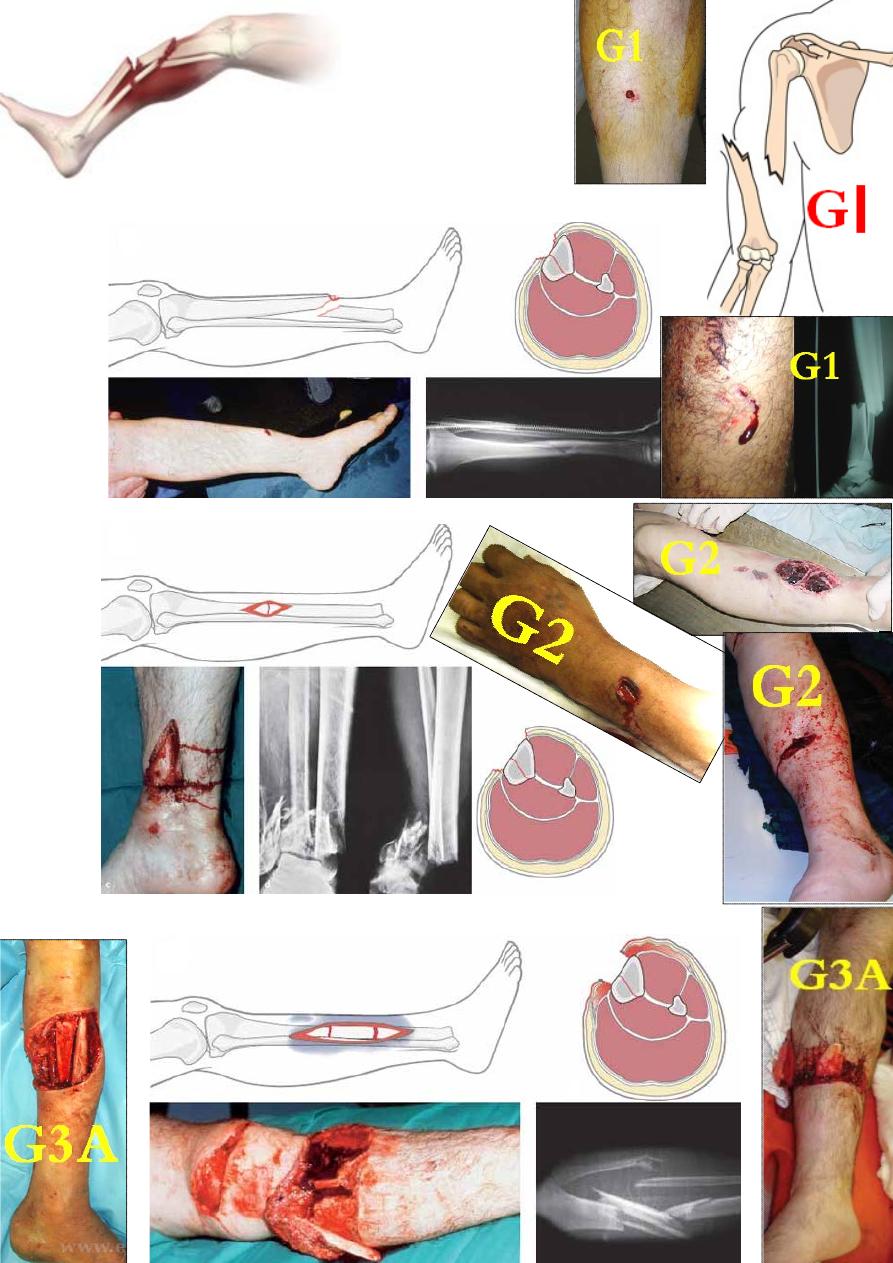
Compound fracture
Compound # are classified according to the severity of
tissue destruction into 3 types (Gustilo classification):
G
І- the wound is small, clean &usually
caused by bone spike (compound
from within).
