
بسم هللا الرحمن الرجيم
IN THE NAME OF GOD THE
COMPATINATE THE MOST
MERCIFULL

Respiratory diseases caused by fungi
Objectives is to know the following
Epidemiology
Risk for
Clinical presentation
Investigation
treatment

Significance
• The majority of fungi encountered by humans
are harmless saprophytes,
• but in certain circumstances some species
may infect human tissue .

Aspergillus spp
• Most cases of bronchopulmonary aspergillosis
are caused by Aspergillus fumigatus, but other
members of the genus occasionally cause
disease.

Allergic bronchopulmonary
aspergillosis (ABPA)
• ABPA is a hypersensitivity reaction to
germinating fungal spores, which may
complicate asthma and cystic fibrosis.
• It is a recognised cause of pulmonary
eosinophilia .
• The prevalence of ABPA is approximately 1-2%
in asthma and 5-10% in CF.

Factors predisposing to fungal disease
Systemic factors
• Metabolic disorders: diabetes mellitus
• Chronic alcoholism
• HIV and AIDS
• Corticosteroids and other immunosuppressant
medication
• Radiotherapy
Local factors
• Tissue damage by suppuration or necrosis
• Alteration of normal bacterial flora by antibiotic
therapy

Classification of bronchopulmonary
aspergillosis
1. Allergic bronchopulmonary aspergillosis
(asthmatic pulmonary eosinophilia)
2. Extrinsic allergic alveolitis (Aspergillus
clavatus)
3. Intracavitary aspergilloma
4. Invasive pulmonary aspergillosis
5. Chronic and subacute pulmonary
aspergillosis

Features of allergic
bronchopulmonary aspergillosis
• Asthma
(in the majority of cases).
• Proximal bronchiectasis
(inner two-thirds of
chest CT field) .
• Positive skin test
to an extract of A. fumigatus.
• Elevated total serum IgE
.
• Peripheral blood eosinophilia
.
• Presence or history of
chest X-ray abnormalities
• Fungal hyphae
of A. fumigatus on microscopic
examination of
sputum

Clinical features and investigations
depend on the
stage of disease.
• Fever.
• breathlessness.
• cough productive of bronchial casts .
• worsening of asthmatic symptoms.

