UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
1
Definition:
Cysts are pathological fluid-filled cavities lined by epithelium.
Pathogenesis:
All cysts enlarge slowly, and there are two main mechanisms of
enlargement:
1. Hydrostatic pressure is the mechanism of cyst growth in almost all cysts. The luminal
contents are under pressure for a variety of reasons. There is poor lymphatic drainage
from the cavity, the wall and lining have partial properties of a semipermeable membrane
and the lumen contains many degraded inflammatory proteins and dead lining cells.
These factors produce an osmotic pressure that expands the cyst.
2. Growth of the wall is a less common mechanism, seen primarily in odontogenic
keratocytes. In this cyst the epithelial lining has a high mitotic rate, and the lumen is filled
with keratin, which is resistant to degradation, insoluble and thus exerts little osmotic
pressure. Instead the wall enlarges by growing, budding and insinuating finger-like
processes or developing outpouchings that extend into adjacent bone. Glandular
odontogenic cyst grows in a similar way.
Odontogenic cysts
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
2
Box 1
Common Key features of jaw cysts
➢ Clinically
• Cysts are usually asymptomatic unless they are secondarily infected.
• Tooth vitality is not affected by cysts. The radicular cyst is caused by a non-vital tooth,
but the adjacent teeth may be tipped without loss of vitality.
• Aspiration can confirm fluid contents, excluding a solid lesion.
• Cysts close to the mucosal surface may be trans illuminated and appear bluish.
• Grow slowly, displacing rather than resorbing teeth.
• Rarely large enough to cause pathological fracture.
• Form compressible and fluctuant swellings if extending into soft tissues.
➢ Radiographically
• The radiographic appearance of cysts is characteristic and sharply-defined
radiolucencies with corticated smooth borders (i.e., condensing osteitis) with a
radiolucent center.
• Most cysts are unilocular; however, multilocular forms are often seen in some
keratocysts and cystic ameloblastomas.
• Cysts do not usually cause resorption of the roots of teeth; therefore, when resorption
is seen, the clinician should suspect a neoplasm.
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
3
Classification
According to World Health Organization (WHO) classification 2017 (Box 2), Cysts can be classified
into two groups based on the origin of the epithelium that lines the central cavity.
➢ Odontogenic cysts are lined by odontogenic epithelium derived from the dental lamina.
This epithelium originates by proliferation of rests of Serres, reduced enamel epithelium
or rests of Malassez. Odontogenic cysts, therefore, can only affect the tooth-bearing
regions of the jaws. Odontogenic cysts are subclassified as:
• Developmental.
• Inflammatory.
➢ Nonodontogenic cysts those arising from oral epithelium that is trapped between fusing
processes during embryogenesis and they are usually developmental in origin.
Box 2
World Health Organization (WHO) classification of Cysts of the jaws, face and neck
ODONTOGENIC CYSTS
NON-ODONTOGENIC CYSTS
➢ Cysts of inflammatory origin
Radicular cyst
Residual cyst
Inflammatory collateral cysts
➢ Cysts of developmental
Dentigerous cyst
Eruption cyst
Odontogenic keratocyst
Ortho-keratinised odontogenic cyst
Lateral periodontal cyst
Botryoid odontogenic cyst
Glandular odontogenic cyst
Gingival cyst of infants
Gingival cyst of adults
Incisive canal cyst
Nasolabial cyst
Sublingual dermoid cyst
Thyroglossal duct cyst
Branchial cyst
Foregut cysts
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
4
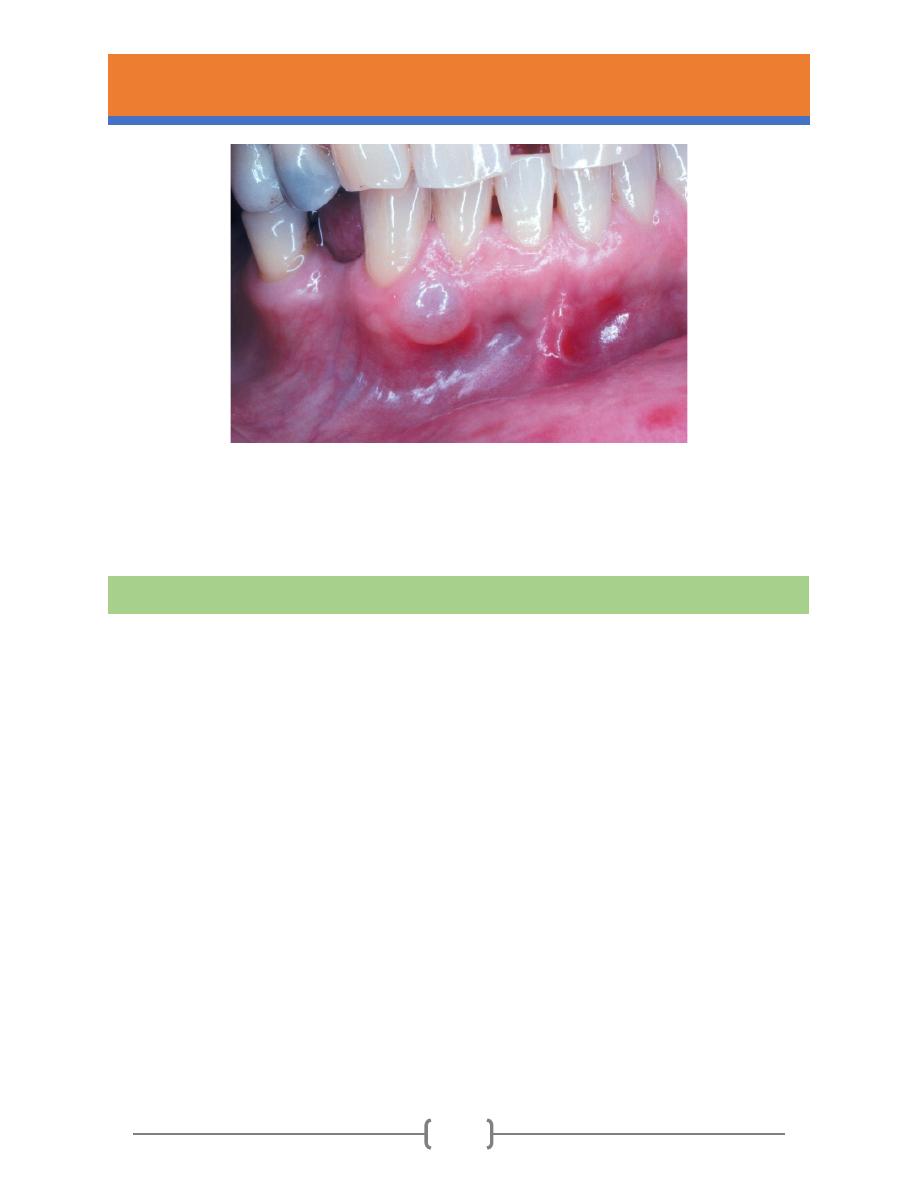
➢ Clinical features
• It is a cyst form in relation to the root of an existing non-vital tooth.
• Slowly progressive painless swelling, with no symptoms until the cyst or becomes
infected or large enough to be noticed.
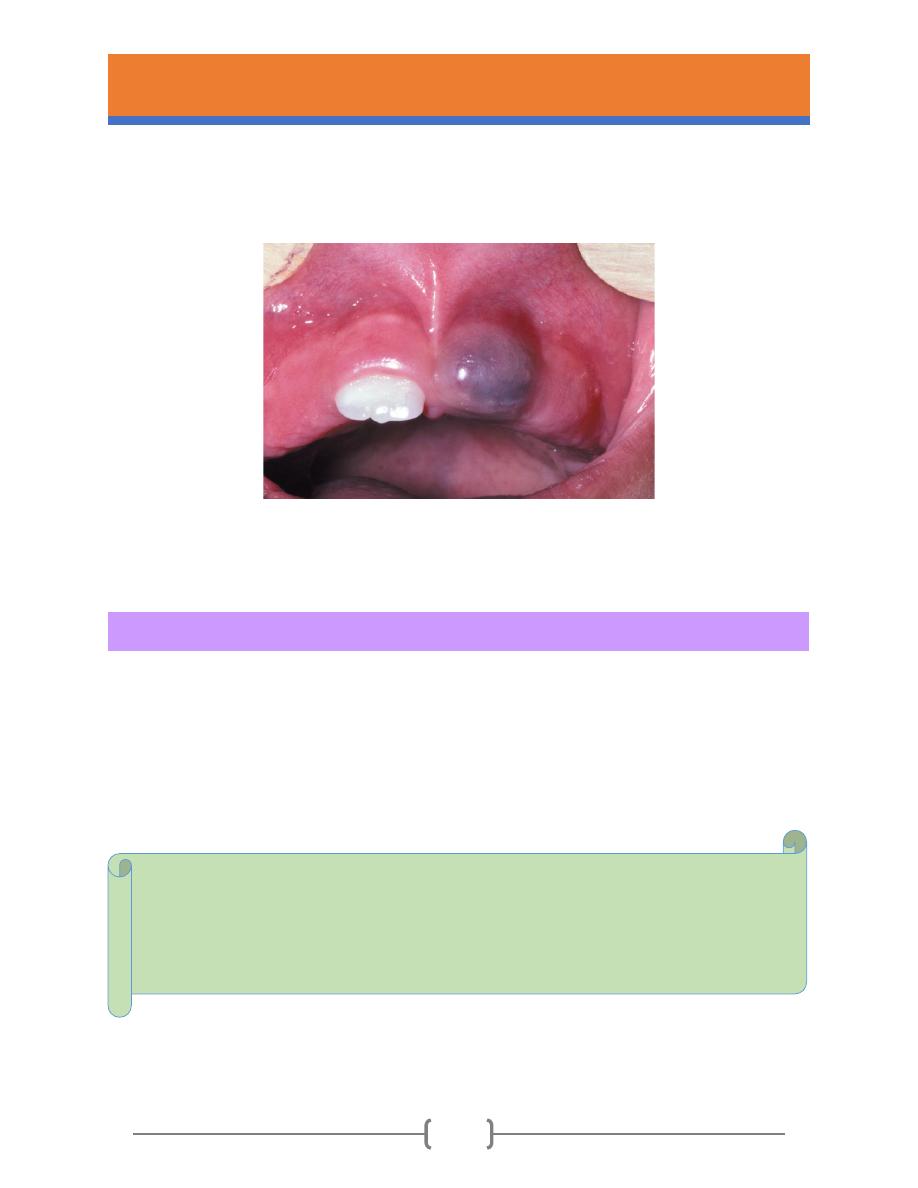
• The swelling is rounded and at first hard. Later, when the bone has been reduced to
eggshell thickness, a crackling sensation may be felt on pressure. Part of the wall is
resorbed entirely away, leaving a soft fluctuant swelling, bluish in colour, beneath the
mucous membrane. (Fig.1)
Fig.1- Typical clinical appearance of a large cyst. This radicular cyst in the right maxillary alveolar process
forms a rounded swelling with a bluish colour.
