Complications of tooth extraction
Soft tissue injuryExtraction of the wrong teeth
Fracture of the teeth during extraction
Fracture of tooth root during extraction
Fracture of the alveolus
Fracture of tuberosity
Displacement of the tooth in to the maxillary sinus
Creation of oroantral fistula
Fracture of mandible
Breakage of instrumentLuxation of adjacent tooth
Injury regional nerves
Swallowing of loss teeth
Dislocation of condyle
Failure to secure local anesthesia
1. Complications occurring during tooth extraction
2. Complications occurring after tooth extraction
Presence of bony spiculeHemorrhage
Dry socket
Infection
Truisms
Fainting during or after extraction
Respiratory arrest
Cardiac arrest.
Soft tissue injuries, Types and causes
AbrasionThese injuries are caused by careless use of rotary instruments
Thermal injuries
Caused when instruments taken out from autoclave or hot air oven are used immediately intraorally.
Mucosal tears
These are caused due to injudicious use of instruments, improper elevation of flap or the exercise of excessive force.
Prevention and Management
Take extreme care during the handling of the rotary or other hand instruments.Cool the instruments properly before using to prevent thermal injuries.
Mucosal tears can be prevented by proper designing and elevation of the flap, by proper handling of the flap and by gentle and effective manipulation of the elevators.
Properly retract the cheek and lips during dental procedures thus avoiding trauma from instruments.
If the tear or abrasion is large, suturing should be done for closure.
2. Extraction of the wrong teeth
Management
Inform the patient.
Replace the tooth inside the socket as soon as possible and splint it.If immediate replacement is not possible, place the tooth in a proper medium like saliva (the tooth can be held in the buccal vestibule), milk or water.
This is followed by treatment and follow up as for traumatic avulsion and reimplantation
3. Fracture of the teeth during extraction (including apposing teeth)
CausesApplication of the wrong forceps
Improper application of the forceps
Improper application of force
Extensively carious teeth
Endodontically treated teeth
Curved or ankylosed root.
Movement of patient
Prevention
Proper pre-radiographic assessment of the tooth.proper selection of instrument, proper application of the forceps proper application of the force.
Using transalveolar removal technique whenever intraalveolar extraction is not feasible.
Management
• When the fracture involves the crown of the tooth appropriate restoration should be placed.
• Incase of root fracture remove the tooth or root fragment completely whenever possible.
• In case of close proximity of a small root fragments (less than 5 mm) to the sinus or inferior alveolar nerve, leave the root as it is unless it is infected.
4. Fracture of tooth root during extraction
Causes
Improper technique
Application of incorrect instrument and force
Ankylosed teeth or hypercementosed teeth
Excessively curved roots
Endodontically treated teeth
Teeth with gross filling
Extensively carious teeth
Uncooperative patient
Consequences of retained roots
Retained roots may act as a source of infection.When large retained roots are lying in the submucosa just beneath the denture, the overlying mucosa constantly gets inflamed and may interfere with the proper functioning of the denture.
