Platelets (thrombocytes - "clotting")
The platelets are small, granulated bodies that aggregate at sites of vascular injury.
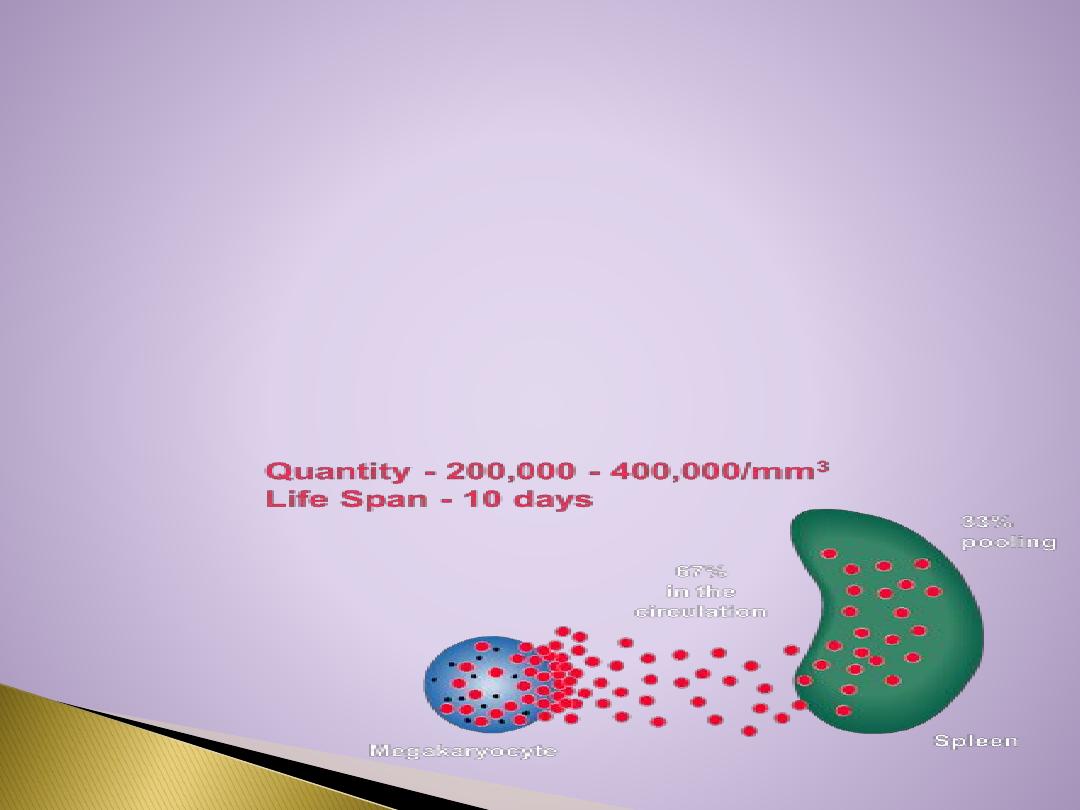
They lack nuclei and are 2-4 um in diameter . There are about( 150,000-
300,000/uL) of circulating blood, and they normally have a half-life of about 10
days.( 8-12 days).
The
megakaryocyte
s, giant cells in the bone marrow, form platelets by pinching off
bits of cytoplasm and extruding them into the circulation. Between 60% and 75% of
the platelets that have been extruded from the bone marrow are in the circulating
blood, and the remainder are mostly in the spleen(1\3).
Splenectomy causes an increase in the platelet count (thrombocytosis).
In their
cytoplasm
are
(1) actin and myosin molecules, which are contractile proteins, thrombosthenin, that
can cause the platelets to contract
(2) residuals of both the endoplasmic reticulum and the Golgi apparatus that synthesize
various enzymes and especially store large quantities of calcium ions
(3) mitochondria and enzyme systems that are capable of forming (ATP) and
adenosine diphosphate (ADP)
(4) enzyme systems that synthesize prostaglandins, which are local hormones that
cause many vascular and other local tissue reactions
(5) an important protein called fibrin-stabilizing factor
(6) a growth factor that causes vascular endothelial cells, vascular smooth muscle
cells, and fibroblasts to multiply and grow, thus causing cellular growth that eventually
helps repair damaged vascular walls.