➢ Radiographical features
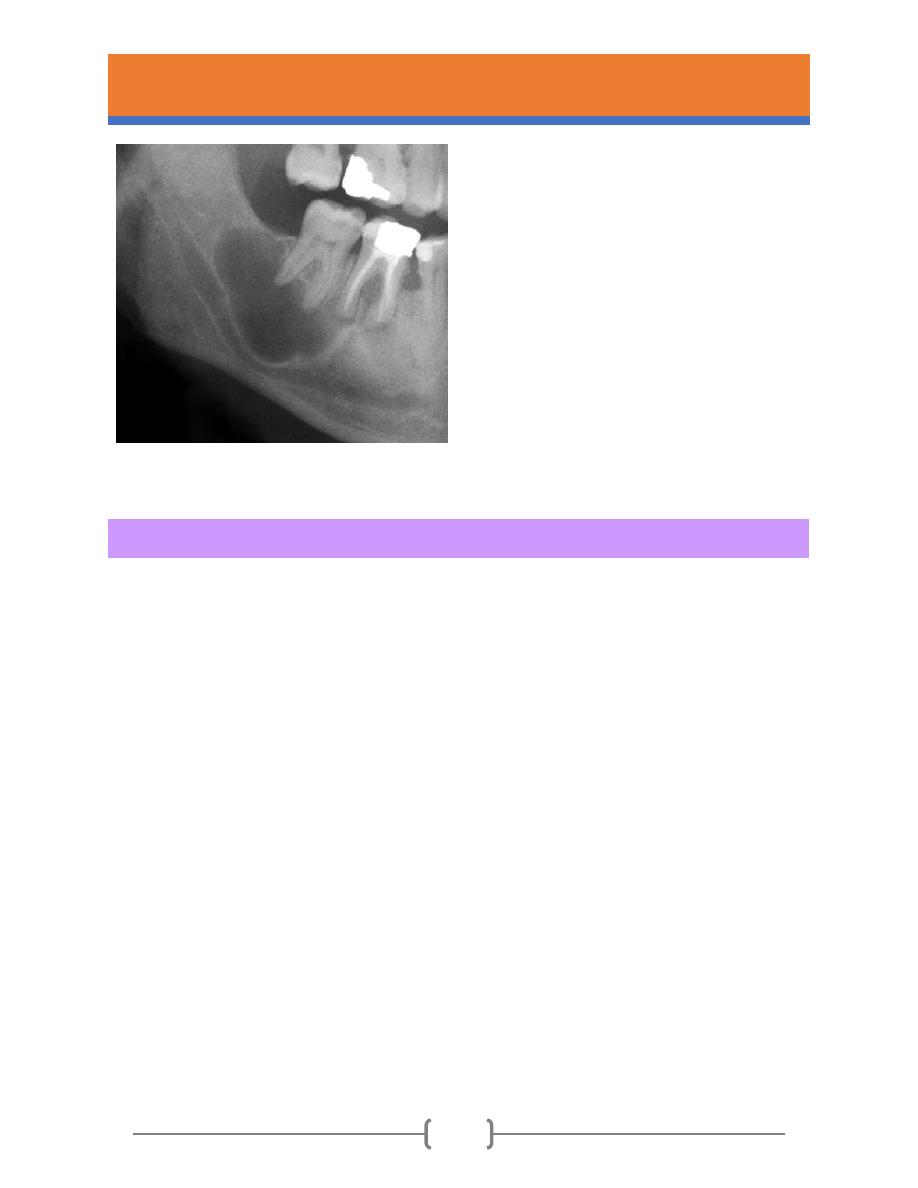
• A radicular cyst appears as a rounded, radiolucent area with a sharply defined outline.
• A condensed radiopaque corticated periphery is present and more prominent in
longstanding cysts.
• The dead tooth from which the cyst has arisen can be seen and often has a large carious
cavity or other cause evident.
• Adjacent teeth may be tilted or displaced and can become slightly mobile bony(Fig.2).
Radicular cysts (periapical cysts)
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
5
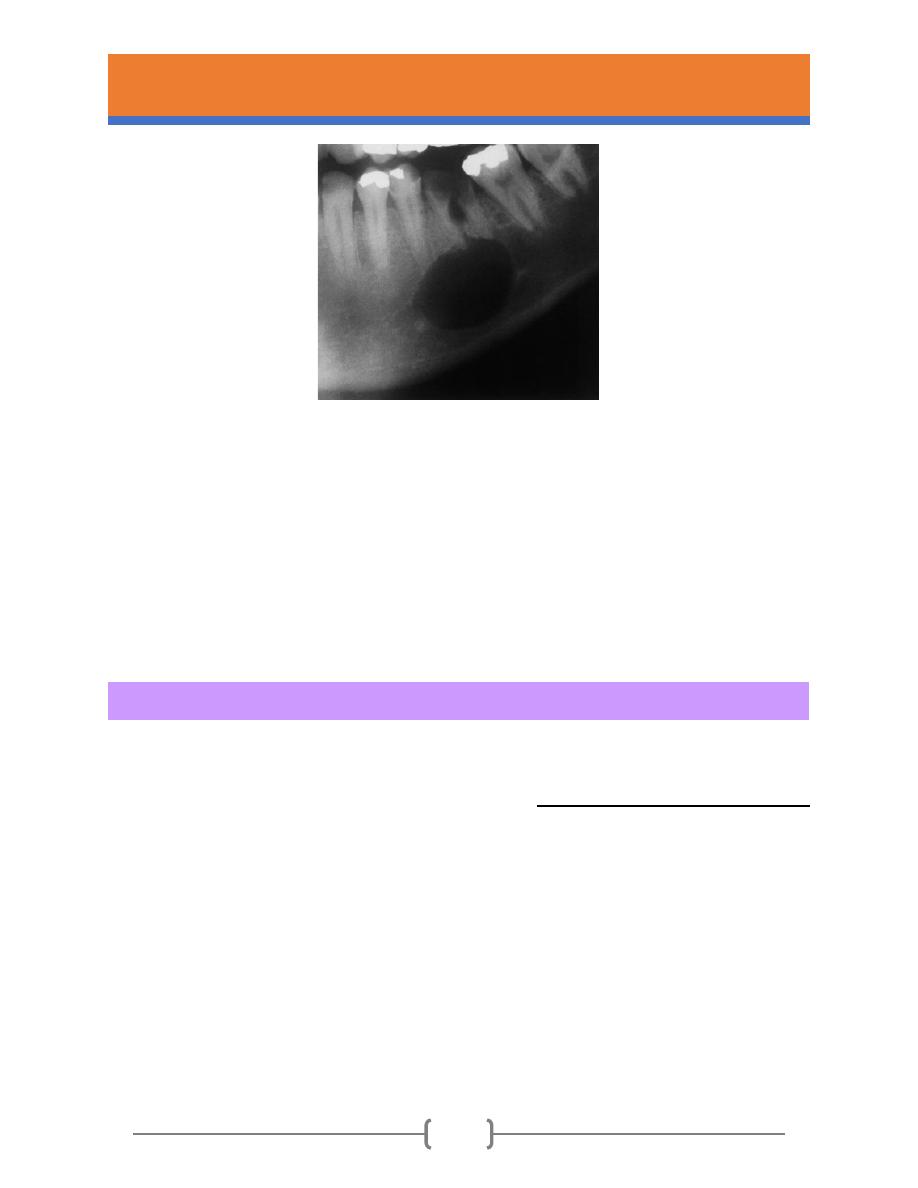
Fig.2- A radicular cyst on a grossly carious and non-vital first permanent molar. A rounded and sharply defined area
of radiolucency is associated with the apices of the roots.
➢ Treatment
Radicular cysts are treated by enucleation. The associated non-vital tooth is usually extracted if
it is unrestorable or it can be preserved by placing an orthograde root filling before surgery and
performing an apicectomy and retrograde filling, usually with mineral trioxide aggregate, when
the cyst is enucleated.
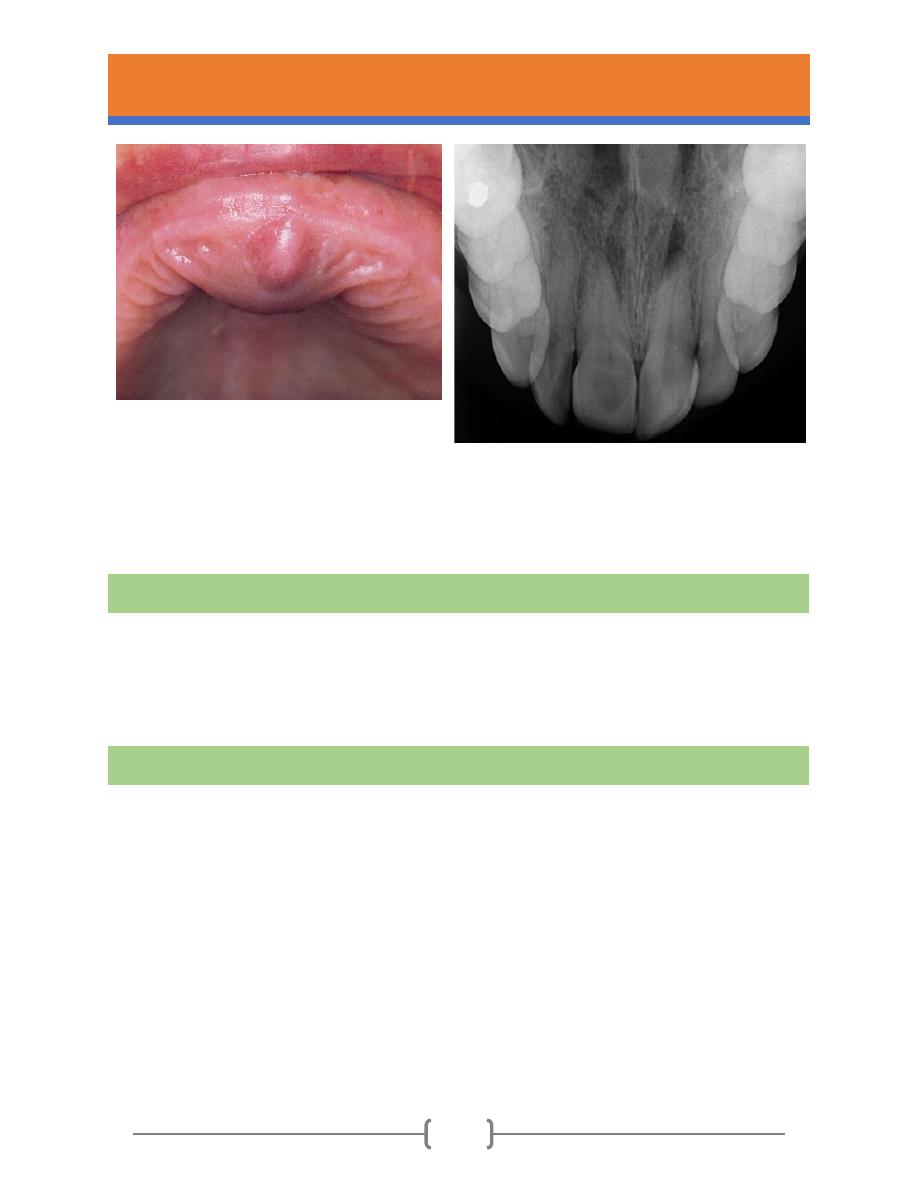
Residual radicular cyst
A residual radicular cyst is a radicular cyst that has persisted after extraction of the causative
tooth. The features are identical to other radicular cysts, except that tooth has been removed
(Fig. 3). Residual cysts are more frequent in older persons and present with expansion of the jaw.
(Fig. 4).