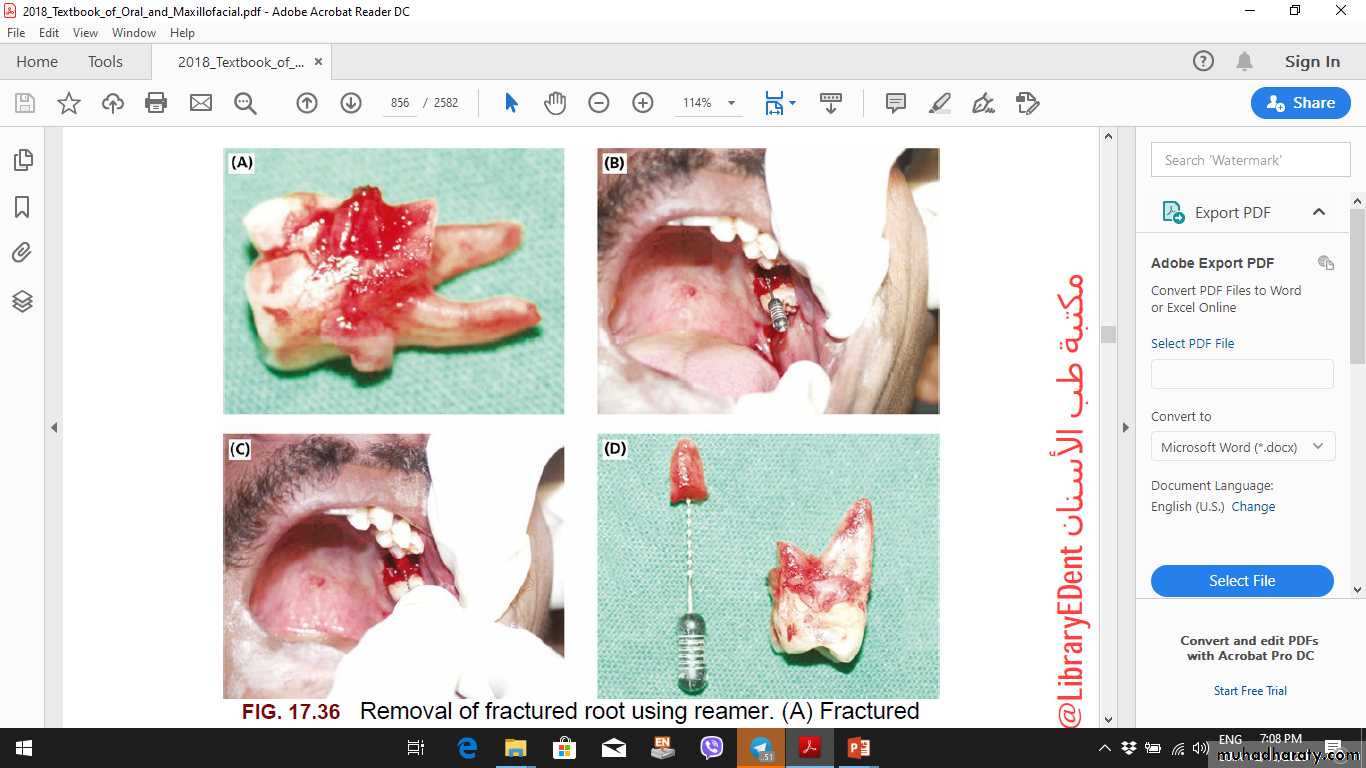
Methods for retrieval of fractured root
Root forceps
Elevator
Reamers
Transalveolar extraction
5. Fracture of the alveolus
Causes• Improper application of the instruments
• Application of excessive force
• Lack of support to the alveolus during extraction
• Brittle alveolar bone
• Ankylosed teeth
Prevention
• Proper radiographic assessment of the tooth and the surrounding alveolar structure.• Proper application of the forceps and elevators.
• Avoid exertion of excessive force.
• Support the alveolus properly during extraction.
Management
• When the bone fragment is completely detached from the periosteum it is advisable to remove it along with the teeth and suture the flap back.• When the bone is attached to the periosteum, it can be replaced back and the flap closed
6. Fracture of tuberosity
Causes
• where the antrum extends into the tuberosity, the extraction of third molar can result in fracture of the tuberosity.
• Exertion of excessive force application.
• Fusion of the roots of second molar with the unerupted third molar (concrescence)
• Divergent roots of the third molar or hypercementosed third molar.
Prevention
• Take radiographs before extraction to assess the condition of the third molar and surrounding structures.• Avoid the exertion of inadvertent force.
• Support the alveolus during extraction.
Management
• If the fractured segment is small, a mucoperiosteal flap is elevated and the tuberosity is removed along with the tooth, followed by wound closure.• If the fractured segment is large and the mucoperiosteal is attached to the bone, it should be replaced and splinted.
• Prescribe antibiotics, analgesics and nasal drops if the fracture involves the antrum.
• Removal of the tooth should be done after the healing of fractured site.
7. Displacement of the tooth into the maxillary sinus
Causesclose approximation of the teeth to the maxillary sinus.
the antral cavities may be large and may dip in between the apices of the posterior teeth or around edentulous area of isolated tooth.
With advancing age the degree of pneumatisation of the maxillary sinus increases and the antral walls become very thin. The roots of the posterior teeth are covered only by thin bone which fracture easily and result in the disappearance of the root tip during its removal.
the shape of the tooth (like the popping of an orange seed) once the extraction forceps are applied.
