atherosclerosis
1
At the End of This Lecture You
should Be Able to
• Appreciate the significance of atherosclerosis
as the major cause of death worldwide
• Describe the gross and microscopic
morphology of atherosclerotic plaques
• Appreciate the significance of plaque
morphology in determining its future behavior
• Understand the risk factors and causes of
atherosclerosis
2
• How would atherosclerosis present you
• How to estimate the likelihood of developing
atherosclerosis
• How to prevent atherosclerosis
• How to treat atherosclerosis
3
Athereosclerosis
• The major cause of morbidity & mortality
worldwide
• Progressive inflammatory disorder of the
arterial wall
• Focal deposition of lipid-rich material
• Initially clinically silent
4
Athereosclerosis
• Later on: they become large enough to obstruct
the lumen of the blood vessel
• Endothelial ulceration leads to acute
thrombosis
• Embolization of lipid material leads to distal
arterial occlusion
5
Manifestations of atherosclerosis
• Largely clinically silent
• Coronary artery disease: angina pectoris,
myocardial infarction, arrhythmias, sudden
death, etc.
• Cerebrovascular disease: stroke, TIA
• Peripheral vascular diseae.
• Renal artery stenosis
• Often these manifestations co-exist
6
PATHOGENESIS
Normal endothelial function
• The blood vessel wall is not a simple tubing
system that merely transports blood
• Rather, the endothelial lining of the blood
vessels is the largest endocrine system in the
body
7
Normal Endothelial Function
• Normal function is to maintain blood in a fluid
state
• When the endothelial function is impaired, it
starts to release factors that enhance
inflammation and platelet-fibrin activation
8
Normal endothelial Function
Factors normally released by the endothelium
include:
• Prostacyclin (PG I2)
• Nitric oxide
• Tissue plasminogen activator (t-PA)
9
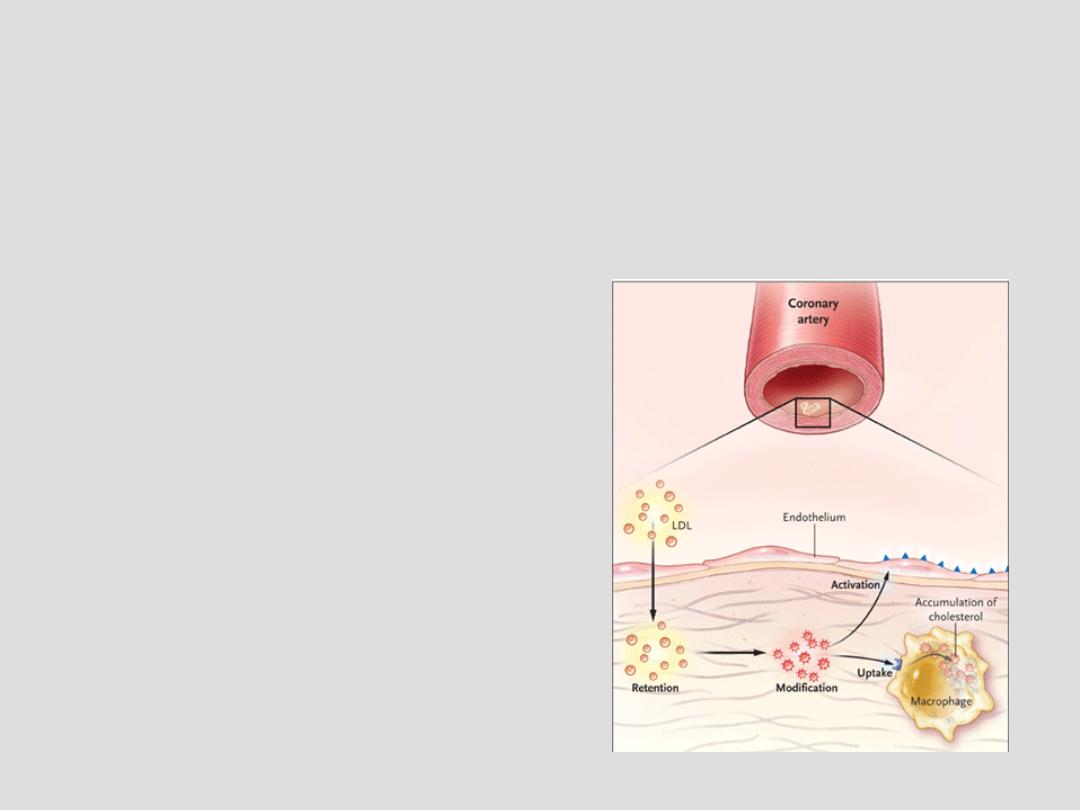
In Atherosclerosis