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
6
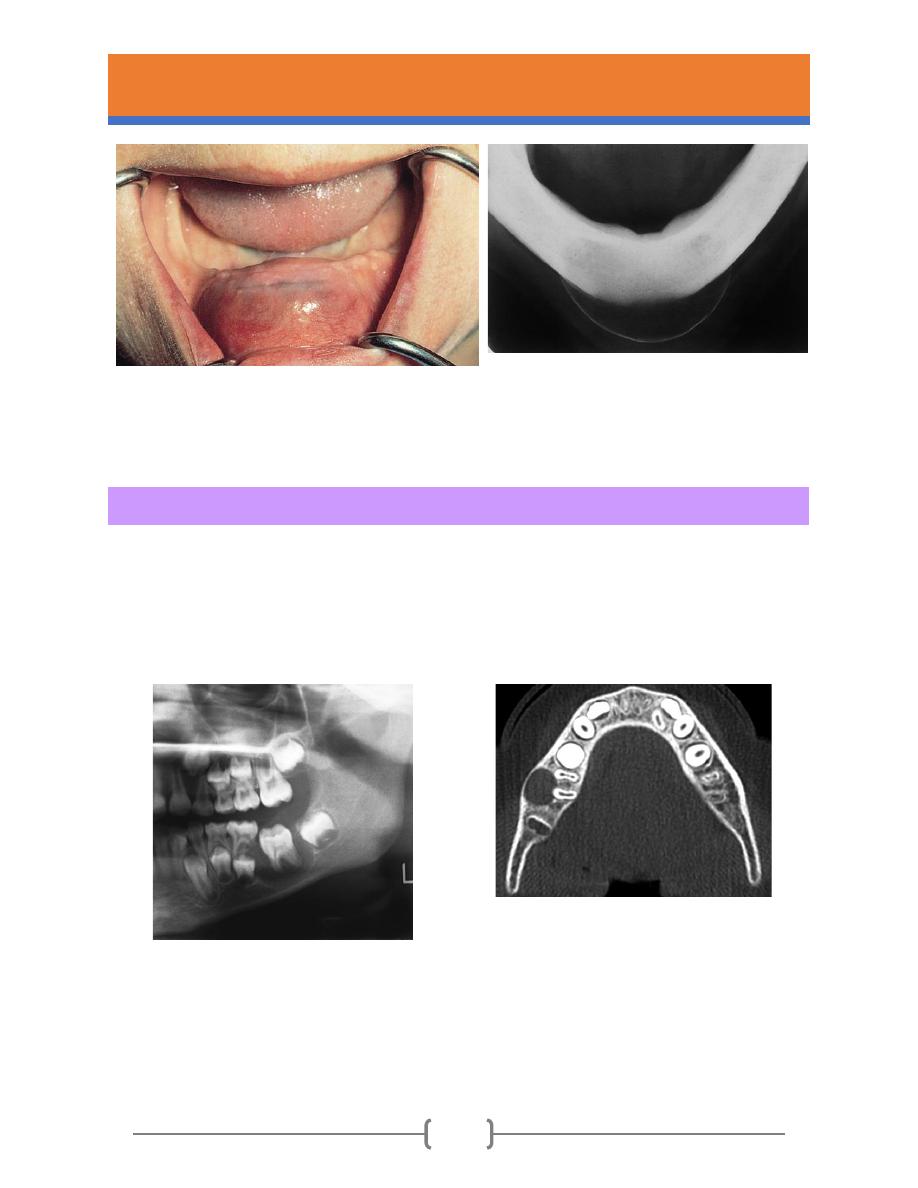
Fig.3- Residual cyst. The causative tooth has been
extracted leaving the cyst in situ.
Fig.4- Radiographic appearance of the residual cyst
shown in Fig.3. Note the thin bulging periosteal new
bone layer which can give rise to the clinical sign of
eggshell crackling.
Inflammatory Collateral Cysts
These are rare cysts adjacent to the cervical area or furcation of molars, particularly mandibular
molars. The affected tooth is vital but typically shows pericoronitis or gingival inflammation (Fig.5
& Fig.6).
Fig.5- Buccal Bifurcation Cyst. Well-circumscribed
unilocular radiolucency superimposed on the roots of
the mandibular first permanent molar.
Fig.6- Buccal Bifurcation Cyst. Axial computed
tomography (CT) image showing a circumscribed
radiolucency buccal to the roots of the mandibular first
molar.
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
7
Dentigerous cyst (Follicular cyst)
The dentigerous cyst is a cyst around the crown of an unerupted tooth, with the epithelial lining
attached around the cemento-enamel junction.
➢ Clinical features
• Dentigerous cysts are more than twice as common in males as females.
• The cysts expand the jaw with displacement of adjacent structures.
• The key diagnostic feature is the dentigerous relationship to the tooth (Fig.7).
• Most frequently associated with unerupted third molars and canines.
• Respond to enucleation or marsupialisation and do not recur after treatment.
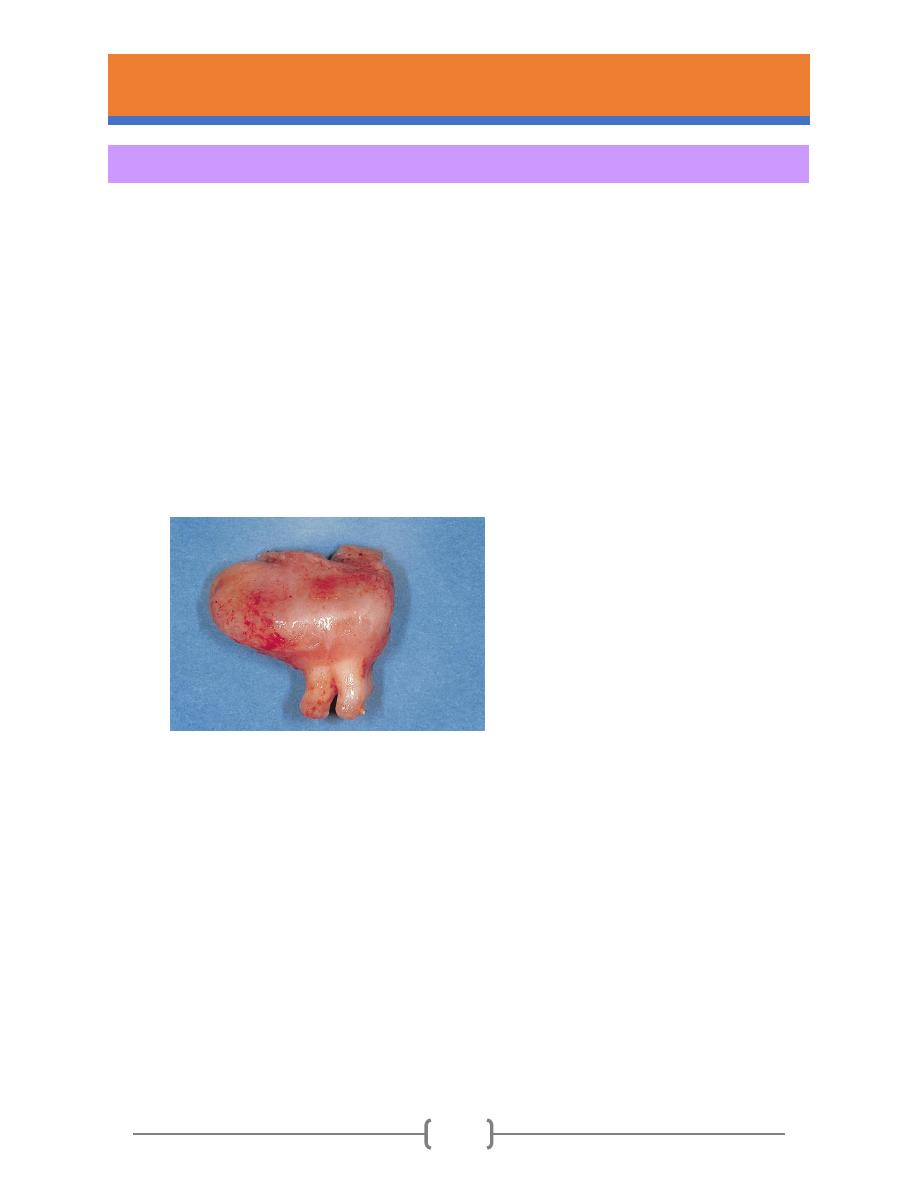
Fig. 7- Dentigerous cyst. This cyst has been
removed together with its associated tooth.
The cyst surrounds the crown and is attached
at the cementoenamel junction.
➢ Radiographical features
• The cavity is circumscribed, rounded and always unilocular and contains the crown of the
tooth (Fig. 8).
• Cysts may attain a very large size, larger than 10 cm, and large cysts may appear to be
multilocular on radiographs (pseudoloculation) because bony ridges on the inside of the
bony cavity are superimposed on the image.
• The affected tooth is often displaced a considerable distance, lower third molars to the
lower border of the mandible or high in the ramus.
• In longstanding cysts, the enclosed tooth may become resorbed (Fig. 9).
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
8
Fig. 8- Dentigerous Cyst. Central type showing the
crown projecting into the cystic cavity.
Fig.9- Resorption of tooth associated with a
dentigerous cyst. The crown of this buried canine
within the cyst shows resorption. This is seen only in
longstanding cysts, as in this otherwise edentulous
patient.
➢ Treatment
Dentigerous cysts are usually treated by enucleation with removal of the unerupted tooth.
However, for other teeth, such as maxillary canines that are in a favourable position, it may be
possible to marsupialise a dentigerous cyst to allow the tooth to erupt, providing space and
traction orthodontically if necessary. The prognosis for most dentigerous cysts is excellent, and
recurrence seldom is noted after complete removal of the cyst.