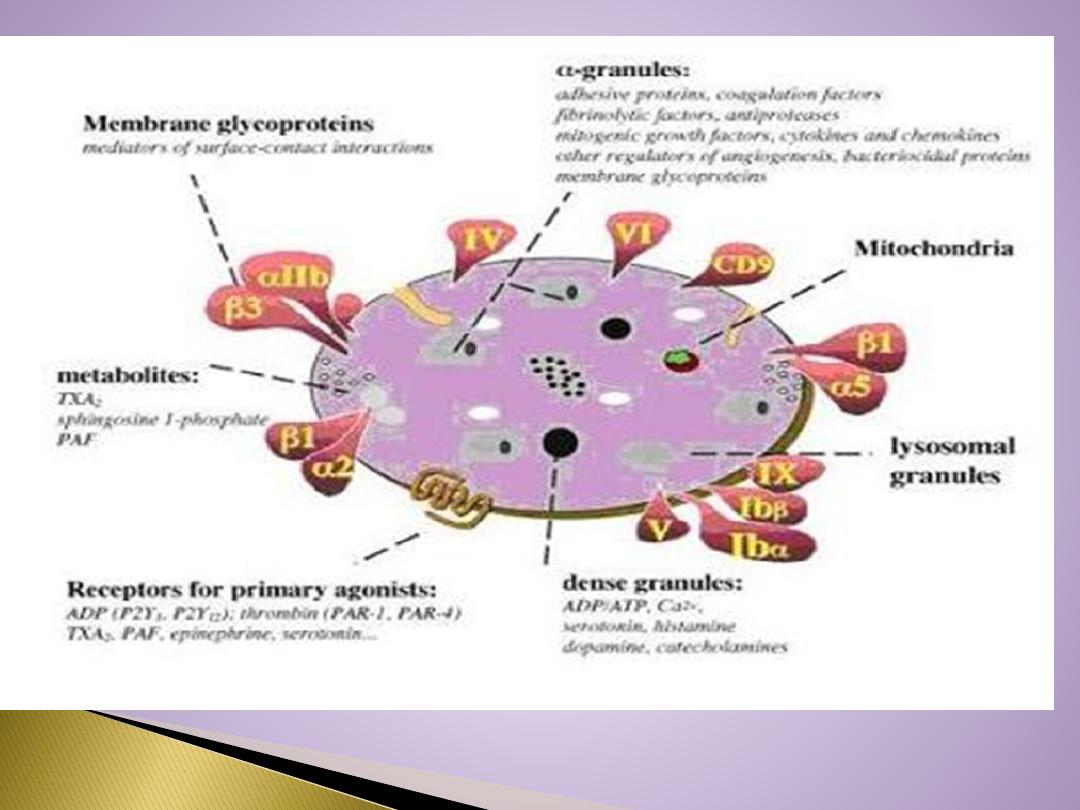
Their
membranes
contain receptors for collagen, ADP, vessel wall von
Willebrand factor . and fibrinogen. Their cytoplasm contains actin,
myosin, glycogen, lysosomes, and two types of granules:
Platelet Granules :
**
Alpha granules
contain:
1.
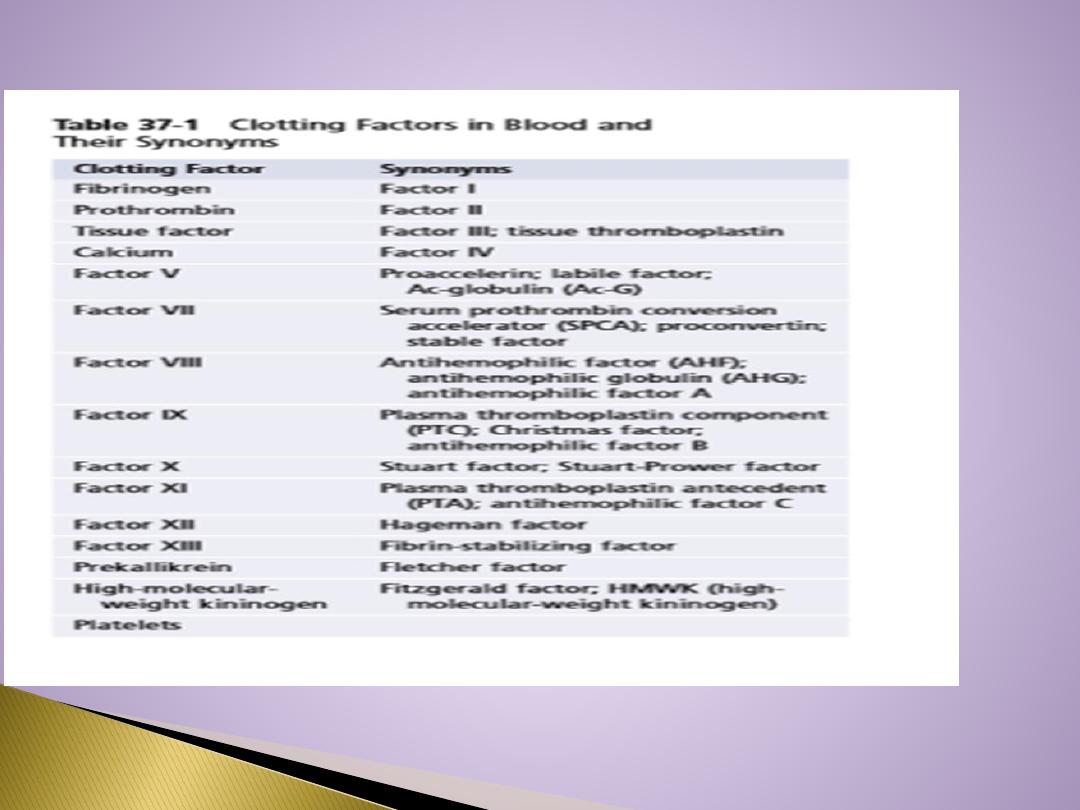
Clotting factors –
fibrinogen
, V and XIII
2.
2. Platelet-derived growth factor PDGF
3.
3. Vascular endothelial growth factor (VEGF)
4.
4. Basic fibroblast growth factor (FGF)
5.
5. Endostatin
6.