Prevention
Proper radiographs should be taken before the extraction to assess the proximity of the root tip to the sinus.
Support the jaw and the alveolus adequately before extraction
Management
• Confirm the presence and location of the tooth or root tip in the sinus using radiograph.
• Once the location is confirmed, keep a nozzle connected to a powerful suction device at the entrance of the fistula to recover the root.
• Pack along piece of roller gauze into the sinus through the opening and remove it with a jerk, the root tip or the tooth might sometimes be removed along with the gauze.
• If none of the aforementioned procedures solves the problem then Caldwell-Luc operation is carried out.
Causes
Close proximity of the posterior teeth to the sinus predisposes to an oroantral fistula during the extraction of these teeth.No or thin bone between roots and floor of sinus
Long divergent roots that during extraction piece of bone may come out with root and communication create.
Prevention
Preoperative radiograph.
Shifting to transalveolar extraction with sectioning of roots and avoid excessive apical force.
8. Creation of oroantral communication
Diagnosis:The diagnosis of an oroantral communication can be made in several ways.
The first is to examine the tooth once it has been removed.
If little or no bone adheres to the molars, a communication may exist anyway.
the nose-blowing test may confirm the presence of a communication. This test involves pinching the nostrils together to occlude the patient’s nose and asking the patient to blow gently through the nose while the surgeon observes the area of the tooth extraction. If a communication exists, there will be passage of air through the tooth socket and bubbling of blood in the socket area
Radiograph (P.A. view or water’s view)
Management
Depend on size of opening
If less than 2mm: seqweez the socket to stabilize high quality blood clot and instruct the patient to follow sinus precautions to prevent dislodgment of blood clot
Sinus precautions:
avoid blowing the nose,
avoid sneezing violently,
avoid sucking on straws,
avoid smoking
If the opening is moderate size (2 to 6 mm)
additional measures should be taken,a figure-of-eight suture should be placed over the tooth socket.
patient should also be told to follow sinus precautions.
Finally, the patient should be prescribed several medications to reduce the risk of maxillary sinusitis.
In addition, a decongestant nasal spray should be prescribed to shrink the nasal mucosa to maintain patency of the ostium.
If the sinus opening is large (≥7 mm),
the surgeon repaired the sinus opening with a flap procedure.
The most commonly used flap is the buccal flap. This technique mobilizes buccal soft tissue to cover the opening and provide for a primary closure. The same sinus precautions and medications are usually required
9. Fracture of mandible
Causes• Atrophic mandible as in old age
• Existence of any bony pathology
• Excessive/inadvertent force application
• In case of removal of vertically impacted third molar
Prevention and Management
• Proper preoperative assessment of the type of impaction and the density of the bone before extraction
• Proper support of the jaw during extraction
• Application of adequate force
• Inform and reassure the patient
10. Breakage of instruments
Causes
• Application of excessive force
• Improper technique
• Defect in manufacturing
• Old and worn out instruments
Prevention
• Proper selection of the instrument
• Proper handling and usage
Management
• Remove the burs or elevator tips with a hemostat if it is visible.
• If impacted deeply, surgical removal of the instrument is advised unless contraindicated as in close proximity to vital structures.
11. Luxation of adjacent tooth
Causes• Improper instrumentation
• No support to the adjacent structures during extraction
Prevention
• Proper technique and careful handling of the instruments
• Support the adjacent teeth adequately before extraction
Management
• Reposition the tooth inside the socket and splint it
• The tooth should be treated endodontically after 1 week.
The most frequently involved specific branches are the mental, lingual, buccal, and nasopalatine, inferior alveolar nerves.
1. The nasopalatine and buccal nerves are frequently sectioned during the creation of flaps for the removal of impacted teeth. The area of sensory innervation of these two nerves is relatively small, and reinnervation of the affected area usually occurs rapidly
2. when the mental nerve is injured, the patient will experience paresthesia or anesthesia of the lip and chin. If the injury is the result of flap reflection or manipulation, normal sensation usually returns in a few days to a few weeks. If the mental nerve is sectioned at its exit from the mental foramen or torn along its course, it is likely that mental nerve function will not return, and the patient will have a permanent state of anesthesia.