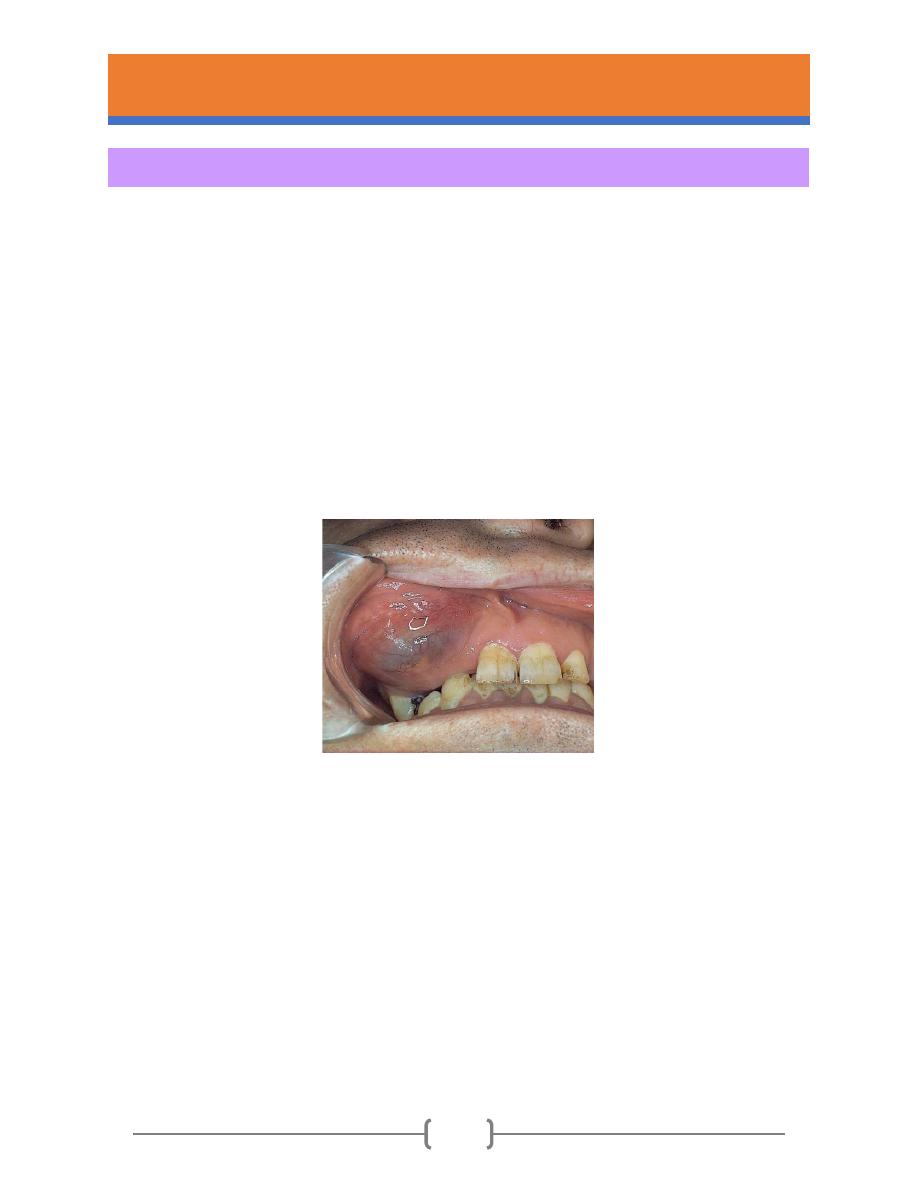
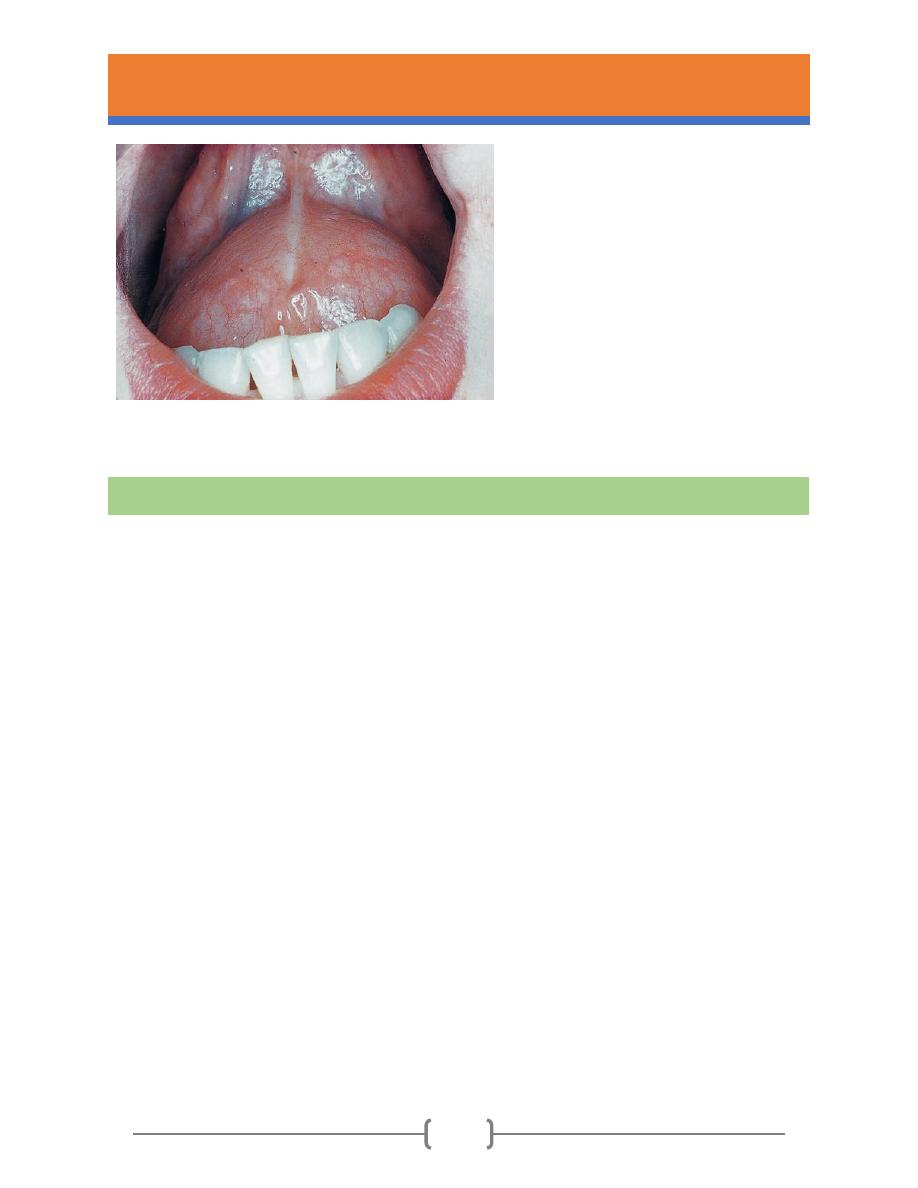
Eruption cyst
• An eruption cyst is arising on a tooth during eruption, therefore seen in children.
• Forming a soft, rounded, swelling on the alveolus.
• Trauma to the cyst causes internal bleeding and a dark blue colour (Fig. 10).
• Treatment may not be required because the cyst usually ruptures spontaneously,
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
9
permitting the tooth to erupt. If this does not occur, then simple excision of the roof of
the cyst generally permits speedy eruption of the tooth.
Fig. 10- Eruption Cyst. This soft gingival swelling contains considerable blood and can also be designated as an
eruption hematoma.
Odontogenic keratocyst (OKC)
OKC is a distinctive form of developmental odontogenic cyst because of three reasons:
1. Greater growth potential than most other odontogenic cysts.
2. Higher recurrence rate.
3. Possible association with the nevoid basal cell carcinoma syndrome.
Note
Several investigators have suggested that the OKC be regarded as a benign cystic
neoplasm rather than a cyst, and this lesion has been given the name keratocystic
odontogenic tumor (KCOT). Many studies have shown certain molecular genetic
alterations that are also present in some neoplasms.

UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
10
➢ Clinical features
• Accounting 5%–11% of jaw cysts.
• Incidence peaks in second and third decades, mean age 38 years.
• The mandible is involved in 60% to 80% of cases, with a marked tendency to involve the
posterior body and ramus.
• Grow around teeth without displacing them.
• OKCs tend to grow in an anteroposterior direction within the medullary cavity of the bone
without causing obvious bone expansion. This feature may be useful in differential clinical
and radiographic diagnosis because dentigerous and radicular cysts of comparable size
are usually associated with bony expansion.
• May recur after enucleation.
• Definitive diagnosis only by histopathology.
• May be confused with ameloblastoma or with dentigerous cysts radiographically.
• May be part of the basal cell naevus (Gorlin’s) syndrome
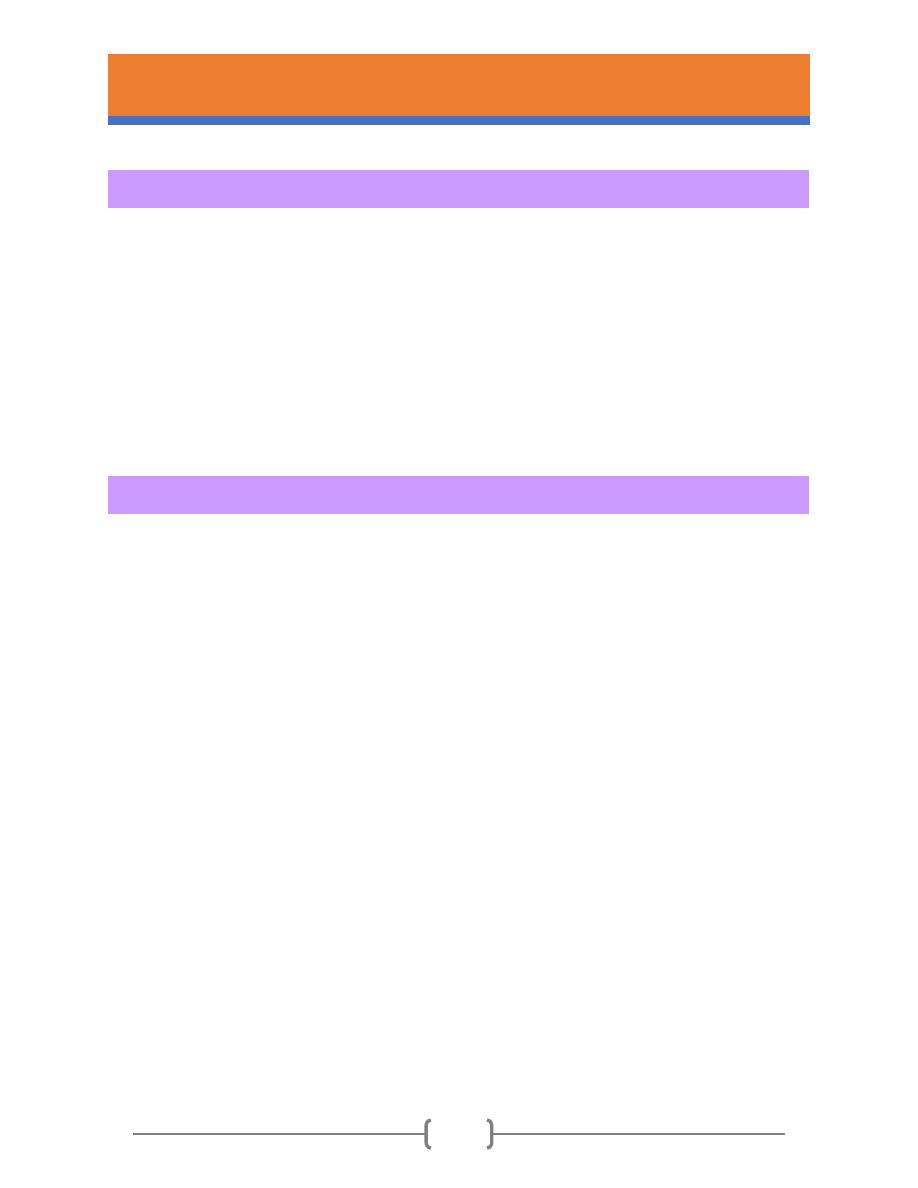
➢ Radiographical features
• Odontogenic keratocysts produce well-defined radiolucent areas, with a more or less
rounded or scalloped margin. Some are unilocular, but the majority are multilocular
(Fig.11).
• The margin is sharply demarcated and corticated.
•
The characteristic growth pattern is evident radiologically and is almost diagnostic. There
is extensive spread forward and backward along the medullary cavity with minimal
expansion until the whole of the medulla is replaced (Fig.12).
•
There is minimal displacement and no resorption of teeth or the inferior dental canal.

UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
11
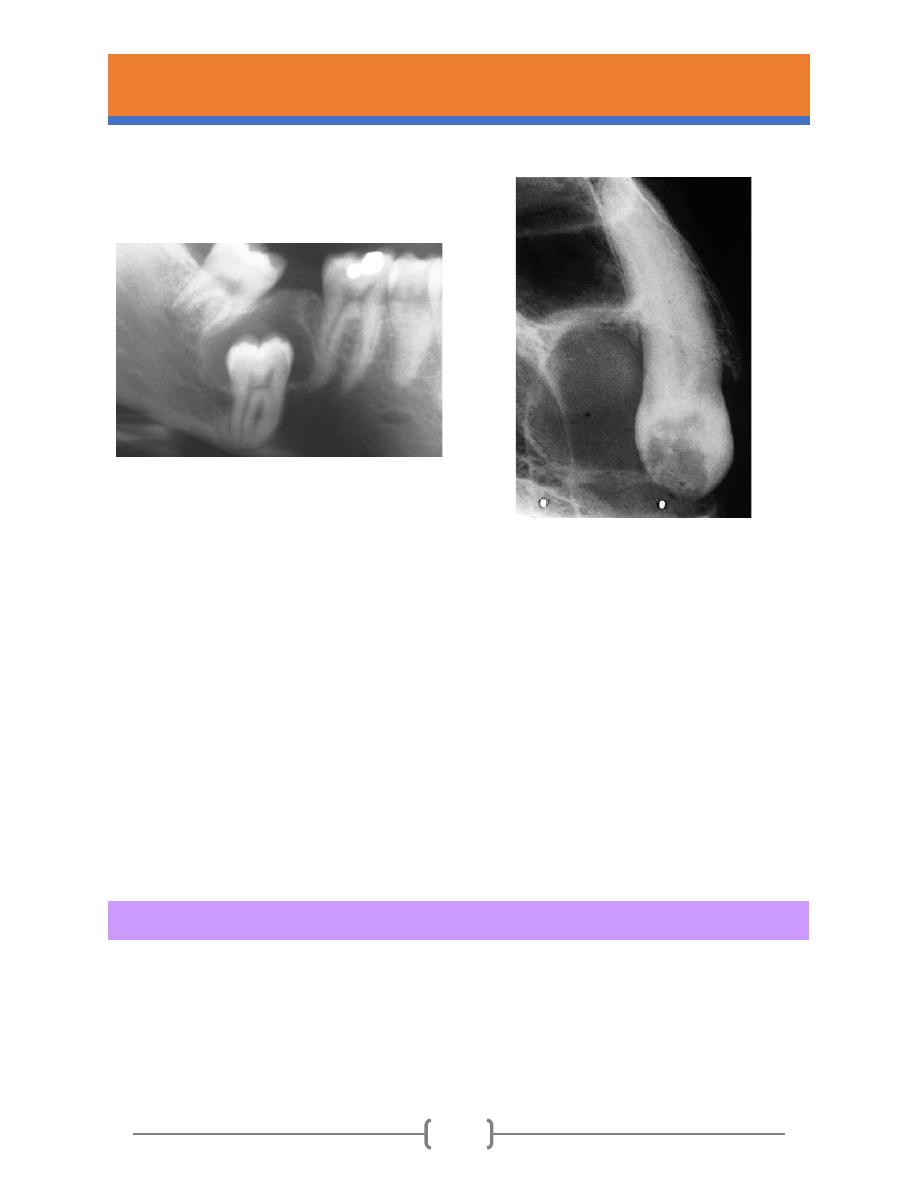
Fig.11- Odontogenic keratocyst. Part of a
panoramic tomogram showing typical
appearances. The cyst is multilocular and
has extended a considerable distance
along the medullary cavity without
appreciable expansion or displacement
of the teeth.
Fig.12- Odontogenic keratocyst. Huge lesion extending from
coronoid to the opposite molar region with minimal tooth
displacement or expansion of bone.
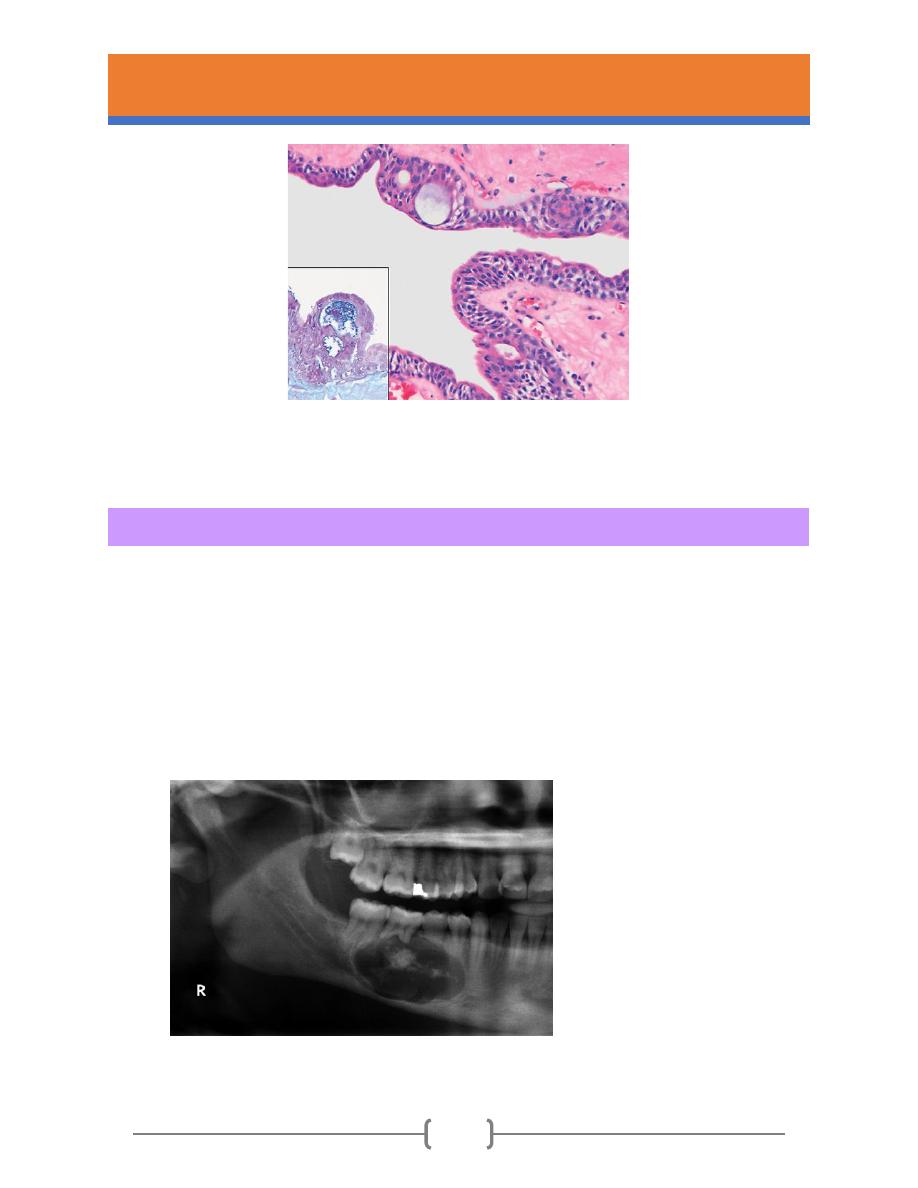
➢ Histological features
• Epithelial lining of uniform thickness with flat basal layer.
• Thin eosinophilic layer of parakeratin with corrugated surface.
• Clearly defined basal layer of palisaded ameloblast-like basal cells at least focally with
reversed polarity (Fig. 13).
• Epithelial lining weakly attached to the fibrous wall.
• Thin fibrous wall.
• Satellite cysts in the wall.
• Inflammatory cells typically absent or scanty

UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
12
Fig. 13- Odontogenic keratocyst. Showing the
typical features of the epithelial lining: a flat
basement membrane; elongated palisaded basal
cells with focal reserve polarity; 10–20 cells in
thickness and with a corrugated parakeratotic
surface.
➢ Treatment and recurrence
Recurrence has several contributing causes (Box 3). Historically, recurrence rates of more than
50% were reported, but with the thorough treatment, recurrence rates of 2%–3% can be
achieved. Ideally, therefore, diagnosis should be confirmed by biopsy. Treatment depends largely
on the extent of the cyst and the degree of multilocularity.
Box 3
Possible reasons for recurrence of keratocysts
• Thin, fragile linings, difficult to enucleate intact.
• Finger-like cyst extensions into cancellous bone.
• Satellite (daughter) cysts sometimes present in the wall.
• More rapid proliferation of keratocyst epithelium.
• Experience of surgeon.
• Formation of additional new cysts from other dental lamina remnants.

UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
13
➢ Treatment options of OKC
❖ Enucleation and curettage: Unilocular and small multilocular cysts are usually enucleated
and the bony cavity curetted vigorously to remove every fragment of cyst lining. A useful
additional precaution is the treatment of the cavity wall with a fixative (Carnoy’s solution).
This can be applied either before enucleation to kill and toughen the lining for removal or
to the bony walls after curettage to destroy residual epithelial cells. It kills and denatures
tissue to a depth of approximately 1–2 mm, far enough to kill the full thickness of the
wall. However, it is a caustic mixture of ferric chloride in alcohol, chloroform and highly
concentrated acetic acid and must be used with care near vital structures such as the
inferior dental neurovascular bundle.
❖ Marsupialisation and enucleation: Reduction in size is associated with ingrowth of oral
epithelium into the cavity, replacing the typical keratinised epithelium with non-
keratinising stratified squamous epithelium. This makes enucleation of the residual cyst
much easier, and recurrence is less frequent than after enucleation alone. Complete
resolution after marsupialisation is possible but takes a long time, as long as 20 months,
and it requires cooperative patients who will irrigate the cavity and keep it open and clean
until it resolves. However, use as a primary treatment is increasing because the morbidity
is considerably less than radical surgery, and the procedure is simpler than trying to
enucleate the lining from a large cavity with a complex shape.
❖ Resection and reconstruction
For the most extensive cysts, resection and reconstruction with a bone graft may be
required. This controls recurrence but carries high morbidity. Posterior maxillary cysts
may be treated more aggressively as they can be difficult to eradicate if they escape the
confines of the bone and occasionally these extend to the skull base.

UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
14
Lateral periodontal cyst
➢ Clinical features
• Form in the periodontal ligament beside the mid portion of the root of a vital tooth.
• More than three-quarters arise in the lower canine and premolar region, and their
location is characteristic and almost diagnostic (Fig.14).
• Symptoless, usually seen by chance in routine radiographs.
• Respond to enucleation.
Fig. 14- Lateral periodontal cyst.
A larger lesion
causing root divergence.
Botryoid odontogenic cysts
➢ Clinical features
• Rare variant of lateral periodontal cyst (Fig.15).
• Affect the mandibular premolar to canine region.
• Have a tendency to recur after enucleation
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
15
Fig.15- Botryoid odontogenic cyst. There is corticated
and well-defined radiolucency with a scalloped outline
as evidence of possible multilocularity, but no other
clue as to the cyst type.
The glandular odontogenic cyst (sialo-odontogenic cyst)
➢ Key features
• Rare developmental odontogenic cyst, usually in the mandible, anterior to molars.
• The cysts are frequently multilocular
and expand the jaw and displace and resorb teeth.
• The cyst has a diagnostic histological appearance with small glands that are lined by
mucous cells and secrete mucin and lie in thickenings of the epithelial lining (Fig.16).
• Has a strong tendency to recur. Approximately a third of cases recur after enucleation
and additional curettage and sacrifice of teeth or conservative excision may be necessary.
• Small lesions may be enucleated with curettage.
• Large multilocular lesions are excised conservatively.
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
16
Fig. 16- Glandular odontogenic cyst. The epithelial lining has an occasional plaque similar to those in lateral
periodontal cysts and contains small glands or duct-like spaces.
Calcifying odontogenic cyst
➢ Key features
• Any age and either jaw can be affected.
• The site is most often in bone anterior to the first molar.
• Radiographically, the appearance is usually unilocular but may be multilocular and
contain flecks or dense masses of calcification which suggests the diagnosis (Fig. 17).
• Usually responds to enucleation, but solid lesions are distinct and more aggressive.
Fig. 17- Calcifying Odontogenic Cyst.
Well-circumscribed mixed
radiolucent/radiopaque lesion in the
right body of the mandible.
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
17
Gingival cysts of newborn
➢ Key features
• Small cysts of the dental lamina can be found in as many as 80% of newborn infants.
• They form small nodules or cysts on the alveolar ridge, each up to 2 mm diameter.
• Their whitish colour is caused by their content of keratin.
• Treatment and Prognosis: No treatment is indicated for gingival cysts of the newborn
because the lesions spontaneously involute as a result of the rupture of the cysts and
resultant contact with the oral mucosal surface.
Gingival cysts of adult
➢ Key features
• Gingival cysts in adults present after the age of approximately 40 years, most often in
the lower canine and premolar region.
• The cysts form dome-shaped swellings less than 1 cm in diameter and sometimes erode
the underlying bone by pressure (Fig.18).
• They are lined by very thin, flat, stratified squamous epithelium and may contain fluid or
layers of keratin.
• Treatment and Prognosis: surgical excision. The prognosis is excellent.
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
18
Fig. 18- Gingival Cyst of the Adult. Tense, fluid-filled swelling on the facial gingiva.
