must be completely freed from colon
part of doud. With out stoma
th
Fixation of stomach with DJJ or 4
Closure of hiatal defect
FORGHN BODY
Sharply pointed objects better to remove by gastrectomy ,while rounded ,small objects left to
pass
There is another types of FB :-
1-Trichobezoar (hair –ball)
2- Phytobezaor(vegitable) occr in Pt with stasis
DOUDENAL DIVERTICULUM
parts usually single, arise at portal of entery of blood vessels
rd
&3
nd
at 2
-
:
Primary diverticulum
, may be large div. near ampula obs. J
part as aresult of scarring of DU
st
at 1
-
:
verticulum
Secondary di
BARIATRIC SURGERY
Gastroplasty for morbid obesity
The goal of bariatric surgery is to improve health in morbidly obese patients by achieving long-term,
durable weight loss
Morbid obesity :- is defined as being 100% over the ideal weight for height or having a body mass index
of greater than 45.
A number of surgical procedures but none is free of problems ,Selection of patients for operation
should ideally be made by a team that includes a nutritionist/endocrinologist and a psychiatrist, as well
as a surgeon
Indications of bariatric surgery
1-- obese patients that have a BMI of 35 kg/m or more with comorbidity,
2--those with a BMI of 40 kg/m or greater regardless of comorbidity,
3-- Candidates should have failure attempted weight loss in the past by medical supervised diet
regimens, exercise, or medications, but this is not mandatory.
4--They must be motivated to comply with postoperative dietary and exercise regimens and follow
up.
Contraindications
-- unfit to general anesthesia
-- unable to comply with postoperative lifestyle changes, diet,
-- unstable psychiatric illness, or inadequate ability to understand the consequences of surgery
Types of operations
the Stomach 2019-20
Dr. Muslim Kandel
19
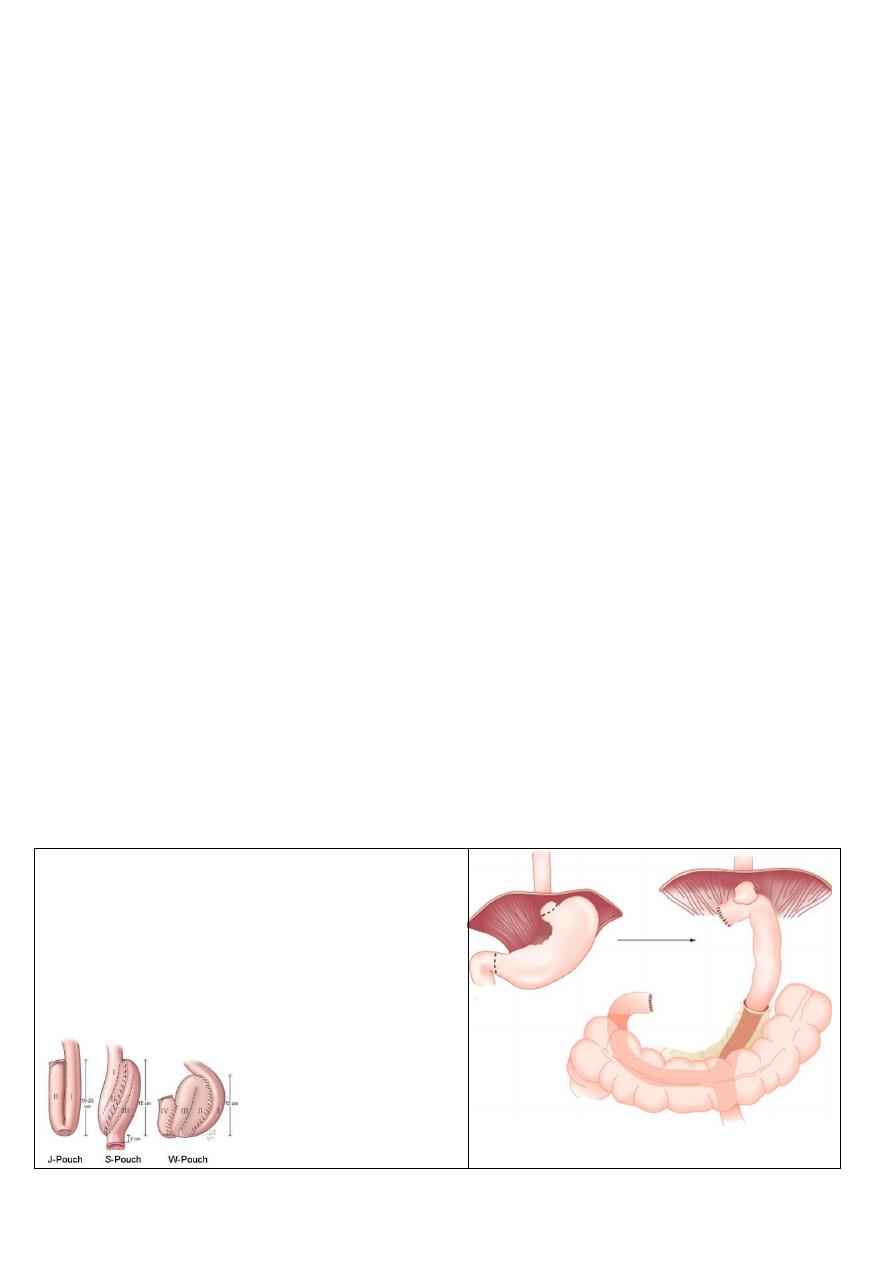
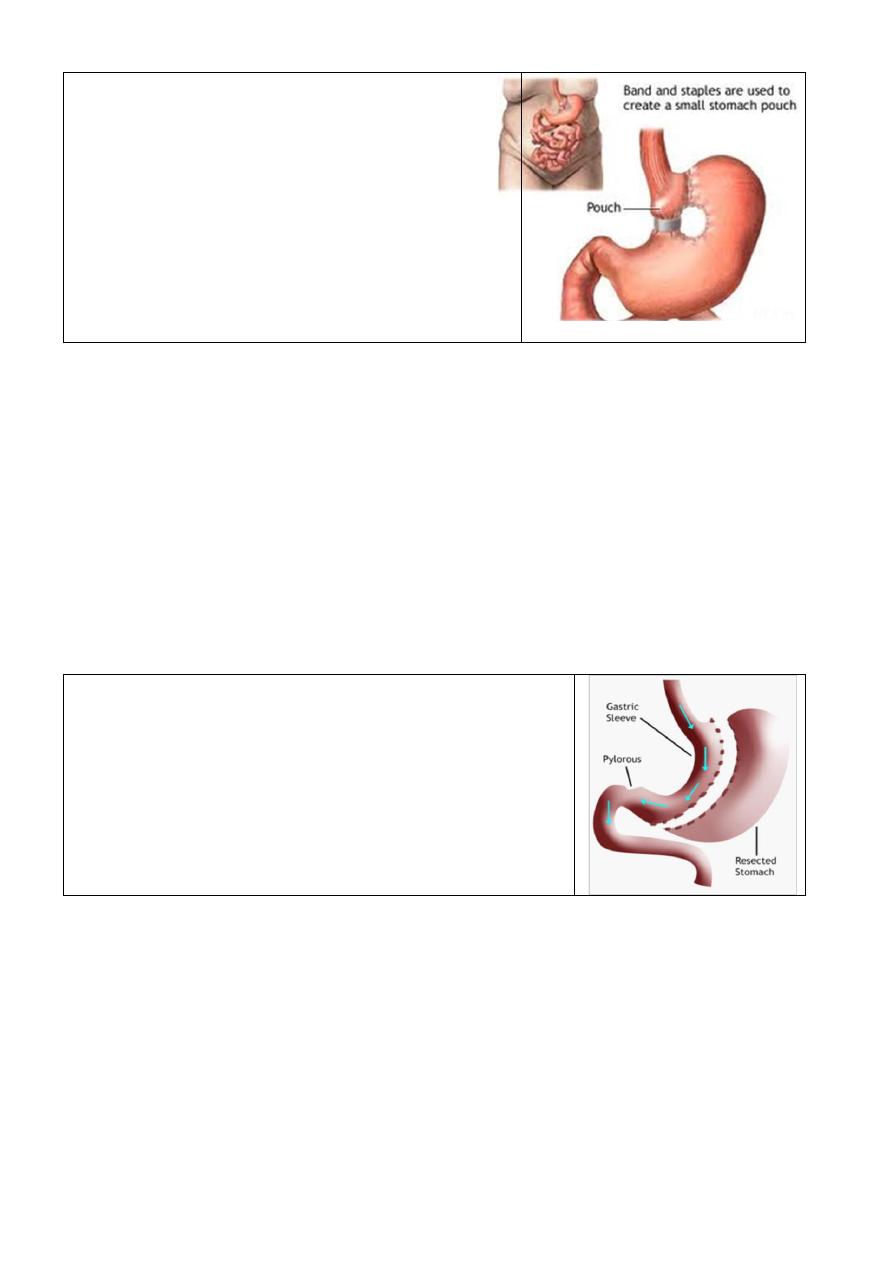
I--Restrictive operations restrict the amount of food intake
by reducing the quantity of food that can be consumed
(1)vertical banded gastroplasty (VBG )
The VBG is purely restrictive in nature. A proximal gastric
pouch empties through a calibrated stoma, which is