• In patients with hypercholesterolemia, LDL
infiltrates the artery and
is retained in the intima
10
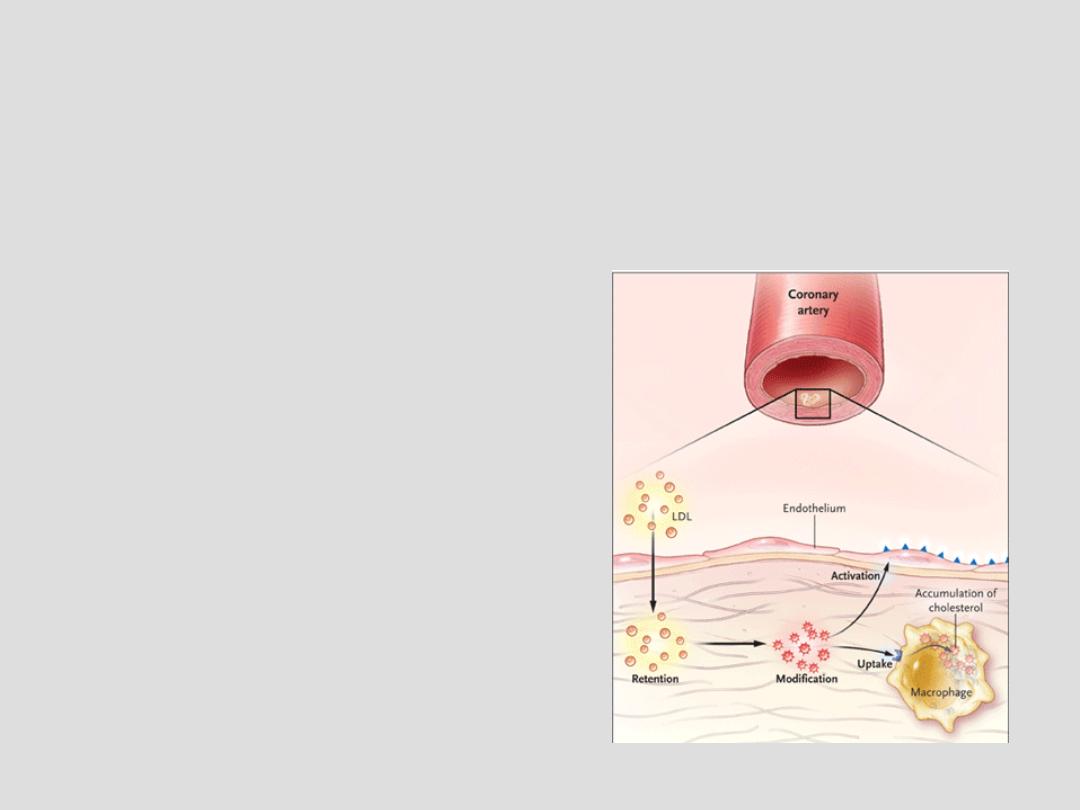
In Atherosclerosis
• LDL undergoes oxidative and
enzymatic modifications
(oxidized LDL)
11
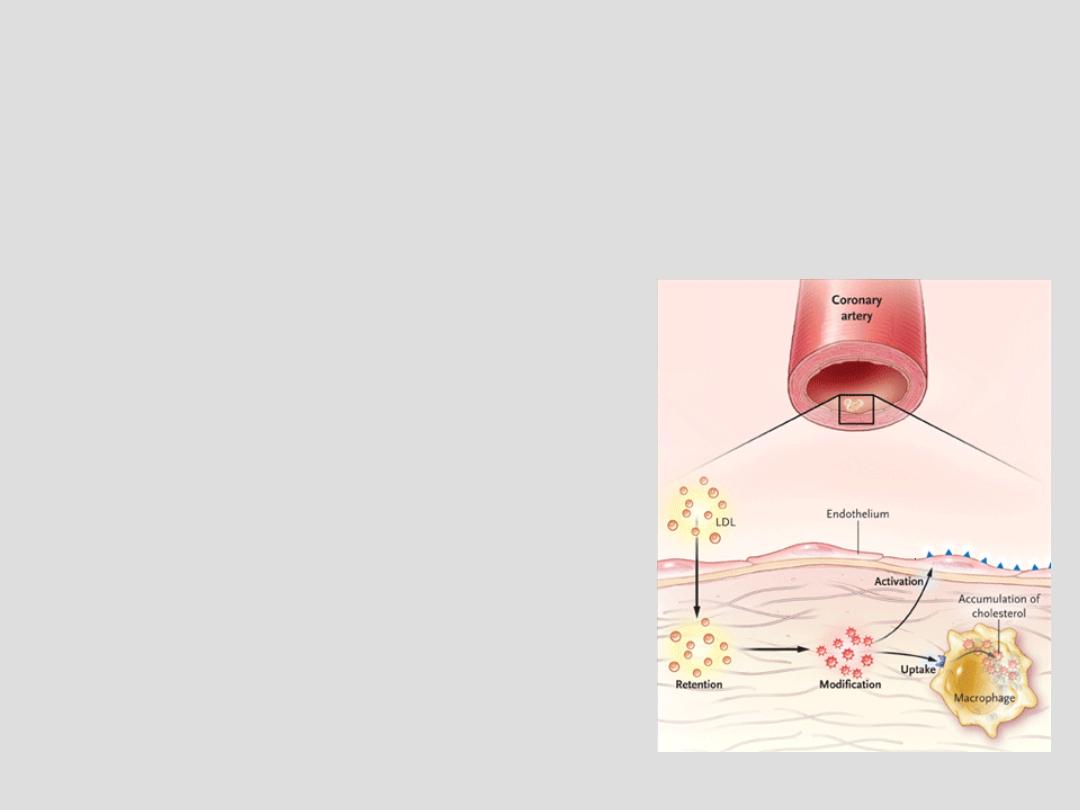
In Atherosclerosis
• Oxidized LDL stimulates the endothelium to
release adhesion molecules:
– Thromboxane A2
– Endothelin
– Plasminogen activator
inhibitor (PAI-1)
12
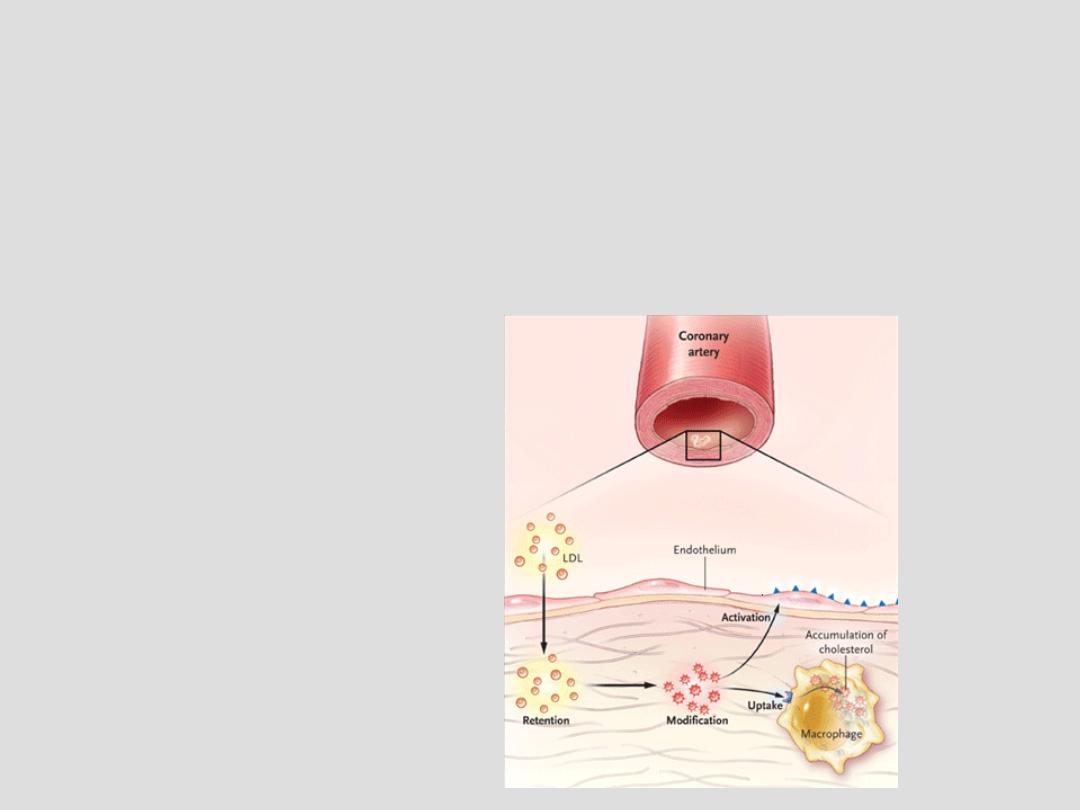
In Atherosclerosis
• Monocytes are recruited through the activated
endothelium to differentiate into macrophages
13
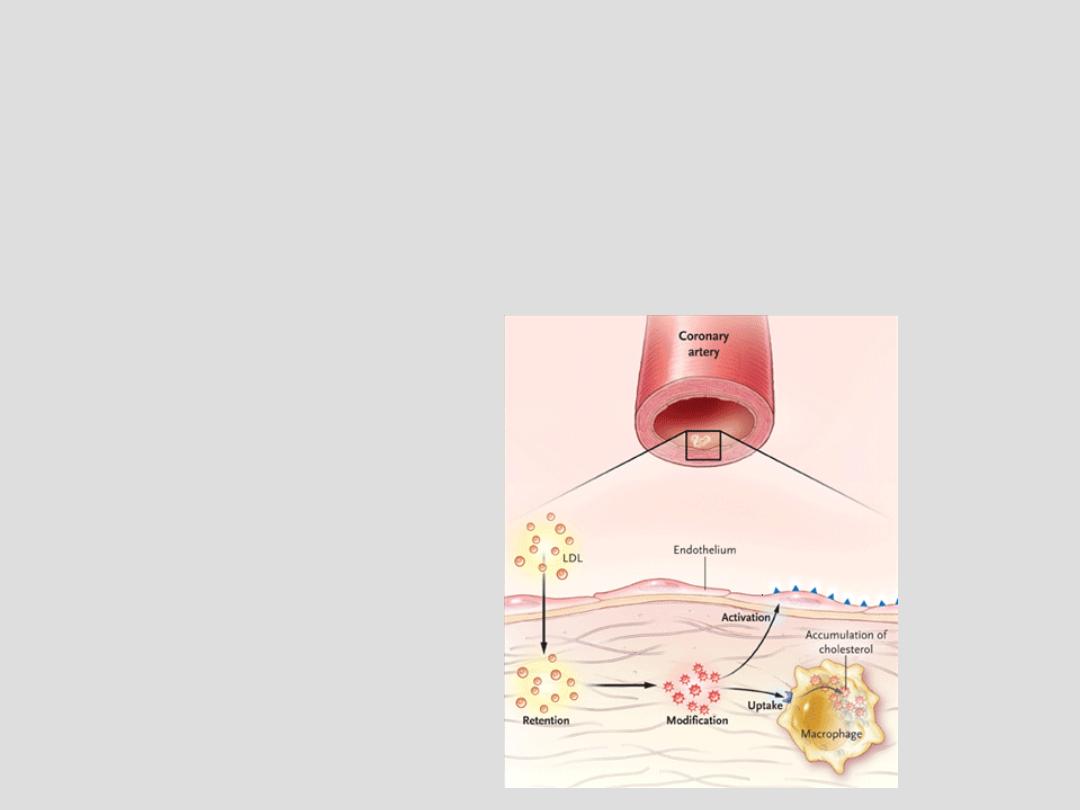