Management
• ABPA
regular low-dose oral corticosteroids
(prednisolone 7.5-10 mg daily).
• itraconazole
(400 mg/day).
•
specific anti-IgE
monoclonal antibodies.
• bronchoscopy
remove impacted mucus.
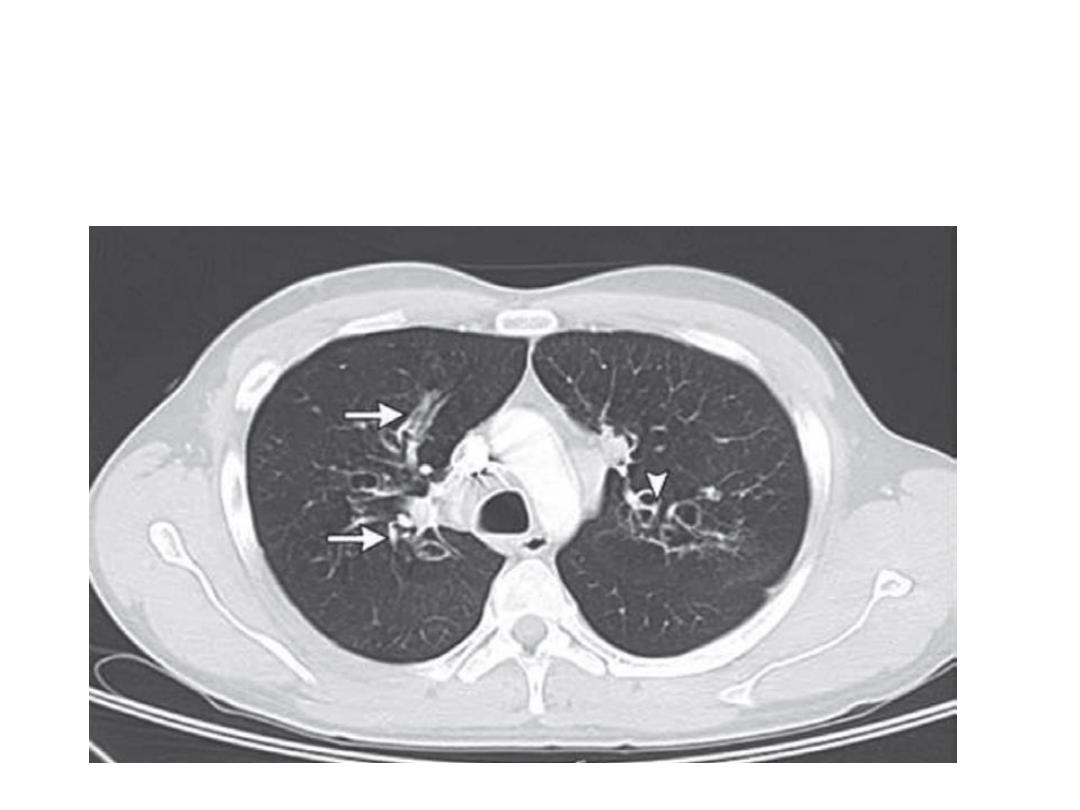
Allergic bronchopulmonary aspergillosis in a patient with a long
history of asthma. Chest radiographs showed multilobar infiltrates.
Computedtomographyshows areas of tubular ( arrows) and cystic ( arrowhead)
bronchiectasis
.
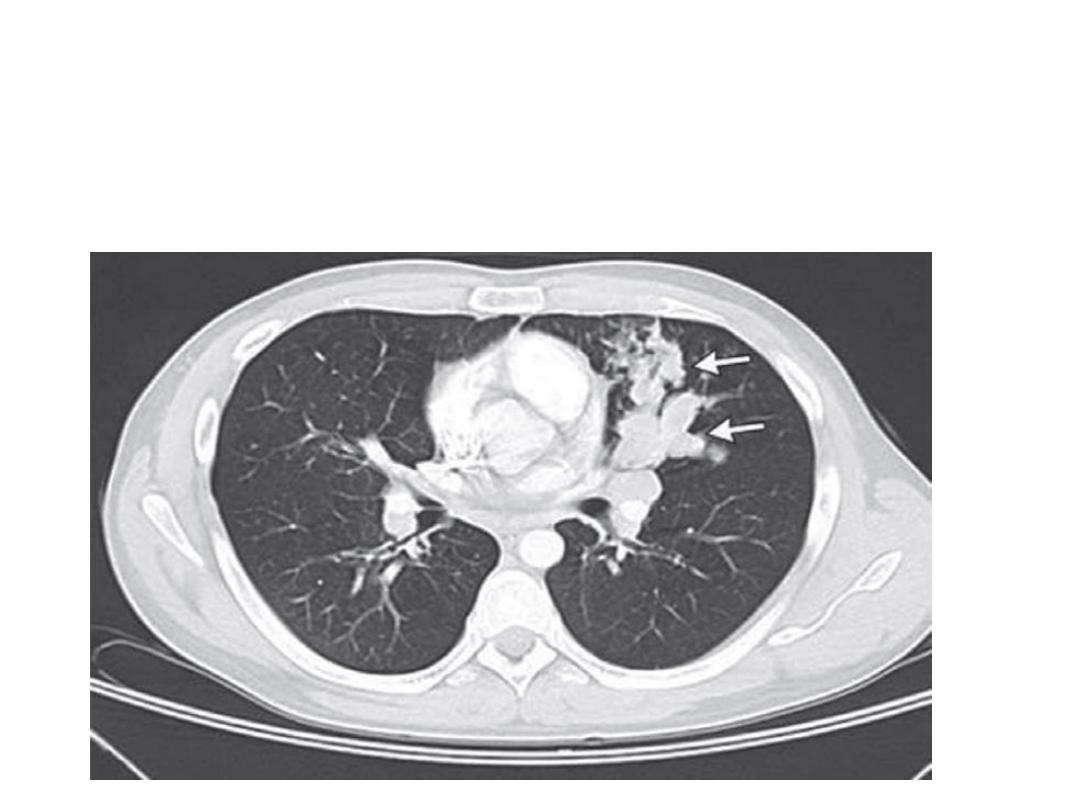
Allergic bronchopulmonary aspergillosis in a patient with a long
history of asthma. Chest radiographs showed multilobar infiltrates. Allergic
bronchopulmonary aspergillosis in a patient with a long
history of asthma. Chest radiographs showed multilobar infiltrates predominantly
in the upper lobes, and bilateral mucous plugging ( arrows) with mediastinal and hilar
lymphadenopathy

Aspergilloma
• Inhaled Aspergillus may lodge and germinate
in areas of damaged lung tissue
• a fungal ball or aspergilloma.
• The upper lobes.
• Cavities of any cause.
The 'complex aspergilloma'
presence of multiple aspergilloma cavities.

Clinical features and diagnosis
• Simple aspergillomas are often asymptomatic.
• Recurrent haemoptysis which can be severe
and life-threatening.
• The fungal ball
• presence of a crescent of air between the
fungal ball and the upper wall of the cavity.

Investigation
• HRCT is more sensitive .
• Elevated serum precipitins to A. fumigatus
• Sputum microscopy
• skin hypersensitivity to extracts of A.
fumigatus


Management
• Asymptomatic cases
do not require
treatment.
• Aspergillomas complicated by haemoptysis
should be
excised surgically
• In unfit for surgery, palliative procedures
range from local instillation of amphotericin B
---- to bronchial artery embolisation.

Invasive pulmonary aspergillosis (IPA)
• IPA is most commonly a complication of
profound neutropenia caused by drugs
(especially immunosuppressants ) .

Clinical features and diagnosis
Acute IPA
severe necrotising
pneumonia, and must be considered in any
immunocompromised patient who develops
fever, new respiratory symptoms (particularly
pleural pain or haemoptysis) or a pleural rub.

Thank you

Q
•
QUIZE