NON-ODONTOGENIC CYSTS
Nasopalatine cyst (ncisive canal cysts)
➢ Key features
• It is the commonest non-odontogenic cyst of the jaws.
• Often asymptomatic.
• Form in the incisive canal region (Fig.19).
• Lined by squamous or columnar respiratory epithelium.
• Radiography shows a rounded radiolucent area with a corticated outline at the site of
the incisive canal.The root apices of the central incisors are often pushed apart (Fig.20).
• Do not recur after enucleation.
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
19
Fig. 19- Nasopalatine cyst. Typical presentation with
a dome-shaped bluish enlargement overlying the
incisive canal.
Fig. 20-Nasopalatine cyst. The usual appearance is a
rounded or pear-shaped area of radiolucency, at the site
of the incisive canal.
Nasolabial Cysts
➢ Key features
• The cysts form soft tissue swellings in the upper lip, distort the nostril.
• The cyst is excised, usually from an intraoral approach through the labial sulcus.
Sublingual dermoid cysts
➢ Key features
• These are cysts above the hyoid and mylohyoid, immediately beneath the tongue (Fig.21).
• They are lined by a keratinising stratified squamous epithelium like skin, complete with
associated sebaceous glands, sweat glands and sometimes hair follicles.
• A sublingual dermoid is more deeply placed than a ranula, lacks the bluish appearance
and is firmer.
• They are asymptomatic when small, enlarge to interfere with speech or eating.
• These cysts are removed by excision.
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
20
Fig. 21- Sublingual dermoid cyst. This cyst,
unlike a ranula, can be seen to have a thick wall
because it has arisen in the deeper tissues of
the floor of the mouth.
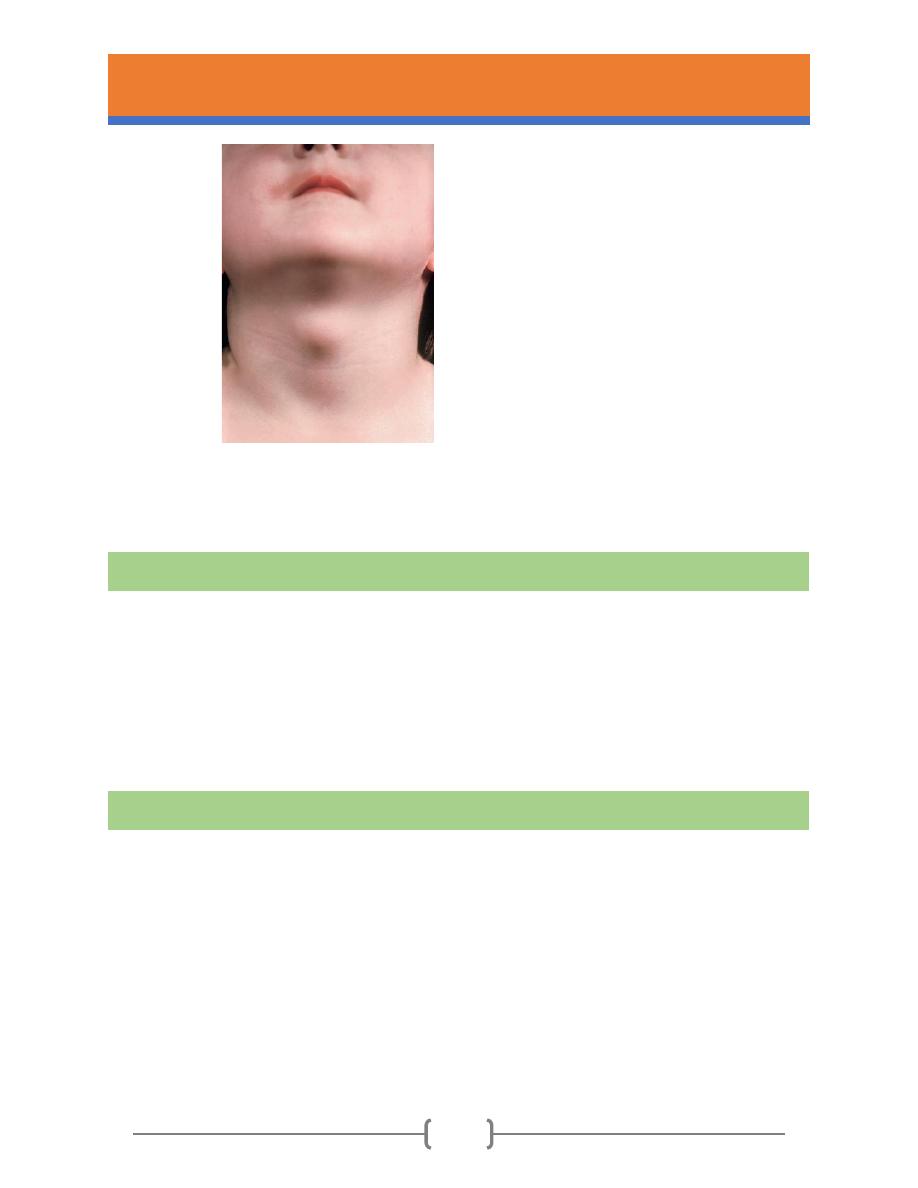
Thyroglossal duct cysts
➢ Key features
• Develop from embryological epithelial remnants of the thyroglossal duct.
• Present in the area of the body of the hyoid bone forming swellings in the midline neck
skin in adolescents and young adults (Fig. 22).
• Histologically, the cysts are lined by stratified squamous epithelium or respiratory
epithelium, and there are often clusters of ectopic thyroid tissue in the wall.
• Treatment: surgical removal with the body of the hyoid bone and tissue along the line of
the tract down to the gland. This prevents recurrence.
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
21
Fig. 22- Thyroglossal cyst. A typical thyroglossal
cyst in the midline close to the body of the hyoid
bone and just below the skin.
Branchial cyst
➢ Key features
• Caused by the failure of fusion of the five pharyngeal arches.
• The commonest is the second branchial arch cyst, which is visible externally at the
anterior border of sternomastoid muscle just below the angle of the mandible.
• Sometimes the cysts open to the skin and are then known as branchial clefts.
Foregut cyst
These very rare cysts are developmental anomalies in children and adolescents, usually in the
midline ventral tongue or floor of mouth. The cyst is lined by gastric or other intestinal mucosa
and is treated by excision.
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
22
Surgical Management of Cysts
Cysts of the jaws are treated using one of the following four basic methods:
1. Enucleation.
2. Marsupialization.
3. A staged combination of the two procedures.
4. Enucleation with curettage
1. Enucleation
It is the process by which the total removal of a cystic lesion is achieved. By definition, it means
a shelling-out of the entire cystic lesion without rupture.
➢ Indications
Enucleation is the treatment of choice for removal of cysts of the jaws and should be used with
any cyst of the jaw that can be safely removed without unduly sacrificing adjacent structures.
➢ Advantages
1. The cavity usually heals without complications.
2. Little aftercare is necessary. The patient does not have to care for a marsupial cavity
with constant irrigations.
3. The complete lining is available for histological examination.
4. The initial excisional biopsy (i.e., enucleation) has also appropriately treated the lesion.
➢ Possible disadvantages
1. Infection of the clot filling the cavity.
2. Recurrence due to incomplete removal of the lining.
3. Serious haemorrhage.
4. Devitalization of teeth.
Keep in mind that the
Basic Surgical Goals are:
1.Eradication of Pathologic
Condition.
2.Functional Rehabilitation
of Patient.
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
23
5. Damage to the inferior dental nerve.
6. Opening the antrum when enucleating a large maxillary cyst.
7. Fracture of the jaw if an exceptionally large mandibular cyst is enucleated.
➢ Technique
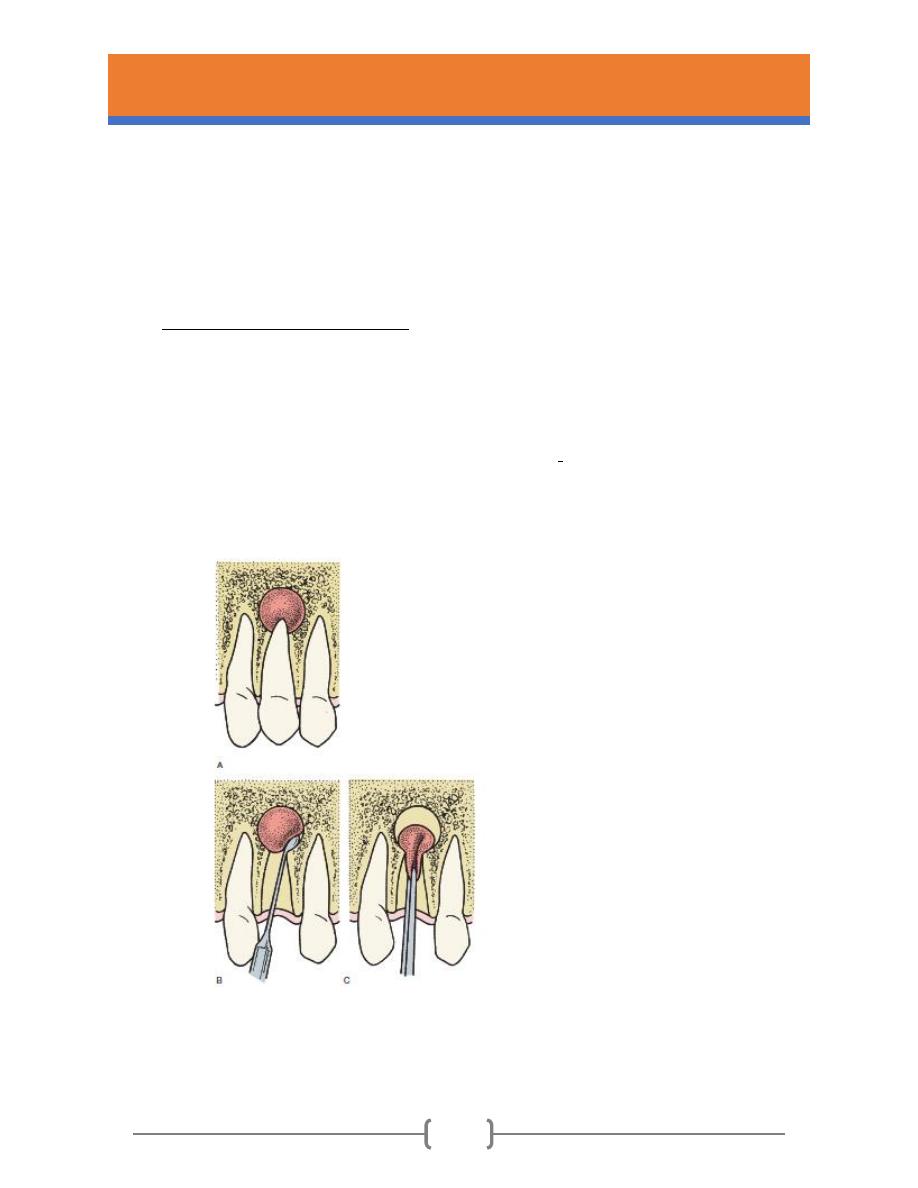
❖ Enucleation via extraction socket
When extracting teeth with periapical radiolucencies, enucleation via the tooth socket can be
readily accomplished by using curettes when the cyst is small (Fig. 23) Caution is used in teeth
with apices that are close to important anatomic structures such as the inferior alveolar
neurovascular bundle or the maxillary sinus because the bone apical to the lesion may be
very thin or non-existent.
Fig. 23-Apical cystectomy performed at
time of tooth removal. (A–C) Removal of a
cyst with curette via a tooth socket is
visualized. An apical cystectomy must be
performed with care because of the
proximity of the apices of teeth to other
structures such as the maxillary sinus and
the inferior alveolar canal.