6. Thrombospondin.
**
Dense granules
contain:
Adenine
1. Nucleotides “ADP “
2. Serotonin
3. Phospholipid
4. Calcium
5. Lysosomes.
150,000 to 300,000 per microliter
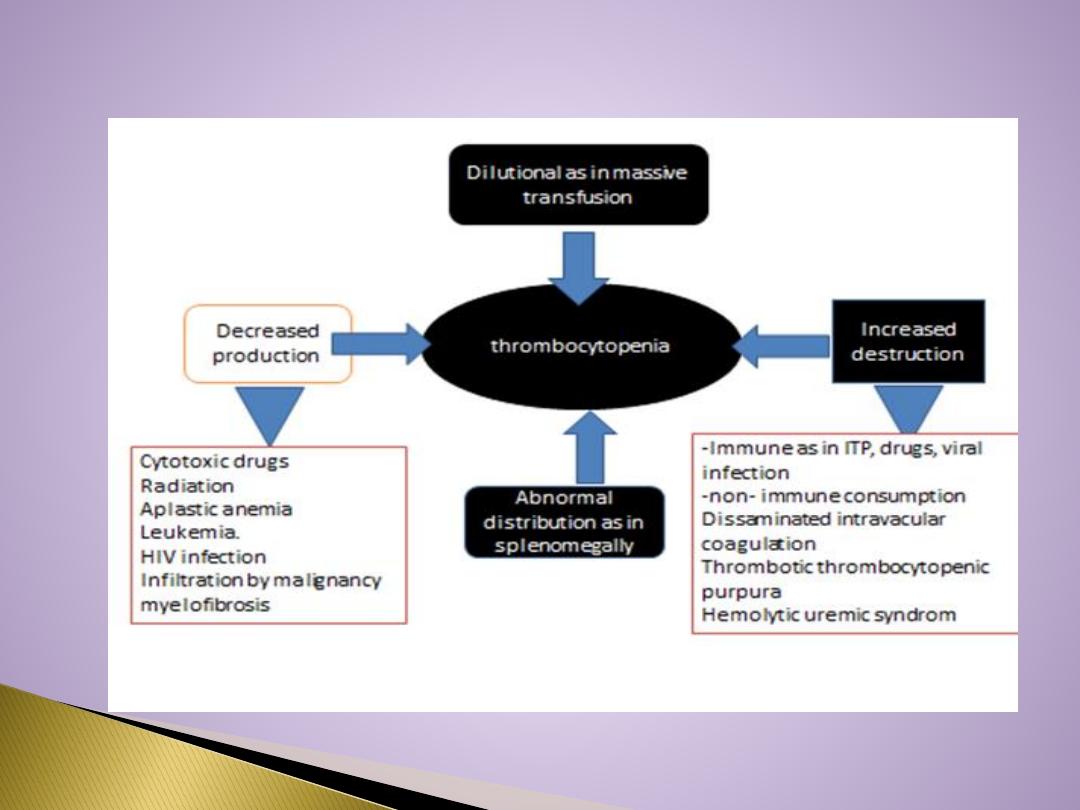
Thrombocytopenia:
abnormally low platelet count
Thrombocytosis:
abnormally high platelet count
Low count due to :
Decreased Production
Decreased Survival – Immune (ITP) immune thrombocytopenia
Increased utilization – DIC disseminated intravascular coagulopathy
Defective Platelet function:
Acquired – Drugs – Aspirin, MDS Myelodysplastic syndrome
Congenital – Eg. Thrombasthenia.
Thrombocytopenic purpura
When the platelet count is low, clot retraction is deficient and there is poor
constriction of ruptured vessels. The resulting clinical syndrome
(thrombocytopenic purpura) is characterized by easy bruisability and multiple
subcutaneous hemorrhages. Purpura may also occur when the platelet count is
normal & in state of , the circulating platelets are abnormal (thrombasthenic
purpura). Individuals with thrombocytosis (increased number of platelets) are
predisposed to thrombotic events.