Pathogenesis of atherosclerosis
• The recruited macrophages engulf the oxidized
LDL to become foam cells
14
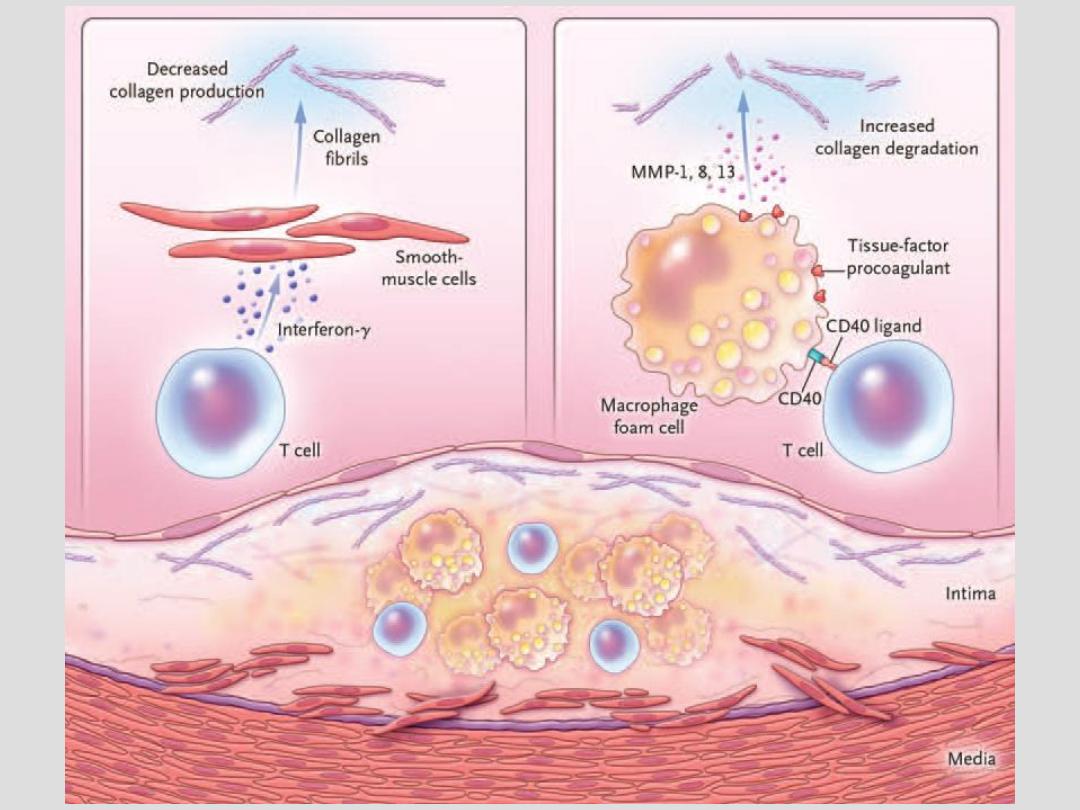
Pathogenesis of atherosclerosis
• Also, the recruited macrophages release
cytokines which promote inflammation
including:
– Interlukin 1(IL-1)
– Tumor necrosis factor (TNF)
– Interferon γ
– Matrix metalloproteinase
15
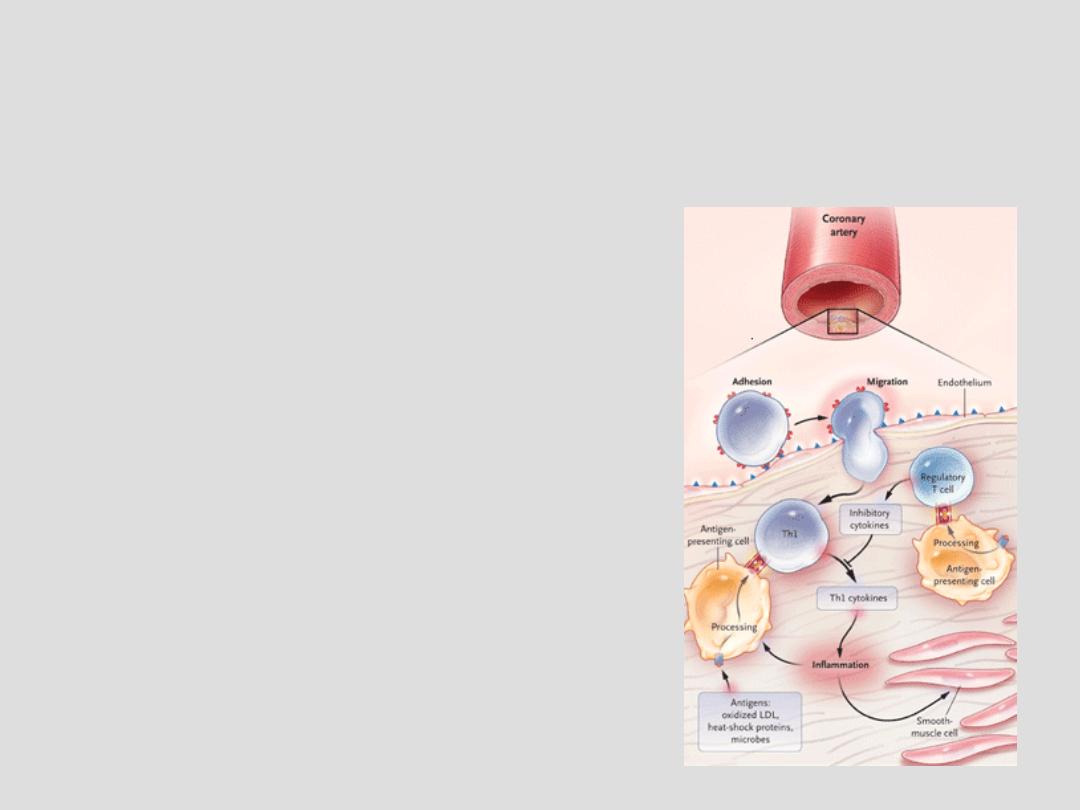
Pathogenesis of atherosclerosis
Cytokines released from
macrophages and lymphocytes
lead to recruitment of
smooth muscle cells
from the media
16
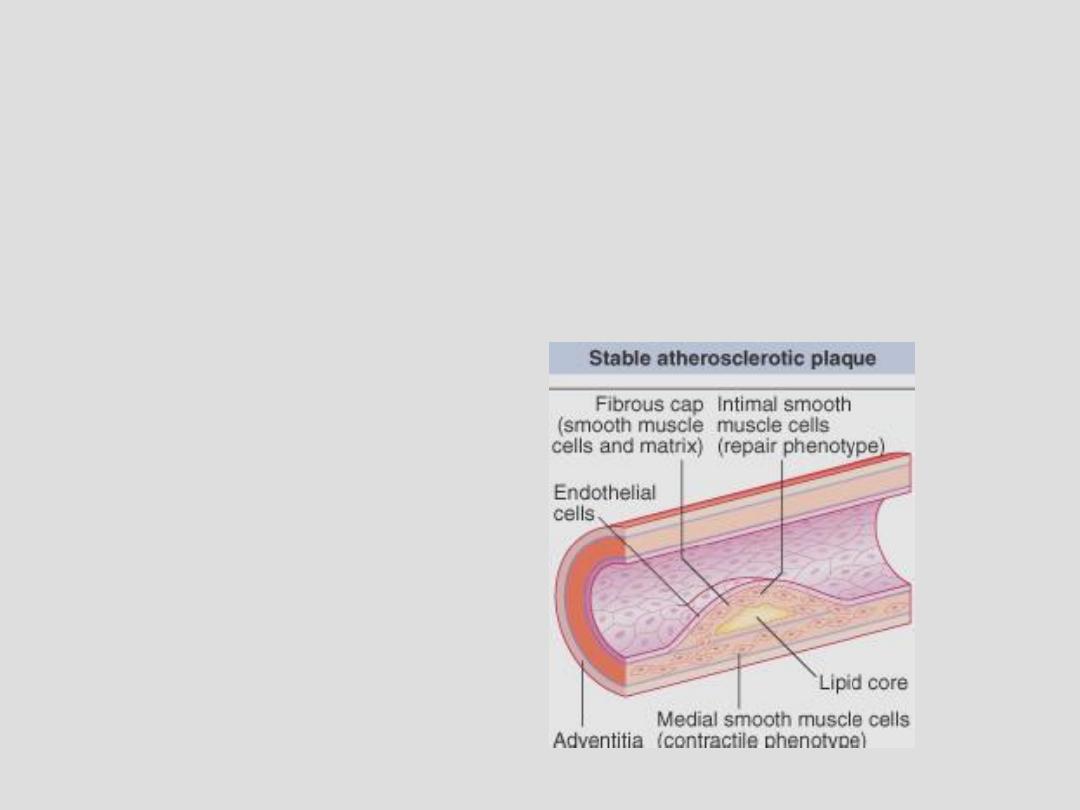
Pathogenesis of atherosclerosis