3. If a three-corner flap is to be used in the area of the mental nerve, the vertical releasing incision must be placed far enough anteriorly to avoid severing any portion of the mental nerve.
12. Injury to regional nerves nerve
Injury to Inferior alveolar nerve
may be traumatized along the course of its intrabony canal. The most common place of injury is the area of the mandibular third molar.Removal of impacted third molars may bruise, crush, or sharply injure the nerve in its canal.
This complication is common enough during extraction of third molars that it is important routinely to inform patients preoperatively that it is a possibility.
The surgeon must then take every precaution possible to avoid injuring the nerve during the extraction.
Injury to lingual nerve
• The nerve may be damaged during the removal of the third molar when the lingual cortex fractures.• There is a risk of damage during the elevation of the lingual mucoperiosteum.
Prevention
Proper technique and careful manipulation of the instruments.
incisions made for surgical exposure of impacted third molars or of bony areas in the posterior molar region should be made well to the buccal aspect of the mandible.
Prevention of injury to the lingual nerve is of paramount importance to avoid this problematic complication.
13. Swallowing of extracted tooth
Causes• Careless handling of the instruments
• Improper technique
Management
• Check for breathing difficulty.
• Check for dislodgement of teeth in pyriform fossa by radiograph/indirect laryngoscopy.
• Confirm the presence of teeth in the GIT.
• Prescribe laxatives.
• Confirm the expulsion of the tooth using serial radiographs
14. Dislocation of condyle (uni or Bi )
Causes• Exertion of excessive force
• Failure to support the mandible adequately during extraction
• Number of previous episodes of dislocation
Prevention
• Proper exertion of adequate force
• Support the mandible during extraction
Management
• Take a radiograph of the area.
• If the condyle is dislocated into the middle cranial fossa, refer to an oral surgeon.
• Manual reduction of anterior displacement of the condyle requires downward pressure on the retro-molar region and simultaneous upward pressure on the chin.
15-Failure to secure anesthesia:-
a-Faulty technique...DUE TO Incorrect technique or insufficient amount of L.A.
b-The use of expired date L.A. agent
c-Individual variation such as anatomical or physiological variation ( high pain reaction and low pain threshold ).
d-Presence of acute infection.
Complications occurring after the surgical
procedure1. Presence of bony spicule
Cause
Improper and careless technique of extraction.
Prevention
Checking the socket for any sharp edges before closure.
Management
removal of the bony spicule.
2. Excessive hemorrhage
Causes(a) Patient with a history of bleeding (During a pervious extraction, A family history of bleeding, A history of previous post-extraction hemorrhage.)
(b) Use of plain local anesthesia (without vasoconstrictors).
(c) Placement of insufficient pieces of cotton on the socket.
(d) Continuous change of the socket pack.
Bleeding may occur during, after or later the extraction. Reactionary hemorrhage occurs within 48 hours of the operation when local rise in blood pressure may force open divided vessels which are insecurely sealed by natural or artificial means. This is common in patients treated with local anesthesia when the effects of the vasoconstrictor beings to wear off . Secondary hemorrhage is caused by infection which destroys the blood clot or the ulceration of the vessel wall. This type starts 7 days after operation usually with a mild oozing. This can be arrested by local measures and antibacterial drugs are prescribed to combat the infection.
Methods to control bleeding
a) Packing: severe bleeding can be controlled by pressure on a hot normal saline pack held in position for 15 minuets.b) Digital pressure: this is useful for capillary or venous bleeding and as immediate measures when large vessels have been cut.
c) Haemostatic agents like tannic acid, adrenaline, gel foam, bone wax; topical thrombin can be placed into the socket.
d) Electro cauterization: this may be applied directly to the vessels or by passing current through artery forceps clamping the vessels.
e) Direct ligation of the vessels.
f) Suturing: simple interrupted or horizontal mattress sutures should be inserted across the socket as soon as possible.