G
І
G
П - the wound is >1cm with moderate
tissue damage (bone & soft tissue).
G
П
G
Ш- there is extensive skin, soft tissue, bone & neurovascular damage
with considerable contamination:
G
ШA- If the fracture can be covered by
soft tissue.
G
ШA
G
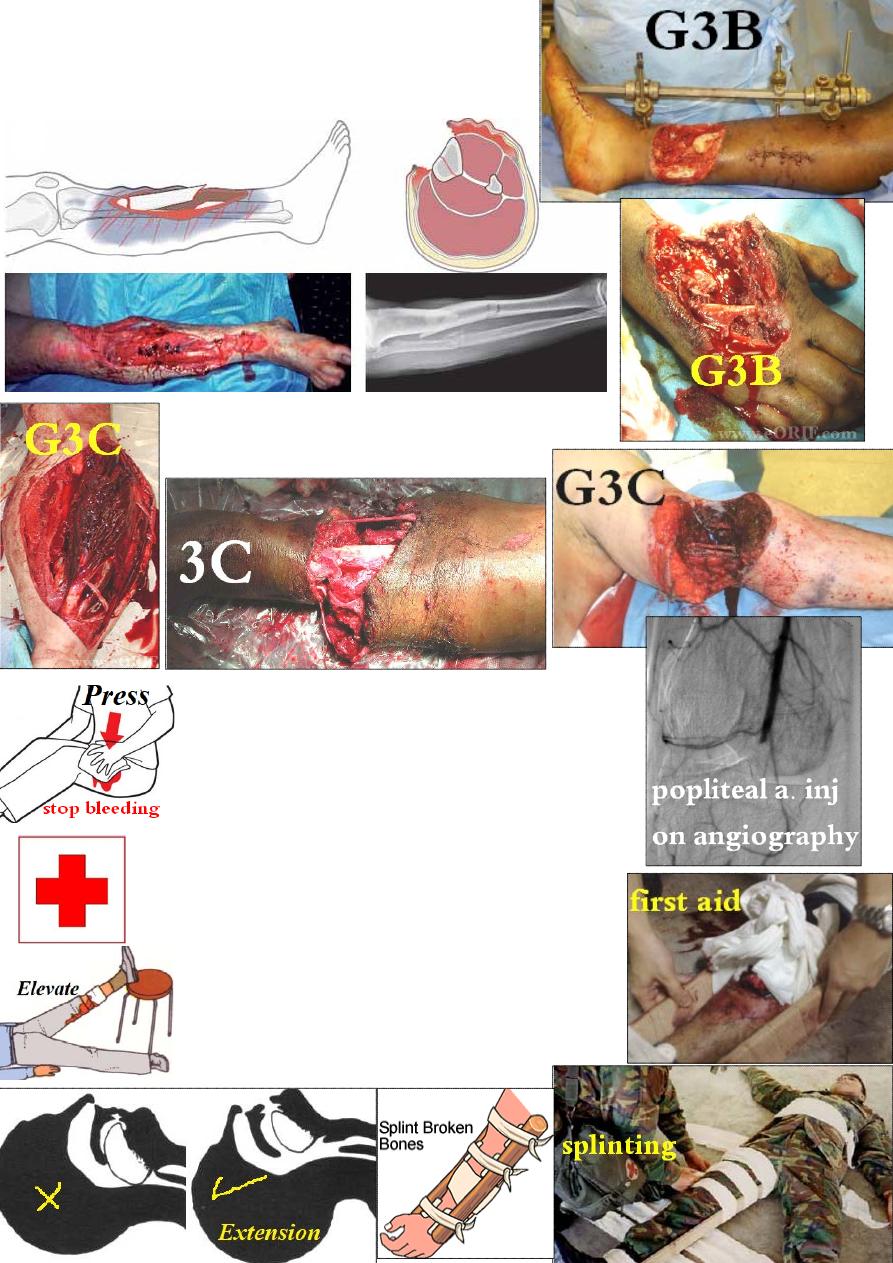
Ш B- If the # require
reconstructive surgery
for coverage.