• These smooth muscle cells no longer function
as contractile cells but as repair cells
17
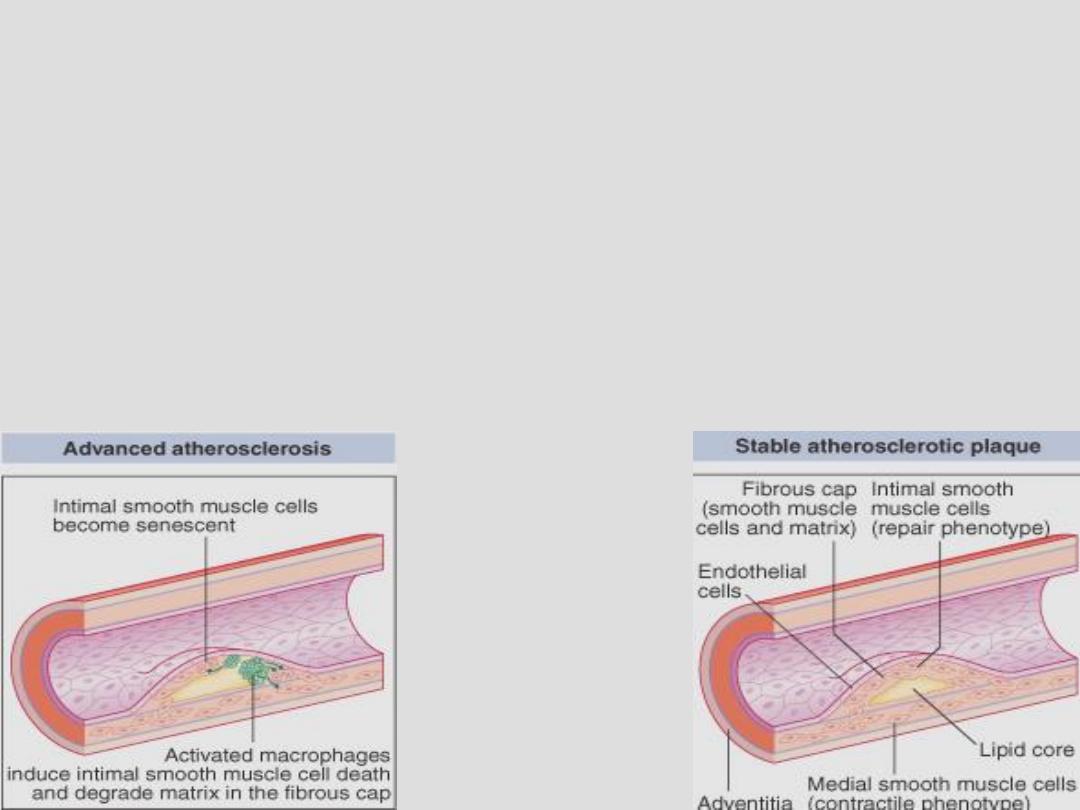
Pathogenesis of atherosclerosis
• The end result of an atherosclertic plaque
depends on the destructive effect of
macrophages and the reparative role of smooth
muscle cells
18
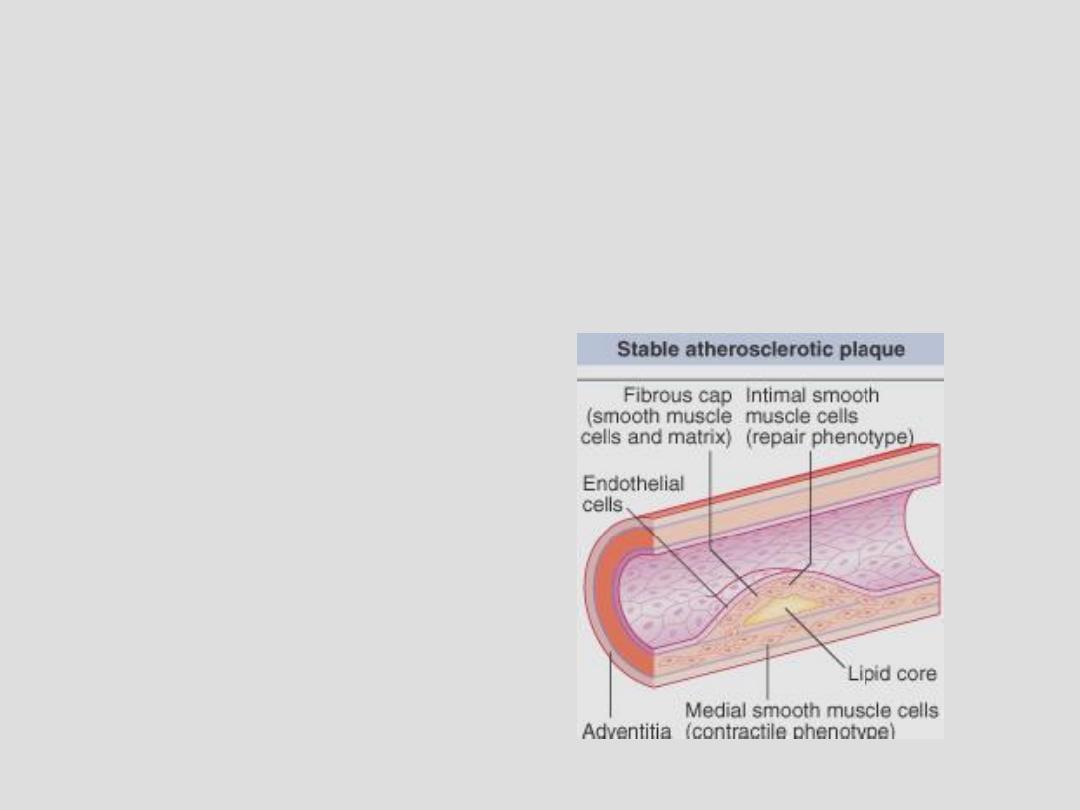
Pathogenesis of atherosclerosis
• A stable plaque contains small lipid core and
dense cap composed of smooth muscles and
collagen
19
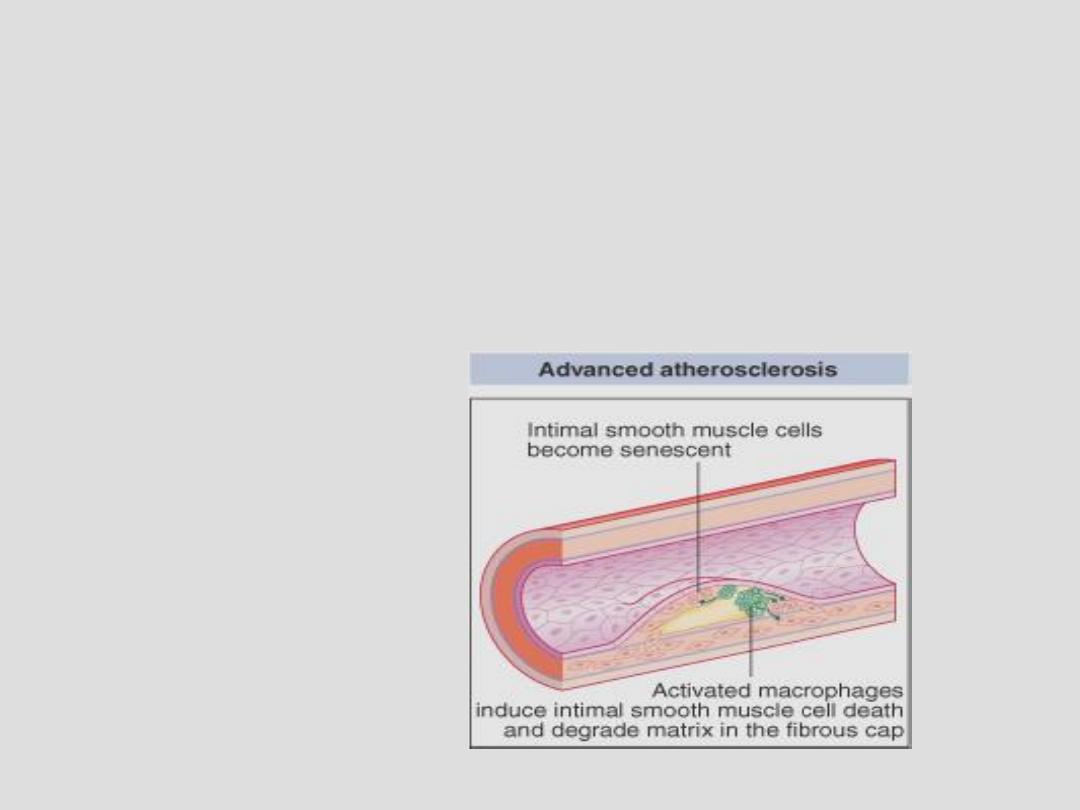
Pathogenesis of atherosclerosis
• An unstable plaque has a thin fibrous cap
which can be digested by enzymes released by
macrophages.