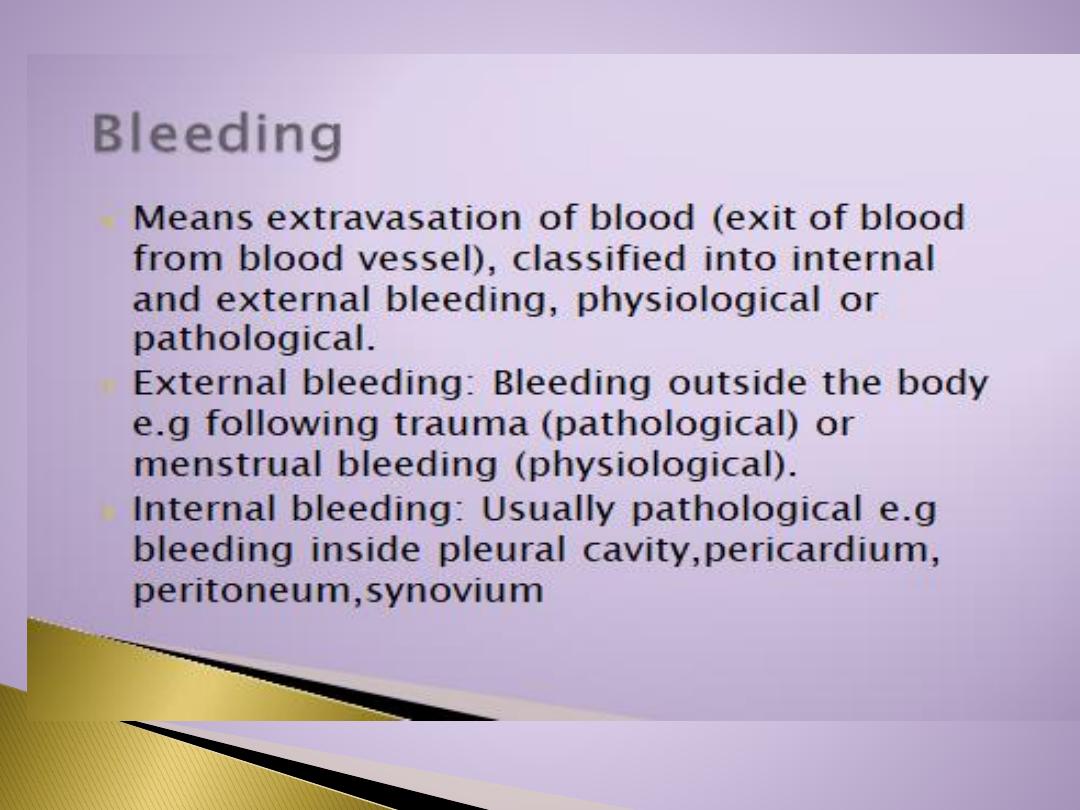
Petechiae
Tiny red spots resulting from blood
extravasated from normally healthy blood vessels which have
become abnormally permeable (due to a vascular or platelet
disorder)
Epistaxis "Nose bleeding"
This is usually caused by a
mild trauma to the blood vessels of the anterior nares, but
occasionally is a manifestation of a platelet or vascular
abnormality
Ecchymosis
An area of extravasated blood arising from
trauma to the blood vessels of that area. This can also arise in
patients with vascular or platelet disorders
.

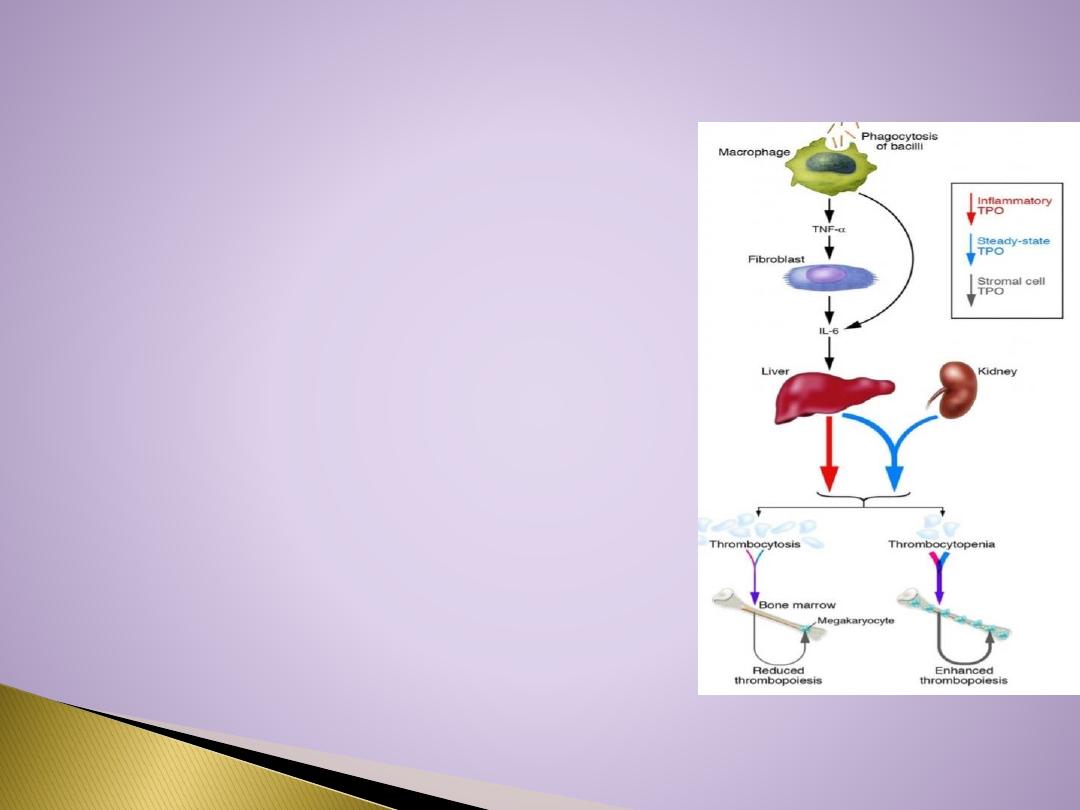
Platelet production is regulated by
(Thrombopioesis
):
1. colony- stimulating factors that control the production of megakaryocytes.
2. Thrombopoietin, a circulating protein
factor which facilitates megakaryocyte
maturation.(TPO)
From the pluripotent stem cells in the bone marrow.
CFU-M “Colony forming megakaryocyte”
Megakaryo
blast
→→
Pro
megakaryo
cty
e
→Megakaryocytes →Platelets
Platelets are eliminated from the circulation
mainly by the tissue macrophage system in the
spleen( splenomegaly reduced the platelet count).

Hemostasis
means prevention of blood loss( stoppage of
blood flow after damage) .