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
24
❖ Enucleation via mucoperiosteal flap
A mucoperiosteal flap over the cyst is raised and a window is opened in the bone large
enough to give adequate access. The soft tissue of the cyst wall is then separated from
the bony wall. In thick-walled cysts it separates cleanly with a blunt instrument and scoops
out easily; in thinner-walled cysts more care is needed. The entire cyst is removed intact
and should be sent for histological examination. If there is a non-vital tooth associated,
as in a radicular cyst, the teeth should endodontically treated. If there are apices of other
teeth extending into the cavity, these teeth are usually either root treated preoperatively
or on cyst removal by a retrograde approach. Alternatively, they may be extracted. The
edges of the bone cavity are smoothed off, free bleeding is controlled and the cavity is
irrigated to remove debris. The mucoperiosteal flap is replaced and sutured in place on
sound bone around the margin of the bony window. The cavity fills with blood and
organises. The sutures should be left for at least 10 days. Radiographic evidence of bone
fill will take 6 to 12 months (Fig. 24, Fig. 25).
Fig. 24-Removal of an apical cyst by flap reflection and creation of osseous window are
demonstrated at the time of tooth removal.
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
25
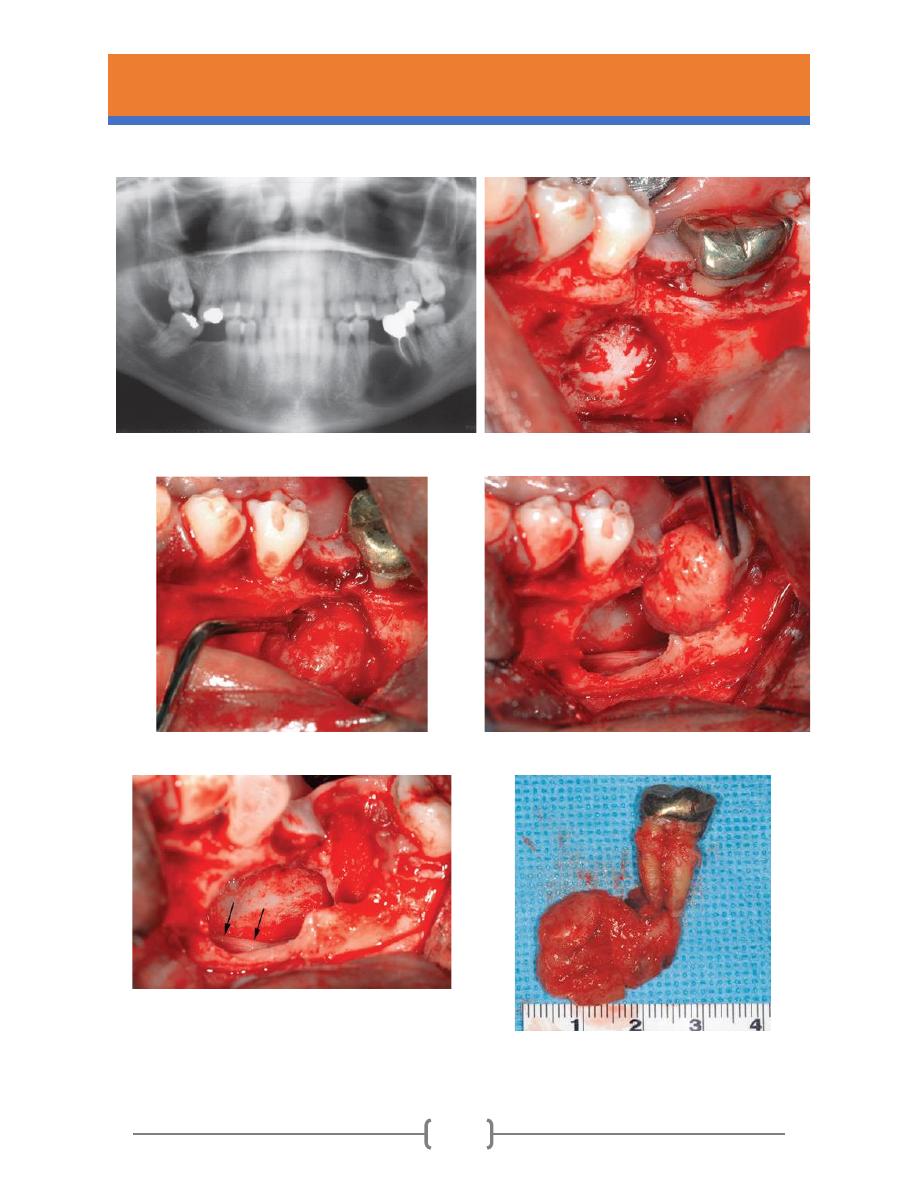
A
B
C
D
E

UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
26
F
G
Fig.
25- A clinical case of apical cystectomy
performed with tooth extraction. (A) Pretreatment
panoramic radiograph showing large radiolucent
lesion at the apices of teeth No. 18 and 20. (B)
Incision designed to ensure that the incisions are
located over intact bone after cystectomy. (C)
Appearance of the lesion after the buccal flap is
elevated. Note that the lesion has eroded the bone.
(D) Curette used to elevate the lesion from the bony
walls. (E) Cyst being removed. (F) Surgical specimen.
(G) When opened, the specimen appeared to be
cystic. The patient should be monitored with
periodic radiographs to ensure bone fill and no
recurrence of the lesion
.
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
27
2. Marsupialization
Marsupialization (decompression) refers to creating a surgical window in the wall of the cyst,
evacuating the contents of the cyst, and maintaining continuity between the cyst and the oral
cavity, maxillary sinus, or nasal cavity. The only portion of the cyst that is removed is the piece
removed to produce the window. The remaining cystic lining is left in situ. This process decreases
intracystic pressure and promotes shrinkage of the cyst and bone fill (Fig.26 and Fig 27).
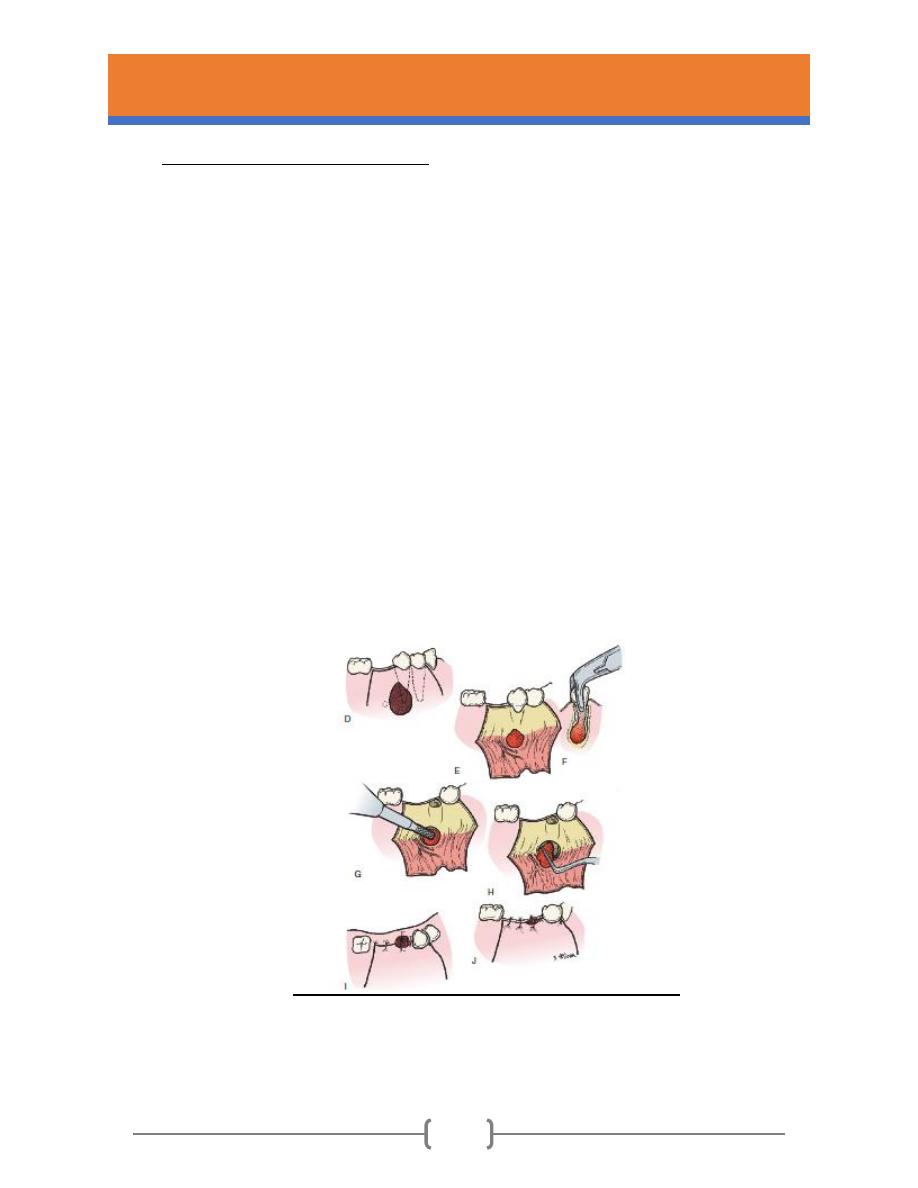
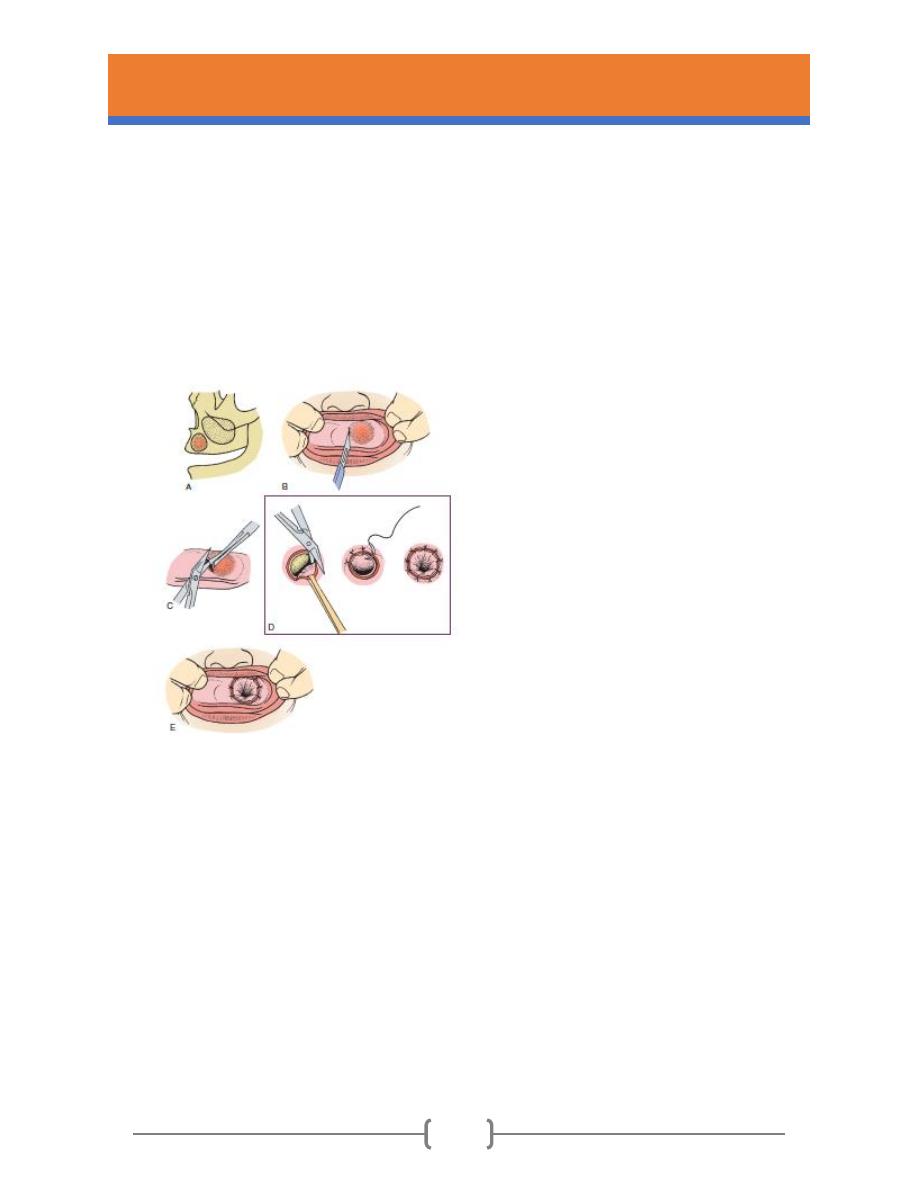
Fig. 26- Marsupialization technique. (A) Cyst
within the maxilla. Palpation of the mucosa
often reveals a compressible firmness,
indicating that the bone has been eroded. The
undersurface of the oral mucosa and the
undersurface of the cyst (fibrous) capsule will
therefore be fused together. (B) Incision
through the oral mucosa and cystic wall into the
center of the cyst. (C) Scissors are used to
complete excision of the window of mucosa
and cystic wall. This specimen is submitted for
pathologic examination. (D) Oral mucosa and
mucosa of the cystic wall sutured together
around the periphery of the opening. This
effectively “decompresses” the cyst, and it will
now shrink as new bone fills in the cystic cavity.
UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
28
A
B
C
D
E
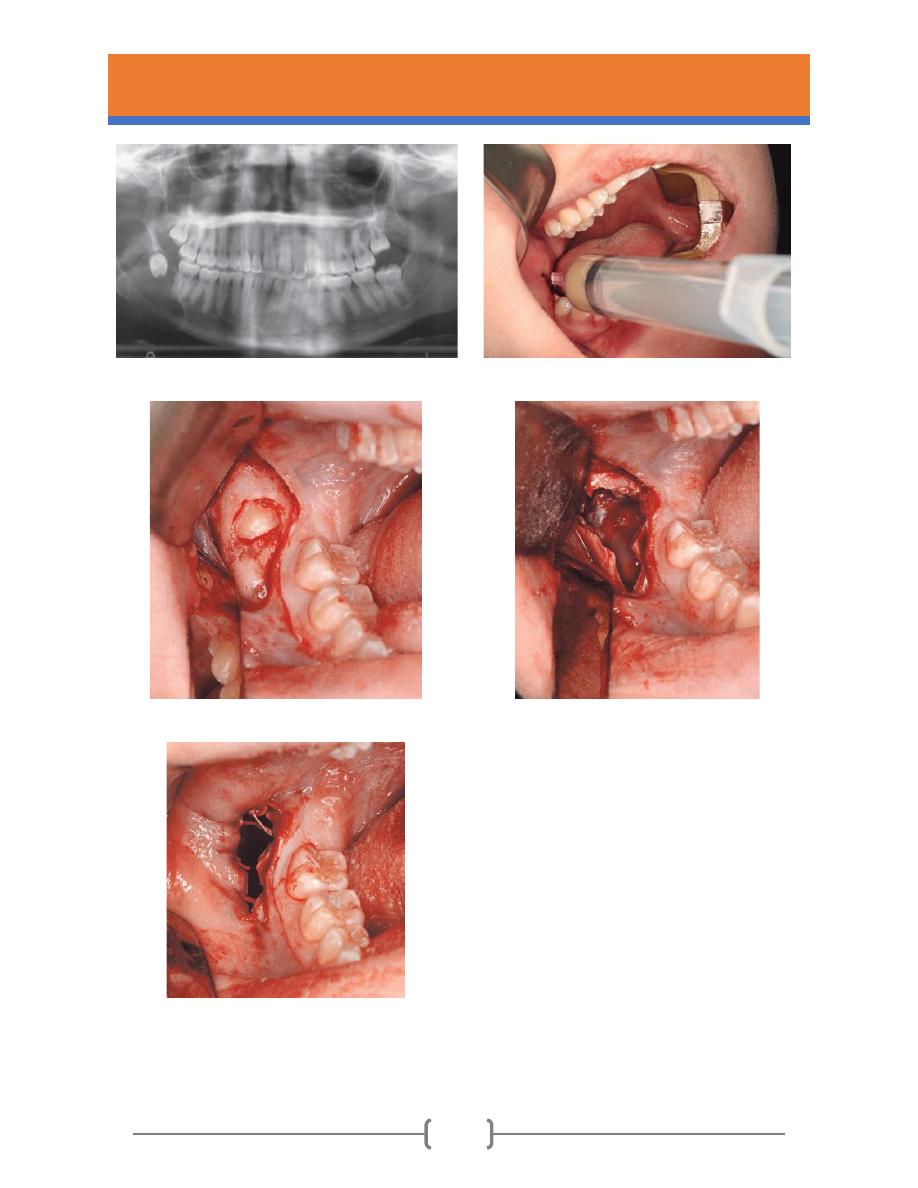
Fig. 27- Marsupialization of an odontogenic
keratocyst in the right mandible associated with an
impacted third molar. (A) Panoramic radiograph
showing a large multilocular radiolucent lesion
associated with tooth #32. (B) Aspiration of the lesion
reveals a creamy liquid (keratin). (C) Exposure and
removal of bone behind the second molar reveals the
impacted third molar crown. (D) The impacted tooth
was removed, as was additional bone to provide a
large window into the lesion. A portion of the lining
was excised and sent for pathologic examination. The
cavity was inspected through the opening to ensure
there was no solid mass that might indicate a tumor.
(E) Holes were drilled around the periphery of the
bony opening to pass sutures from the oral mucosa,
through the holes in the bone, and through the cyst
lining.

UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
29
➢ Indications
The following factors should be considered before deciding whether a cyst should be removed
by marsupialization:
1. Amount of tissue injury. Proximity of a cyst to vital structures can mean unnecessary sacrifice
of tissue if enucleation is used. For example, if enucleation of a cyst would create oronasal or
oroantral fistulae or cause injury to major neurovascular structures (e.g., the inferior alveolar
nerve) or devitalization of healthy teeth, marsupialization should be considered.
2. Surgical access. If access to all portions of the cyst is difficult, portions of the cystic wall may
be left behind, which could result in recurrence.
3. Assistance in eruption of teeth. If an unerupted tooth that is needed in the dental arch is
involved with the cyst (i.e., a dentigerous cyst), marsupialization may allow its continued eruption
into the oral cavity.
4. Extent of surgery. In a patient with ill health or any debilitation, marsupialization is a
reasonable alternative to enucleation because it is simple and may be less stressful for the
patient.
5. Size of cyst. In very large cysts, a risk of jaw fracture during enucleation is possible. It may be
better to perform marsupialization of the cyst and defer enucleation until after considerable
bone fill has occurred.
➢ Advantages of marsupialisation of cysts
1. Shrinkage before enucleation.
2. May allow preservation of teeth.

UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
30
3. Reduce the operative risk to inferior dental nerve.
4. Reduce the risk of mandibular fracture.
5. Shrinkage allows easier enucleation of residual cyst.
6. Enucleation may not be possible in a compromised patient.
➢ Possible disadvantages
1. Shrinkage is very slow, over weeks and months.
2. Tendency for the opening to shrink faster than the cavity.
3. Close follow up required. This means that the patient must irrigate the cavity several
times every day for several months. The patient may be inconvenienced in this respect.
4. Patient must keep the cavity clean.
5. The pathologic tissue is left in situ, without thorough histologic examination.
➢ Technique
The cyst is opened essentially as for enucleation, but the lining is left in place and sutured to the
oral mucous membrane at the margins of the opening to produce a wide communication into the
mouth. The aim is to decompress the cavity and make it into a pouch continuous with the oral
mucosa. The cavity gradually closes by ingrowth of bone from the periphery and replacement of
the lining epithelium by ingrowth of the oral epithelium. However, considerable aftercare is
needed to keep the cavity clean. The cavity is initially packed with ribbon gauze and, after the
margins have healed, a plug or extension to a denture is made to fill the opening.
Marsupialization is rarely used as the sole form of treatment for cysts. The main application of
marsupialisation is for temporary decompression of exceptionally large cysts where fracture of
the jaw is a risk. When the cyst has shrunk and enough new bone has formed, the remaining
lining can be enucleated.

UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
31
3. Enucleation After Marsupialization
Enucleation is frequently done (at a later date) after marsupialization thereby enucleation may
be undertaken without injury to adjacent structures. The combined approach reduces morbidity
and accelerates complete healing of the defect.
➢ Indications
The indications for this combined modality of surgical therapy are the same as those listed for
the technique of marsupialization.
➢ Advantages
The advantages of combined marsupialization and enucleation are the same as those listed for
marsupialization and enucleation. In the marsupialization phase, the advantage is that this is a
simple procedure that spares adjacent vital structures. In the enucleation phase, the entire lesion
becomes available for histologic examination. Another advantage is the development of a
thickened cystic lining, which makes the secondary enucleation an easier procedure.
➢ Disadvantages
The total cyst is not removed initially for pathologic examination. However, subsequent
enucleation may then detect any occult pathologic condition.
➢ Technique
First, marsupialization of the cyst takes place, and osseous healing is allowed to progress. Once
the cyst has decreased to a size that makes it amenable to complete surgical removal, enucleation
is performed as the definitive treatment. The appropriate time for enucleation is when bone is
covering adjacent vital structures, which prevents their injury during enucleation, and when
adequate bone fill has provided enough strength to the jaw to prevent fracture during
enucleation.
Once the cyst has been enucleated, the oral soft tissues must be closed over the defect, if

UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
32
possible, which may require the development and mobilization of soft tissue flaps that can be
advanced and sutured over the osseous window. If complete closure of the wound cannot be
achieved, packing the cavity with strip gauze impregnated with an antibiotic ointment is
acceptable. This packing must be changed repeatedly with cleansing of the cavity until
granulation tissue has obliterated the opening and epithelium has closed over the wound.
4. Enucleation with Curettage
Enucleation with curettage means that after enucleation a curette or burr is used to remove 1 to
2 mm of bone around the entire periphery of the cystic cavity. This is done to remove any
remaining epithelial cells that may be present in the periphery of the cystic wall or bony cavity.
These cells could proliferate into a recurrence of the cyst.
➢ Indications
1. Removing anodontogenic keratocyst because odontogenic keratocysts exhibit aggressive
clinical behavior and a considerably high rate of recurrence.
2. Any cyst that recurs after what was deemed a thorough removal.
➢ Advantages
If enucleation leaves epithelial remnants, curettage may remove them, thereby decreasing the
likelihood of recurrence.
➢ Disadvantages
Curettage is more destructive of adjacent bone and other tissues. The dental pulps may be
stripped of their neurovascular supply when curettage is performed close to the root tips.
Adjacent neurovascular bundles can be similarly damaged.
➢ Technique
After the cyst has been enucleated and removed, a sharp curette or a bone burr with sterile

UNIVERSITY OF MOSUL/COLLEGE OF DENTISTRY
ORAL AND MAXILLOFACIAL DEPARTMENT
LECTURER/ DR. THAFAR ALMELA/2020
33
irrigation can be used to remove a 1- to 2-mm of bone around the complete periphery of the
cystic cavity. The cavity is then cleansed and closed.