3. Dry Socket
It is defined as an acute localized alveolitis involving either the whole or part of condensed bone (lamina dura) lining a tooth socket. It is characterized by a deeply seated pain which begins about 2-4 days following extraction and is associated with denuded bone and a broke down blood clot. It is of an unknown etiology but the predisposing factors may include:a) Infection of the socket occurring either before, during or after the extraction.
b) The use of excessive force during extraction.c) The use of large or high concentration if the adrenaline in the local anesthetic solution especially in the mandible.
d) After radiotherapy due to endarteritis obliterans of the blood vessels leading to decreased blood supply.
e) Pregnant women and also those taken oral contraceptive
f) Mechanical dislodgment of clot due to vigorous mouth washing.
Prevention of Dry Socket :
a) The patient should rinse his mouth with 0.5% Chlorohexidine before the administration of local anesthetic agents.
b) Only the minimal amount of local anesthetic solution necessary should be administrated.
c) Avoid traumatic extraction as much as possible.
Treatment of dry socket:
If dry socket occurs the aim of the treatment should be to relief pain and to promote healing.a) The socket should be irrigated with warm saline and all degenerated blood removed.
b) Sharp bony spicules should be removed with bone rongeurs or smoothed with bone file.
c) A loose dressing of zinc oxide euginol or iodoform pack is tucked into the socket. The apex should not be placed tightly or deeply into the socket as it may set hard and will be difficult to remove and will interfere with healing.
d) Analgesics and antibiotics are prescribes with careful warm saline mouth baths and an appointment is made for follow up in 3 days time.
e) Prophylactic administration of metronidazol (flagyl) in a dose of 200mg/3 times daily for at least 3-5 days starting on the day of extraction appears to reduce the incidence of dry socket. Amoxil Caps. 250mg are also prescribed.
4. Infection
Infection can be treated by:a) The use of frequent intraoral hot saline mouthwashes.
b) Do not apply heat extraorally; this increases the size of the facial oedema.
c) If pus is present, it should be removed.
d) Administration of adequate antibodies and analgesics.
5. Trismus: It is defined as the inability of the patient to open the mouth due to muscle spasm and it is caused by:
a. Postoperative oedema, hematoma formation, and inflammation of the soft tissues like the medial pterygoid muscle.
b. Traumatic arthritis of the TMJ.
c. Following mandibular block injection.
Treatment:
a) Intraoral hot saline mouth wash.
b) Antibiotic administration.
c) Jaw exercise.
d) Muscle relaxant.
e) Non-steroidal Anti-inflammatory Drugs (NSAI D) for e.g. (ponstan caps., Brufen tabs.,…etc.)
6. Fainting during or after tooth extraction: Is a simple vasovagal attack (Syncope), the patient feels dizzy, weak, nauseated with the skin becoming pale, cold and sweating.
Treatment:
a) The dental chair should be made in a supine position by lowering the back of the dental chair with the legs slightly above the level of the head (Header Berge position). In case of pregnant women; the patient is placed in a semi supine position or is rolled to her left side.
b) Any tight collar or belt should be loosened.
c) Adequate ventilation should be available, stimulators as perfumes can be used.
d) Once consciousness returns a glucose drink is administered.
e) If recovery does not occur within a few minutes, Oxygen should be given and medical aid should be called immediately.
7. Respiratory arrest:
Although it is a rare complication but every dentist should be ready to deal with such a complication. The skeletal muscles become flaccid and the pupils become dilated.Management is aimed to maintain airway by:
a. The patient should be laid flat on the floor.b. The patient air-way should be cleared for any foreign bodies, appliances…etc.
c. Pull the mandible upward and forward to extent the head fully.
d. The patient nostrils should be compressed between the operating fingers and thumb, and then mouth to mouth artificial respiration should be performed so that the chest is seen to rise every 3-4 seconds. Medical aid should be called.
8. Cardiac arrest:
Cardiac arrest can lead to irreversible brain damage within 3 minutes due to the cerebral anoxia.
Diagnosis:
a. Patient becomes pallor and skin is covered with a cold sweat.
b. Loss of heart beats, pulses and pupils become dilated.
Management:
a. The patient is laid flat on his back on the floor.
b. The dentist places his left hand on the lower third of the patient's sternum and then places his right hand over the dorsum of his left hand. Both hands are pressed rhythmically at one second intervals with sufficient force to compress the heart between the sternum and vertebral column until the patient starts beating again.