Radiographic Interpretation
Image InterpretationImage interpretation is an explanation of what is viewed on a dental image, or the ability to read what is revealed by a dental radiographic image.
Image interpretation is an important component of patient care and enables the dental professional to detect diseases, lesions, and conditions that cannot be identified clinically.
Visual search strategies
Analytic or systematic strategy; this approach relies on a step-by-step analysis of all the imaging features of an abnormal finding so that a diagnosis can be made based on these findings. This analytic process is believed to reduce bias and premature closure of the decision-making process.
Non analytic approach; this approach suggests that the clinician makes an automatic decision regarding the diagnosis without thorough feature analysis of the image
Analytic of Systematic Strategy
STEP 1: LOCALIZE ABNORMALITY
Localized or Generalized
Generalized disease mechanisms an abnormal appearance affects all the osseous structures of the maxillofacial region, such as metabolic or endocrine abnormalities of bone.
Localized, may be unilateral or bilateral. Variations of normal anatomy are more commonly bilateral. For instance, a bilateral mandibular radiolucency may indicate normal anatomy, such as extensive submandibular gland fossa. Abnormal conditions are more commonly unilateral. For instance, fibrous dysplasia commonly is unilateral.
A few abnormalities, such as Paget’s disease and cherubism, are always seen bilaterally in the jaws.
Position in the Jaws
To determines the epicenter
Some lesions tend to be found in specific locations.
Determining the epicenter of the lesion or the point of origin assists in indicating the tissue types that compose the abnormality for example:
If the epicenter is coronal to a tooth, the lesion probably is composed of odontogenic epithelium
If it is above the inferior alveolar nerve canal (IAC), the likelihood is greater that it is composed of odontogenic tissue.
If the epicenter is below the IAC, it is unlikely to be odontogenic in origin
If it originates within the IAC, the tissue of origin probably is neural or vascular in nature
The probability of cartilaginous lesions and osteochondromas occurring is greater in the condylar region.
If the epicenter is within the maxillary antrum, the lesion is not of odontogenic tissue, as opposed to a lesion that has grown into the antrum from the alveolar process of the maxilla
The other reason to establish the exact location of the lesion is that particular abnormalities tend to be found in very specific locations. Following are a few examples of this observation:
The epicenters of central giant cell granulomas commonly are located anterior to the first molars in the mandible and anterior to the cuspid in the maxilla in young patients.
Osteomyelitis occurs in the mandible and rarely in the maxilla.
Periapical osseous dysplasia (periapical cemental dysplasia) occurs in the periapical region of teeth
Single or Multifocal
Establishing whether an abnormality is solitary or multifocal aids in understanding the disease mechanism of the abnormality. Additionally, the list of possible multifocal abnormalities in the jaws is relatively short. Examples of lesions that can be multifocal in the jaws are periapical cemental dysplasia, keratocystic odontogenic tumors, metastatic lesions, multiple myeloma and leukemic infiltrates.
Size
There are very few size restrictions for a particular lesion, but the size may aid in the differential diagnosis. For instance, when differentiating between a dentigerous cyst and a hyperplastic follicle surrounding the coronal portion of a tooth, size may be considered a determining factor. Because dentigerous cysts have growth potential, they are often much larger than a hyperplastic follicle.Step 2: Assess Periphery and Shape
A well-defined lesion is one in which most of the periphery is well defined. If an imaginary pencil can be used to draw confidently the limits of the lesion, the margin is well defined.
Ill-defined periphery difficult to draw an exact delineation around most of lesion.
Well-Defined Borders
1-Punched-Out Border. A punched-out border is one that has a sharp boundary there is no bone reaction apparent immediately adjacent to the abnormality.2-Corticated Border. A corticated margin is a thin, fairly uniform radiopaque line of reactive bone at the periphery of a lesion. This is commonly seen with cysts and benign slow-growing tumors
3-Sclerotic Margin. A sclerotic margin made up of a thick radiopaque border of reactive bone that usually is not uniform in width. This margin may be seen with periapical osseous dysplasia and may indicate a very slow rate of growth or the potential for the lesion to stimulate the production of surrounding bone
4-Soft Tissue Capsule. A radiopaque lesion may have a soft tissue capsule, which is indicated by the presence of a radiolucent line at the periphery. This soft tissue capsule may be seen in conjunction with a corticated periphery, as is observed with odontomas and cementoblastomas
Ill-Defined Borders
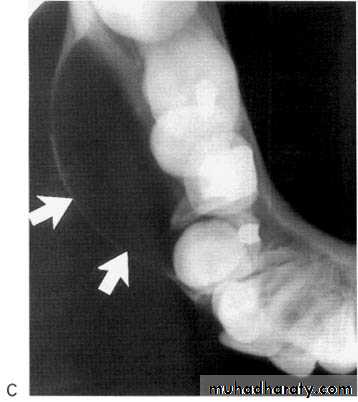
1-Blending Border. A blending border is a gradual, often wide zone of transition between the adjacent normal bone trabeculae and the abnormal-appearing trabeculae of the lesion. The focus of this observation is on the trabeculae and not on the radiolucent marrow spaces. Examples of conditions with this type of margin are condensing osteitis and fibrous dysplasia.2-Invasive Border. An ill-defined invasive border appears as an area of radiolucency with few or no trabeculae representing bone destruction just behind the lesion. The focus of this observation is on the enlarging radiolucency at the expense of bone trabeculae. Invasive borders are usually associated with rapid growth and can be seen with malignant lesions.