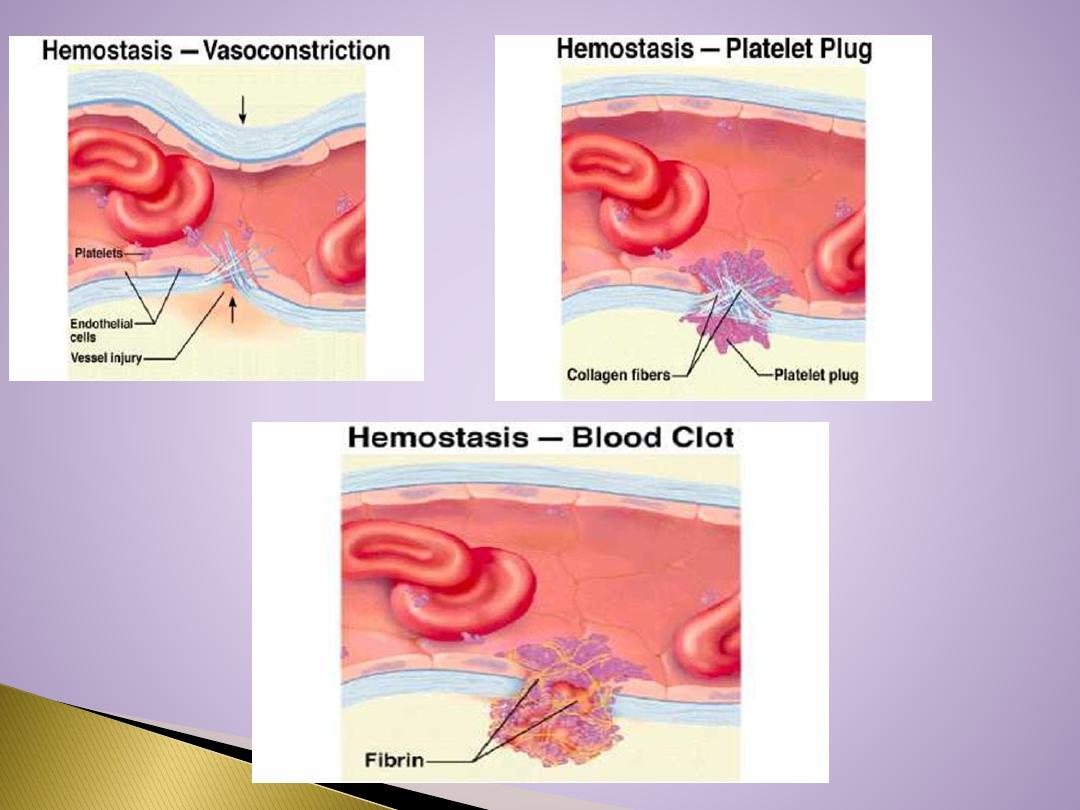
Whenever a vessel is severed or ruptured, hemostasis is
achieved by several mechanisms:
(1) vascular constriction
(2) formation of a platelet plug
(3) formation of a blood clot as a result of blood coagulation
(4) eventual growth of fibrous tissue into the blood clot to
close the hole in the vessel permanently
In ruptured blood vessel
1
. Pain impulses from the site of trauma as well as from the
surrounding nervous tissue originate and reach the spinal cord.
From the spinal cord order signal arise.
The order signals pass through the sympathetic nerves
Lead to spasm of the vessel.
2
. Local muscle also contribute to the vascular vasospasm.
3
. local autacoid factors from the traumatized tissues and blood
platelets.
**Vasoconstriction resulting from local myogenic contraction of
the blood vessels is initiated by direct damage to the vascular
wall.In the smaller vessels, the platelets are responsible for
much of the vasoconstriction by releasing a
vasoconstrictor
substance,
thromboxane A2.