20
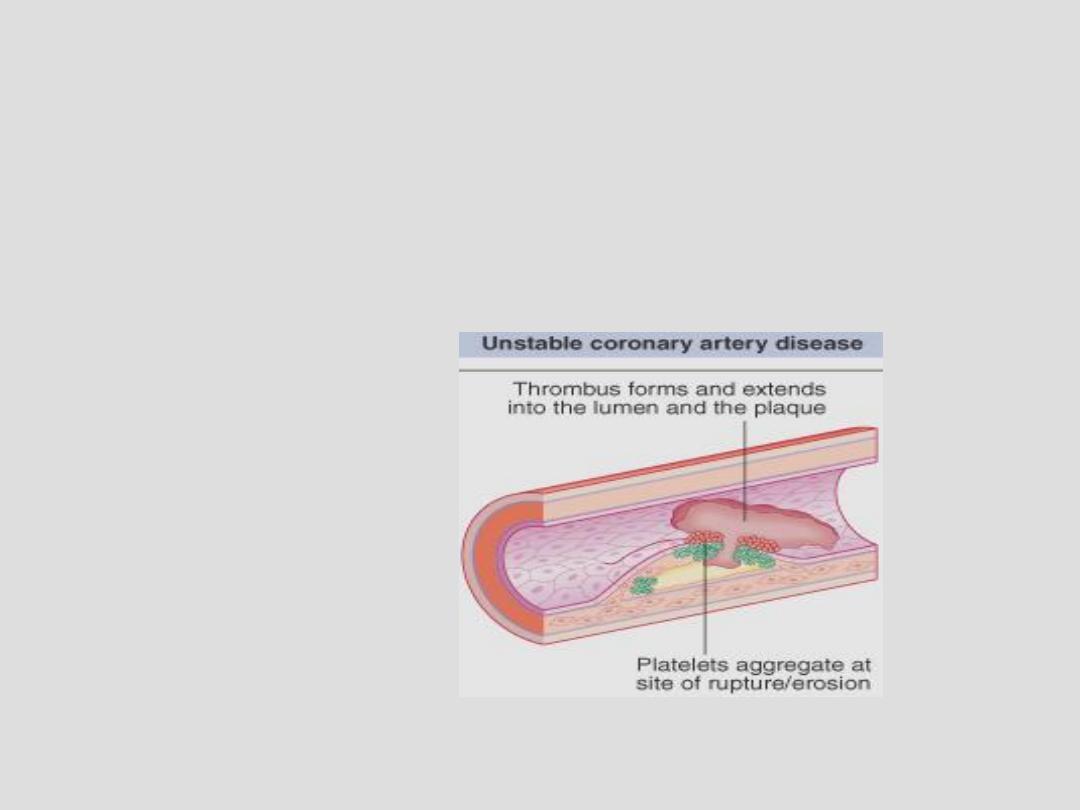
Pathogenesis of atherosclerosis
• Exposure of the subendothelial tissue to the
flowing blood leads to thrombosis and vessel
occlusion
21
22
23
Pathogenesis of atherosclerosis
• The pathological effects of the plaque do not
depend only on its size but also on the relative
constituents of the plaque:
• A plaque with thin fibrous cap may rupture &
cause sudden occlusion of the artery by
superimposed thrombosis even if it was of
small volume
24
Risk Factors for Atherosclerosis
• The effects of risk factors are multiplicative,
not additive
25
Risk Factors for Atherosclerosis
• Hereditary (genetic) factor: multifactorial
(polygenic) inheritance:
• Age and gender:
– Age is the most powerful independent risk factor
– Gender: premenopausal ♀< risk than age-matched
♂
– The beneficial effect of ♀sex disappears rapidly
after menopause
– HRT has no role to prevent CAD
26
Risk Factors for Atherosclerosis
• Family history:
– Positive family history: when IHD occurs in first
degree relatives
– Family history is considered positive if
atherosclerosis occurs in ♂ relatives < 55 years or
♀relatives < 65 years
• Smoking
27
Risk Factors for Atherosclerosis
• Hypertension :
– Related both to systolic, diastolic and pulse
pressure
– Antihypertensive therapy has been shown to
reduce the incidence of coronary mortality, stroke,
& heart failure
28
Risk Factors for Atherosclerosis
• Hypercholeserolemia:
– Most important is total cholesterol:HDL ratio
– Lowering total cholesterol & LDL cholesterol
reduces the risk of cardiovascular events (death,
MI, stroke, & the need for revascularization)
29
Risk Factors for Atherosclerosis
• Diabetes Mellitus:
– Often associated with diffuse disease
– Insulin resistance: Normal plasma glucose despite
increased insulin levels
• Usually associated with obesity
30
Risk Factors for Atherosclerosis
• The metabolic syndrome: (syndrome X)
– Obesity
– Impaired fasting glucose: FBS 110-125 mg/dl
– Glucose intolerance: PPBS 140-200 mg/dl
– Hypertension
– Dyslipidemia: high total cholesterol: HDL
RATIO
31
Risk Factors for Atherosclerosis
• Physical inactivity:
– Regular exercise reduces risk for atherosclerosis:
• Lowers body weight
• Elevates HDL cholesterol
• Reduces BP
• Enhances Collaterals
• Reduces blood clotting
32
Risk Factors for Atherosclerosis
• Obesity
– Truncal (central)
• Alcohol?