G3B
G
Ш C- If there is arterial injury requiring repair
even if there is little tissue damage.
Management:
open fracture is an emergency.
At the scene: ensure clean airway, stop bleeding,
cover the wound, splint the # &transfer to hospital.
In the hospital: in the emergency room re-examine the
patient quickly then start resuscitation with IV line and
take blood sample for cross match.
The priority of
Ŗ should be for: Airway, Breathing &
Circulation then do further assessment checking the
level of consciousness, neck, back, abdomen, pelvis
and the limbs for wounds & #. After that, when the
patient is resuscitated and become more stable, you
can do more careful examination followed by the
required investigations including x-rays.

Local Ŗ of open fracture: start immediately
with broad spectrum AB &tetanus prophylaxis.
In the theater: clean the limb with soap &water, shave the skin
around the wound & sterilize it with antiseptic like chlorhexidine
or povidone iodine; then expose the wound and clean it with
physiological saline mixed with antibacterial agent several times.
Then start debridement:
Skin: only dead edges are excised till get healthy oozing skin.
Subcutaneous tissue: excise all dead subcutaneous tissues.
Muscles: all dead muscles should be excised bec. they are good
food for bacteria. A dead muscle is bluish in color (not red),
does not contract if pinched and if cut it will not bleed.
Bone: bone ends are cleaned, bone fragments are not removed