reinforced by a strip of mesh or a Silastic ring
(2)Laparoscopic Adjustable Gastric Banding (LAGB)
The patient is placed in reverse Trendelenburg position. Six
laparoscopic ports are placed. A 5-mm liver retractor is used
to elevate the left hepatic lob
II--Malabsorptive procedures limit the absorption of nutrients and calories from ingested food by
bypassing the duodenum and predetermined lengths of small intestine
1- Open Roux-en-Y Gastric Bypass (RYGB)
2-Laparoscopic Roux-en-Y Gastric Bypass (LRYGB)
3-Biliopancreatic Diversion (BPD)
4-small bowel bypass
Biliopancreatic Diversion(PBD)
Indications
-
--super obese, who have failed restrictive bariatric procedures,
-
-- patients wishing to have less restriction on their ability to eat after surgery but willing to
accept the consequences of increased bowel frequency and diarrhea
Pruceduer
A subtotal distal gastrectomy is performed, leaving a proximal 200-mL gastric pouch for the
superobese patient, or up to a 400-mL pouch for the others. The terminal ileum is measured, and the
intestine divided 250 cm proximal to the ileocecal valve
III-Sleeve gastrectomy :
the stomach is reduced to about 25% of its original size, by surgical
removal of a large portion of the stomach along the greater
curvature.
The result is a sleeve or tube like structure. The procedure
permanently reduces the size of the stomach, although there could
be some dilatation of the stomach later on in life.
The procedure is generally performed laparoscopically and is
irreversible
Complications
of operation
Pulmonary embolism is a risk for all such patients and hence they should be managed with adequate
doses of prophylaxis (5000 units of heparin tid).
wound herniation would be a common sequel of this operation
major metabolic consequences or liver disease.
patient non compliance,
stomal stenosis which may occur if the band is too tight or if fibrosis occurs in this region. The former
complication can be dealt with only by revisional surgery. Stomal stenosis can be treated endoscopically
by balloon dilatation, although very often this is unsuccessful in the long term