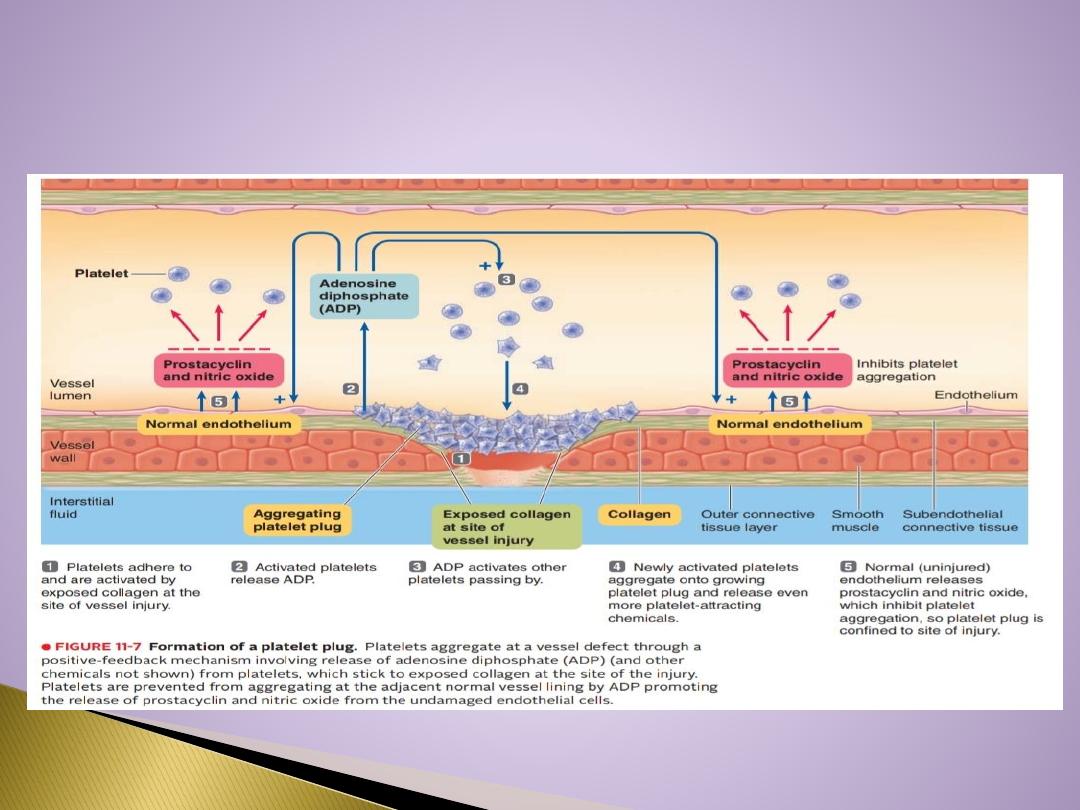

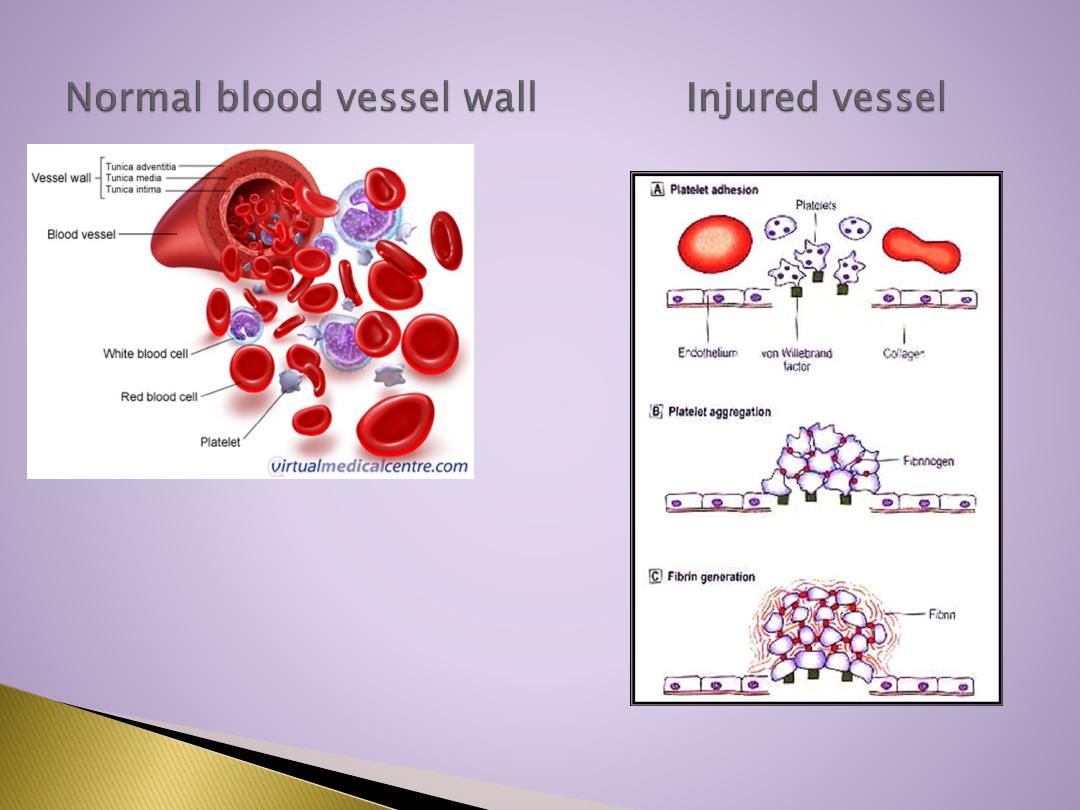
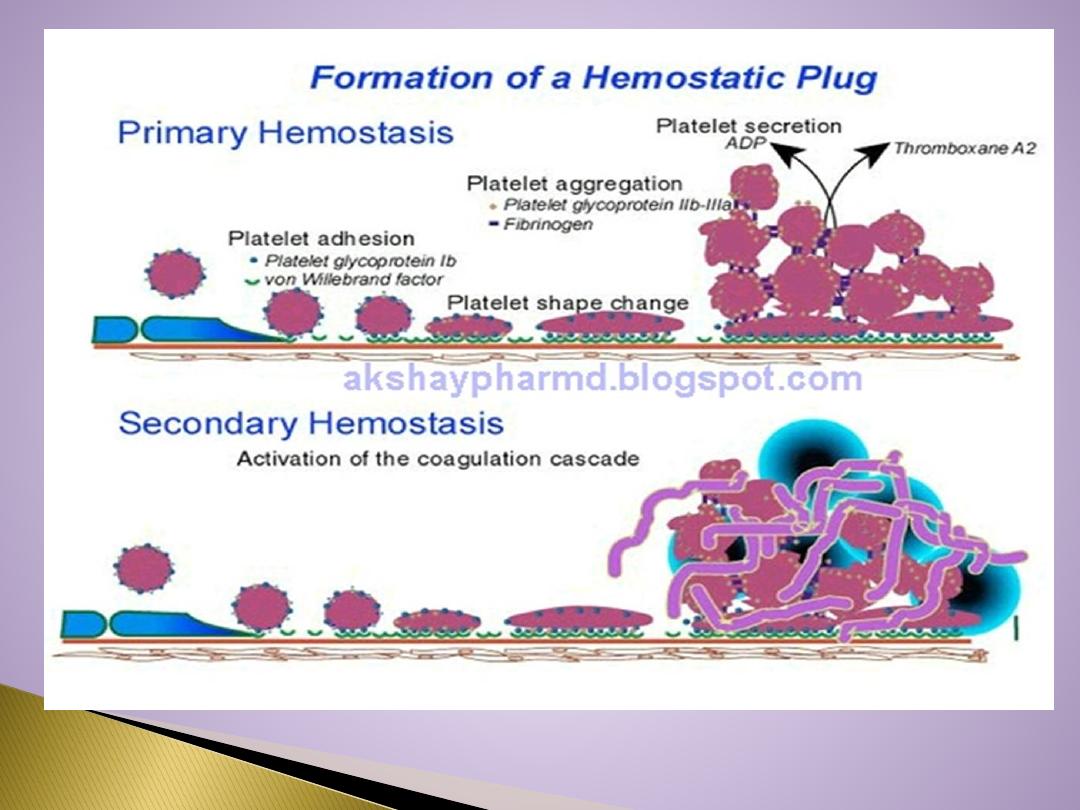
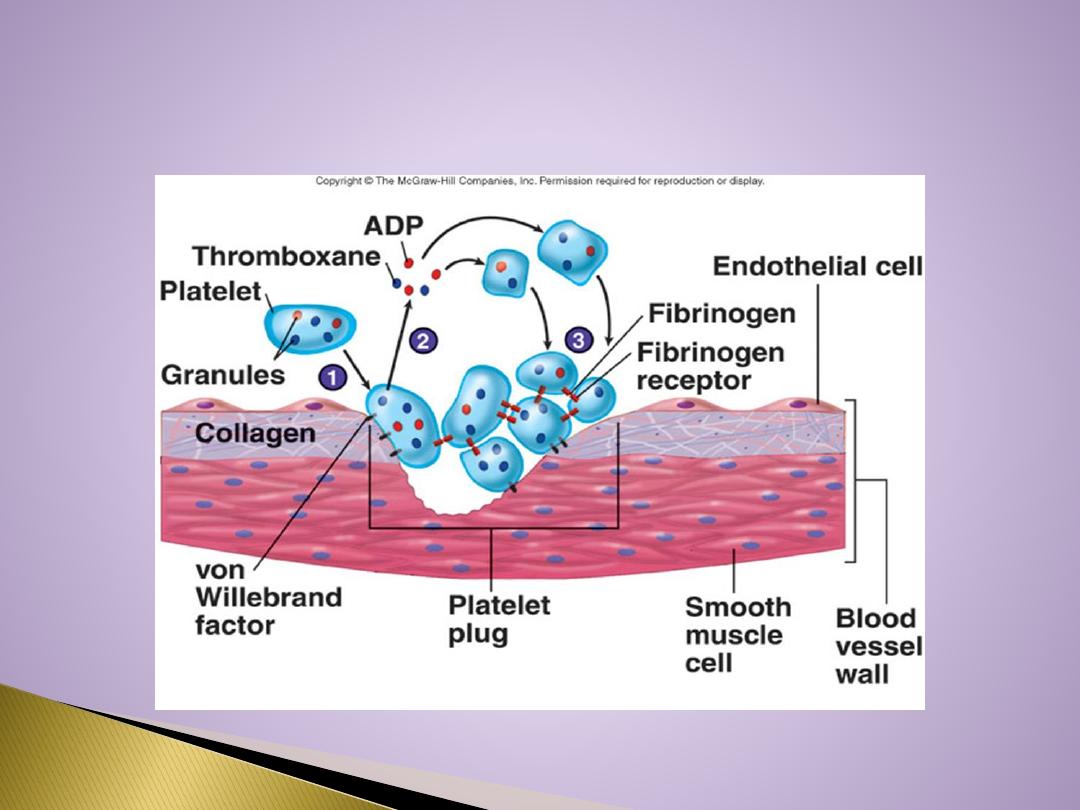
When platelets come in contact with a damaged vascular surface, platelets
attach to the exposed collagen fibers in the vascular wall.
Platelets immediately change their own characteristics.
Platelets begin to swell and assume irregular forms with numerous irradiating
pseudopods protruding from their surfaces.
Contractile proteins in the platelets contract forcefully and cause the release
of granules that contain multiple active factors ,
Adenosine diphosphate (ADP)
is released which causes surface of nearby circulating platelets to become
sticky and it adheres to the
first layer of aggregated platelets
The aggregated platelets adhere to the
von Willebrand factor
that leaks into
the traumatized tissue from the plasma
It leads to the release of more ADP , which cause more platelets to pile up at
the injured site. The aggregating process is reinforced by the formation of
Thromboxane A2. It directly promotes platelet aggregation and further
enhances it indirectly by triggering the release of even more ADP from the
platelet granules, then Formation of platelet plug takes place.