– Moderate amount of alcohol has a protective role
– Heavy alcohol intake is associated with HT
33
Risk Factors for Atherosclerosis
• DIETARY FACTORS
– Diets deficient in fruit, vegetables, and
polyunsaturated fatty acids
• PERSONALITY?
– No evidence that emotional stress is a major risk
factor for IHD
34

PRIMARY PREVENTION
PREVENTING THE OCCURRENCE OF THE
DISEASE
• Population-based strategy
• Targeted therapy
35
PRIMARY PREVENTION
• Population-based strategy:
– Diet
• Avoiding saturated fat and cholesterol
• Increasing intake of fibers
• Low-fat dairy products
– Smoking cessation
– Exercise
• 20-30 min/day, twice or thrice a week
– Maintaining ideal body weight
36
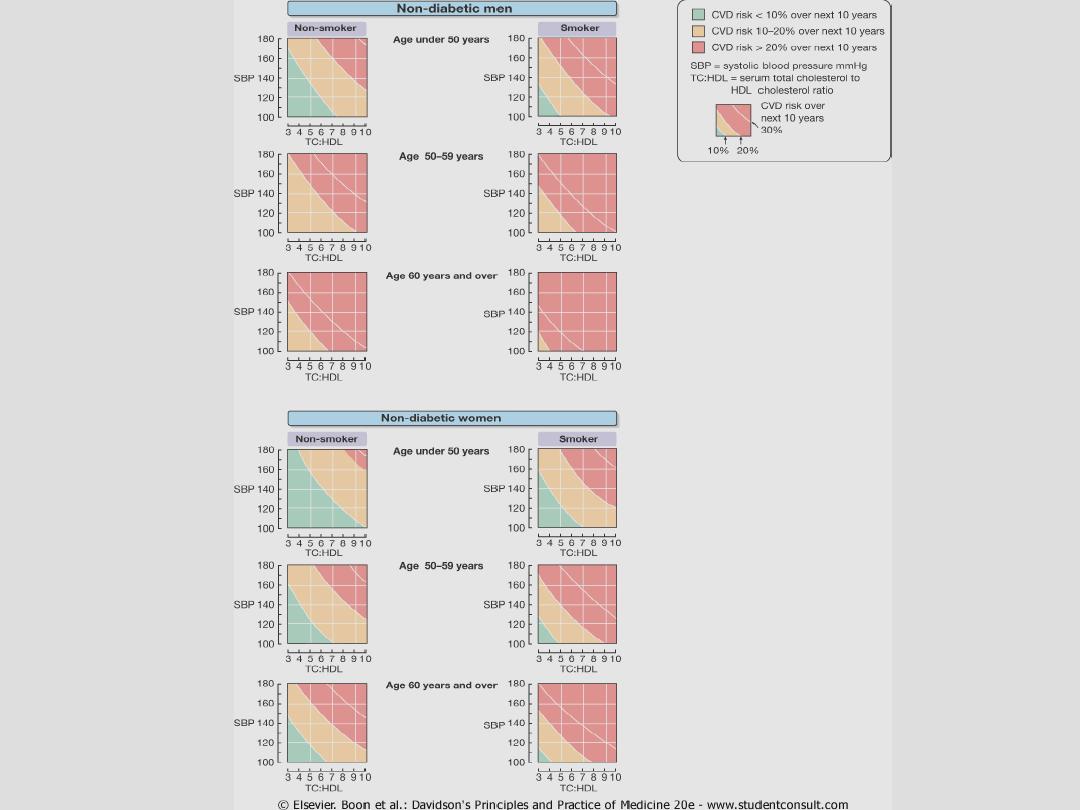
PRIMARY PREVENTION
Targeted therapy
• Identify and treat high-risk individuals
– Calculating the composite risk profile using special
algorithms and charts
• The expected benefits of therapy should be
balanced against the expenses, inconvenience,
and potential side effects of the drugs
37
Primary Prevention
• Using the risk profile charts
38
39

SECONDARY PREVENTION
PREVENTING THE RECURRENCE OF THE
DISEASE: drug therapy
•
HMG Co-A reductase inhibitors: the
“statins”
•
Aspirin
•
ACE inhibitors
40
SECONDARY PREVENTION
HMG Co-A reductase inhibitors: “statins”
(simvastatin, atorvastatin, fluvastatin, lovastatin,
rosuvastatin, etc)
– Given to All patients with established
atherosclerosis
– reduce the incidence of major coronary events &
stroke
– Should be administered at night
41
SECONDARY PREVENTION
ACE inhibitors
• e.g. captopril, enalapril, lisinopril, ramipril
• Shown to improve survival in established
atherosclerosis, even without heart failure or
LV dysfunction
42
Recent Drug: PCSK9
• Inactivation of the enzyme Preprotein
convertase subtilisin-Kexin type 9
• This leads to reduced degradation of LDL
receptors on the surface of the hepatocytes
• Increased expression of LDL receptors leading
to increased rate of clearance of LDL from the
circulation
43