unless they are small and totally detached. Then do stabilize
the # with external fixator.
Blood vessels: large vessels are repaired, while small bleeders are ligated or clamped.
Nerves: approximate the nerve ends with sutures for later repair.
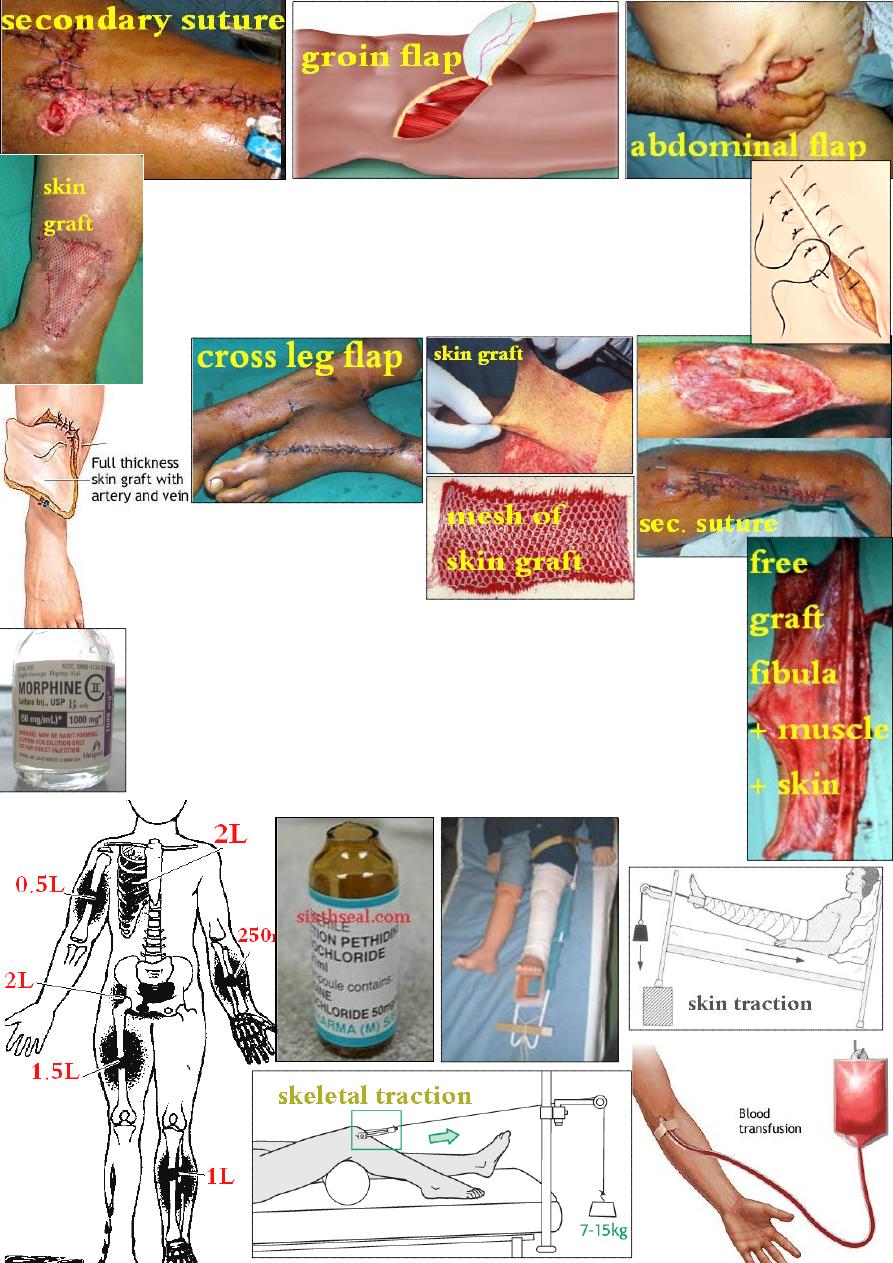
Wound closure: if the wound is small, clean and debrided within
few hours, you can close it, otherwise the wound should be left open
for daily dressing until it become clean with healthy granulation tissue
growth, then close it (secondary suture). Skin loss can be replaced by
skin graft (partial or full thickness), pedicle graft or free graft
(cutaneous, myocutaneous or osteomyocutaneous).
Complications of fracture
General complications
1- shock: is a generalized state of reduced tissue perfusion which if
persist, it will cause damage to vital organs. In # , the shock can be:
Neurogenic shock: due to pain, the blood will pool in the skeletal
muscles.
Ŗ→ splint the # & give anaelgesia like morphine or pethidine.
Hypovolemic shock: is due to blood loss from bone ends, nearby soft
tissue &injured blood vessels e.g. in a simple femoral shaft #, there may
be 1- 1.5 liter of blood lost into the soft tissue of the thigh outside the
circulation.
Ŗ → arrest the bleeding & restore the lost blood.
2
-
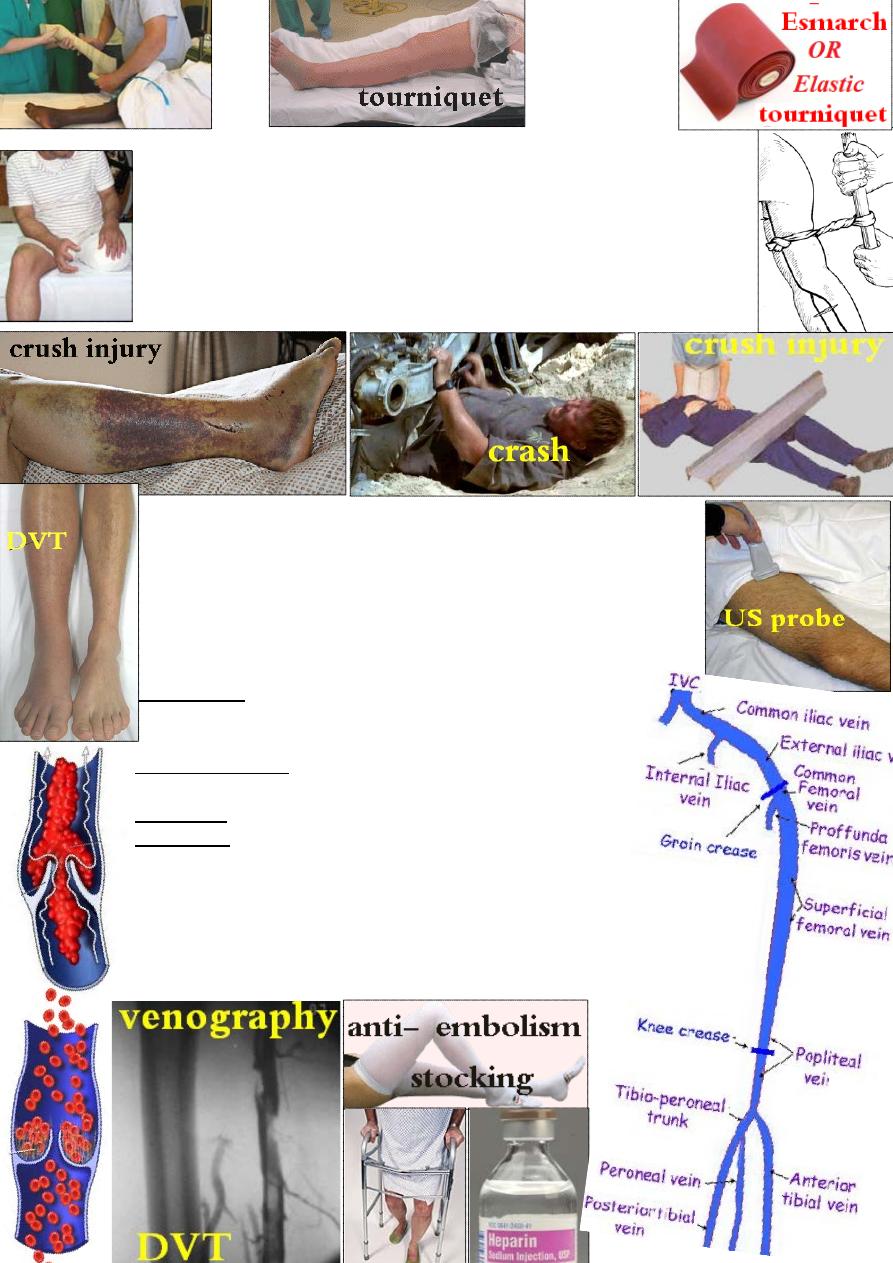
crush syndrome: may occur if a large bulk of muscles is crushed
or if a tourniquet has been left unreleased for > 6 hrs. After release, the
acid myohaematin (cytochrome C), resulting from muscle breakdown,