The
aggregated platelet plug
not only physically seal the break in the vessel
but, also perform
three
other important roles:
1.
Actin and myosin which were the contractile proteins in the platelets
contract , This compacts and strengthens the plug which was initially, a loose
plug.
2.
Various chemicals released from the platelet plug include several
vasoconstrictors (serotonin, epinephrine and Thromboxane A2 ) cause vascular
vasospasm
3.
The platelet plug release other chemical substances that play a role in blood
clotting.
Platelet plugging mechanism alone is sufficient to seal tears in the capillaries
and small vessels but, large holes require formation of blood clot to stop
bleeding.
**Normal endothelium of the vessel release
Prostacyclin
which prevents
platelet aggregation. So, platelet
plug is limited to the defected
part of the
vessel and does not spread to the normal vascular tissue.
Blood clot in ruptured vessels
If there is a large defect in the vessel then blood clot + platelet plug are
required to stop bleeding. As clot on the top of platelet plug , supports
it and reinforces the seal over the break in the vessel.
Onset Of Formation Of Blood Clot:
15 – 20 sec…… in severe trauma.
1 – 2 min…… in minor trauma.
Ultimate step in clot formation is the
conversion of fibrinogen
which is
a (soluble protein that is produced by the liver and is normally always
present in the plasma)
to fibrin
which is( insoluble thread like molecule).
Fibrinogen ( thrombin) Fibrin
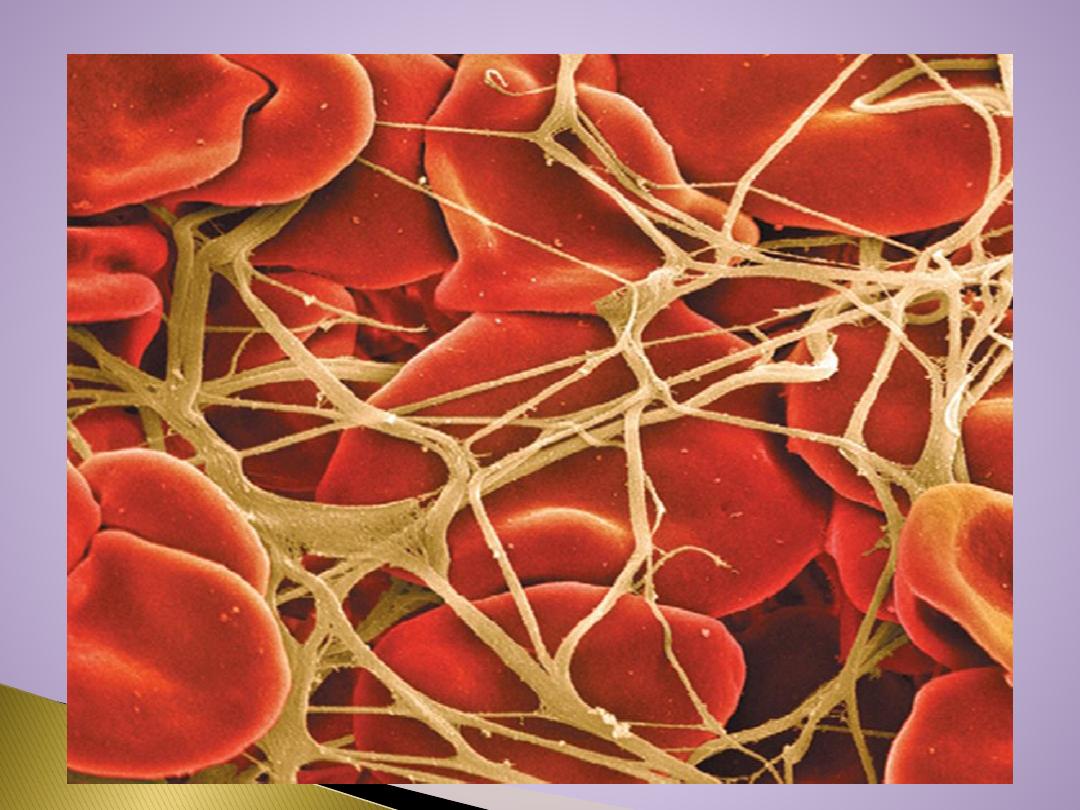
Fibrin molecules adhere to the damaged vessel surface
forming a loose netlike meshwork that traps the cellular
elements of blood. The clot appears red because of
abundance of RBC that are trapped in it.
The original fibrin web is weak because the fibrin threads are
loosely interlaced, then various chemical linkages are formed
between adjacent strands to strengthen and stabilize the clot
mesh work.
The cross linkage process which is catalyzed by a clotting
factor known as
factor XIII (Fibrin stabilizing factor).

Fibrous organization or Dissolution of blood clot
Once a blood clot has formed, it can follow one of two courses:
It can become invaded by fibroblasts, which subsequently form connective
tissue all through the clot.
It can dissolve
The usual course for a clot that forms in a small hole of a vessel wall is
invasion by fibroblasts, beginning within a few hours after the clot is
formed. This event is promoted by growth factor secreted by platelets.
Complete organization of the clot into fibrous tissue takes place within 1 to
2 weeks.

Thank you
