Disorders of lipid metabolism
Most common disorders of lipid metabolism are associated with hyperlipidaemia. Very rare inherited disorders may be associated with accumulation of lipid in tissues and not in plasma. Hypercholesterolaemia is just one of the major risk factors of cardiovascular disease, others include smoking and hypertension.Investigations of lipid disorders
Plasma lipid concentration and lipoprotein pattern are labile and affected by eating , smocking, alcohol intake, stress and change in posture. It is essential that the samples are taken under standard conditions. The following points are important:-Ensure that the patient fasts overnight for around 12 h and is allowed only water to drink, if required. Although plasma cholesterol concentration is little affected by fasting, triglyceride concentrations rise and, and thus ideally fasting samples should be requested.
The patient should be on his or her usual diet for a couple of weeks preceding the test.
Plasma lipids should not be assessed in patients who are acutely ill, for example acute myocardial infarction, as plasma cholesterol concentration may be decreased due to the acute-phase response. Wait for about 3 months after the event, although if a sample is taken within 12 h of an event, a ‘true’ result may be obtained.
Unless treatment is being monitored, the patient must not be on any drugs designed to lower plasma lipid concentration.
Posture can alter plasma lipid concentrations: in the upright position, plasma cholesterol concentration can be 10 per cent higher than in the recumbent position.
The blood sample should not be heparinized and plasma and serum must be separated from cells as soon as possible.
Indications for measuring plasma lipids:-
Plasma total cholesterol and fasting TG concentration should be measured if there:-Clinical indication:-
Evidence of arterial disease in a relatively young individual.
Corneal arcus in a patient under about 40 years.
Tendinousxanthomata.
Is a family history of arterial disease.
Are risk factors for coronary artery disease such as, DM& hypertension.
-If the plasma total cholesterol concentration is greater than 275 mg/dl or if there are other risk factors for coronary artery disease, measure the plasma HDL-Chol. Concentration& LDL-Chol. Concentration.
Predominant hypercholesterolaemia:-
Hypercholesterolaemia associated with little or no elevation of plasma TG concentration is almost always due to raised plasma LDL concentration. The coexistence of an underlying genetic defect ,or the development of a disorder that affects plasma LDL concentration ,will cause greater increase in plasma cholesterol with age.
Secondary Hypercholesterolaemia:-
The commonest disorders that may produce a secondary increase in plasma tot l &LDL cholesterol concentration are:-primary hypothyroidism.
diabetes mellitus.
nephrotic syndrome.
cholestasis.
Drugs e.g. thiazide, loope diuretics(frusemide), β-blockers.
These disorders must be excluded in any individual presenting with hypercholesterolaemia.
Primary Hypercholesterolaemia :-
The familial incidence of hypercholesterolaemia often associated with an increased risk of ischemic heart disease, suggests an inherited disorder. In the following two disorders associated with moderate to severe hypercholesterolaemia, the pattern of inheritance is autosomal dominant.Familial combined hyperlipidaemia:-
The more common, is associated with excessive hepatic production of apo B & therefore of LDL, and of VLDL-triglyceride synthesis due to either a primary or secondary disorder.
Family members have a variety of different phenotypes:-
In one third there is an increase in plasma LDL-Chol. Concentration.
In another third there is an increase in both LDL-Chol.&VLDL-TG.
The remaining third have VLDL-hypertriglyceridaemia.
The lipid abnormalities only become apparent after the 3d decade and the risk of IHD in all cases is higher.
Familial(monogenic) hypercholesterolaemia:-
Is caused by a LDL receptor defect. There are several variants, all of which are inherited as autosomal dominant trait. The reduced cellular uptake of LDL, particularly by the liver, causes an increase in plasma total and LDL-Chol. Concentration .
Plasma TG concentration are either normal or only slightly raised. It is the most lethal of the inherited disorders. in conjunction with xanthomata Premature cardiovascular disease is often observed, along with premature corneal arci.
Predominant hypertriglyceridaemia:-
Elevated plasma TG concentration may be due to an increase in plasma VLDL or chylomicrons or both. Hypertriglyceridaemia is usually secondary to another disorder.-Causes of secondary hypertriglyceridaemia:-
1. Obesity & excessive carbohydrate intake.
2. Alcohol.
3. Diabetes mellitus.
4.Primary hypothyroidism
5. Nephrotic syndrome.
6. Renal glomerular dysfunction.
7. Drugs: Pills&oestrogen,β-blockers, thiazide diuretics.
8. Acute pancreatitis.
Primary hypertriglyceridaemia is less common than primary hyper-cholesterolaemia.
Hyperchylomicronaemia:-
Is usually due either to an acquired or inherited deficiency of lipoprotein lipase. Insulin is needed for optimal enzyme activity. Consequently, Hyper-chylomicronaemia may occur in poorly controlled diabetic patients. It may also be found in those presenting with acute pancreatitis.
-Inherited lipoprotein lipase deficiency may be due to:-
True deficiency of the enzyme.
Reduced activity of the enzyme because of apo C-II deficiency.
The plasma is very turbid because of the accumulation of chylomicrons.
Mixed Hyperlipidaemia:-
Raised plasma concentration of both cholesterol and TG are commonest in patients with poorly controlled diabetes mellitus, severe hypothyroidism or the nephrotic syndrome.The commonest primary cause is familial combined hyperlipidaemia with elevated plasma LDL&VLDL concentration.
Less commonly, mixed hyperlipidaemia may be caused by the accumulation of IDL &chylomicron remnant, which contain both cholesterol and TG.
Fatty liver:-
For a variety of reasons, lipid mainly as triacylglycerol can accumulate in the liver. Extensive accumulation is regarded as a pathologic condition. When accumulation in the liver becomes chronic, fibrotic changes occur in the cells that progress to cirrhosis and impaired liver function. Fatty liver of two types:-1.Associated with raised level of plasma free fatty acid:-
Resulting from mobilization of fat from adipose tissue or from the hydrolysis of lipoprotein triacylycerol by lipoprotein lipase in extrahepatic tissues.
This occurs during starvation and the feeding of high fat diet . the ability to secrete VLDL may also be impaired (e.g. starvation).
2.The second type is usually due to a metabolic block in the production of plasma lipoproteins, thus allowing triacylglycerol to accumulate.
Alcoholism:-
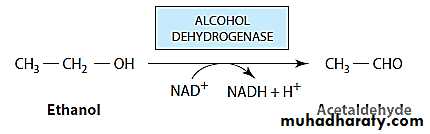
Leads to fat accumulation in the liver, hyperlipidaemia, and ultimately cirrhosis. The exact mechanism of action of ethanol in the long term is still uncertain.Ethanol consumption over a long period leads to accumulation of fatty acids in the liver that are derived from endogenous synthesis rather than from increased mobilization from adipose tissue. Oxidation of ethanol by alcohol dehydrogenase leads to excess production of NADH.
The NADH generated competes with reducing equivalents from other substrates, including fatty acids, for the respiratory chain, inhibiting their oxidation, and decreasing activity of the citric acid cycle. The net effect of inhibiting fatty acid oxidation is to cause increased esterification of fatty acids in triacylglycerol, resulting in the fatty liver.
Oxidation of ethanol leads to the formation of acetaldehyde, which is oxidized by aldehyde dehydrogenase, producing acetate. Other effects of ethanol may include increased lipogenesis & cholesterol synthesis from acetyl-CA, and lipid peroxidation.