Shape
1-Circular or fluid-filled shape, is characteristic of a cyst.2-Scalloped shape is a series of contiguous arcs or semicircles that may reflect the mechanism of growth. This shape may be seen in cysts (e.g., keratocystic odontogenic tumors), cyst like lesions (e.g., simple bone cysts), and some tumors. Occasionally, a lesion with a scalloped periphery is referred to as multilocular.
Step 3: Analyze Internal Structure
The internal appearance of a lesion can be classified into one of three basic categories: totally radiolucent, totally radiopaque, or mixed radiolucent and radiopaque (mixed density).Step 4: Analyze Effects of Lesion on Surrounding Structures Teeth
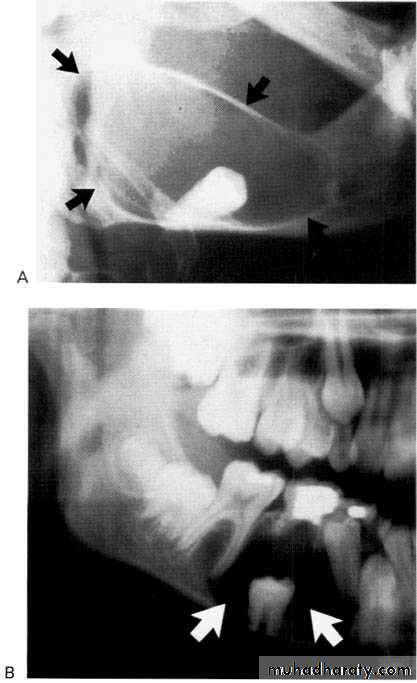
Displacement of teeth is seen more commonly with slower growing, space-occupying lesions.Lesions with an epicenter above the crown of a tooth (i.e., follicular cysts and occasionally odontomas) displace the tooth apically.
Cherubism originates and grows in the mandibular ramus, it has a propensity to push molars in an anterior direction.
Some lesions (e.g., lymphoma, leukemia, Langerhans’ cell histiocytosis) grow in the papilla of developing teeth and may push the developing tooth in a coronal direction
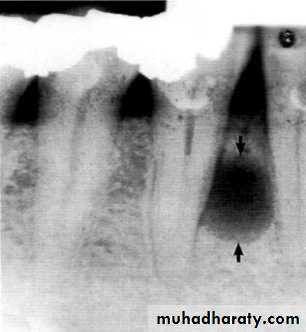
Widening of the periodontal membrane space
It is important to observe whether the widening is uniform or irregular and whether the lamina dura is still present. For instance, orthodontic movement of teeth results in widening of the periodontal membrane space, but the lamina dura remains intact. Malignant lesions can quickly grow down the ligament space, resulting in an irregular widening and destruction of the lamina duraSurrounding Bone Reaction
The presence of reactive bone at the periphery of a lesion whether corticated or sclerotic usually signifies slow benign growth and ability to stimulate osteoblastic activity in the surrounding bone
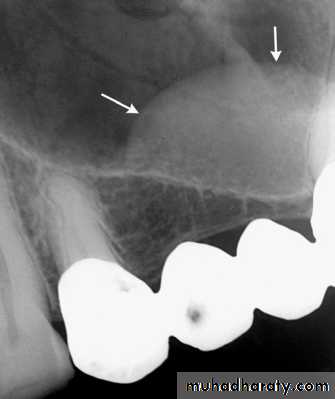
Inferior Alveolar Nerve Canal and Mental Foramen
Superior displacement of the inferior alveolar canal is strongly associated with fibrous dysplasia. Widening of the inferior alveolar canal with the maintenance of a cortical boundary may indicate the presence of a benign lesion of vascular or neural origin within the canal. Irregular widening with cortical destruction may indicate the presence of a malignant neoplasm growing down the length of the canal.