will be released into circulation &may block renal tubules or cause renal
artery spasm, both may lead to acute renal failure. So to avoid that, the
limb should be amputated above the level of the forgotten tourniquet &
before releasing it.
Ŗ of renal failure: ↓fluid &protein, ↑carbohydrate
intake, maintain electrolyte balance. Renal dialysis may be needed.
3- Venous thrombosis & Pulmonary embolism: incidence of
DVT after major trauma or surgery is 30% & that of PE is 5%
Causes of DVT: 1- Activation of factor 10 by thromboplastine
released from tissue damage. 2- Blood stasis. 3- Endothelial
damage.4- Increase number &stickiness of platelets.
Risk factors: 1- old patients. 2- cardiovascular disease.
3- Bed ridden patients. 4- hip surgery.
on &exercise of the patient.
arly mobilizati
E
-
: 1
Prevention
2- Elevation of affected limb. 3- Elastic bandage to prevent
blood pooling. 4- Anticoagulants like aspirin or heparin.
in body
ly there will be slight ↑
clinical
:
DVT
Established
temperature and pulse rate with swollen tender calf.
: venography or ultrasound scaning.
Diagnosis
of extensive DVT especially in thigh and pelvis:
Treatment
1-bed rest. 2-heparin IV 10 000 IU 6 hourly for 5-7 days or
according to partial thromboplastin time ( 1.5- 2 of the normal),
then shift to warfarin with the dose according to prothrombine
time for 3 months.
Pulmonary embolism: if massive, will cause sudden death.
If small, it may cause chest pain, dyspnea and haemoptysis.
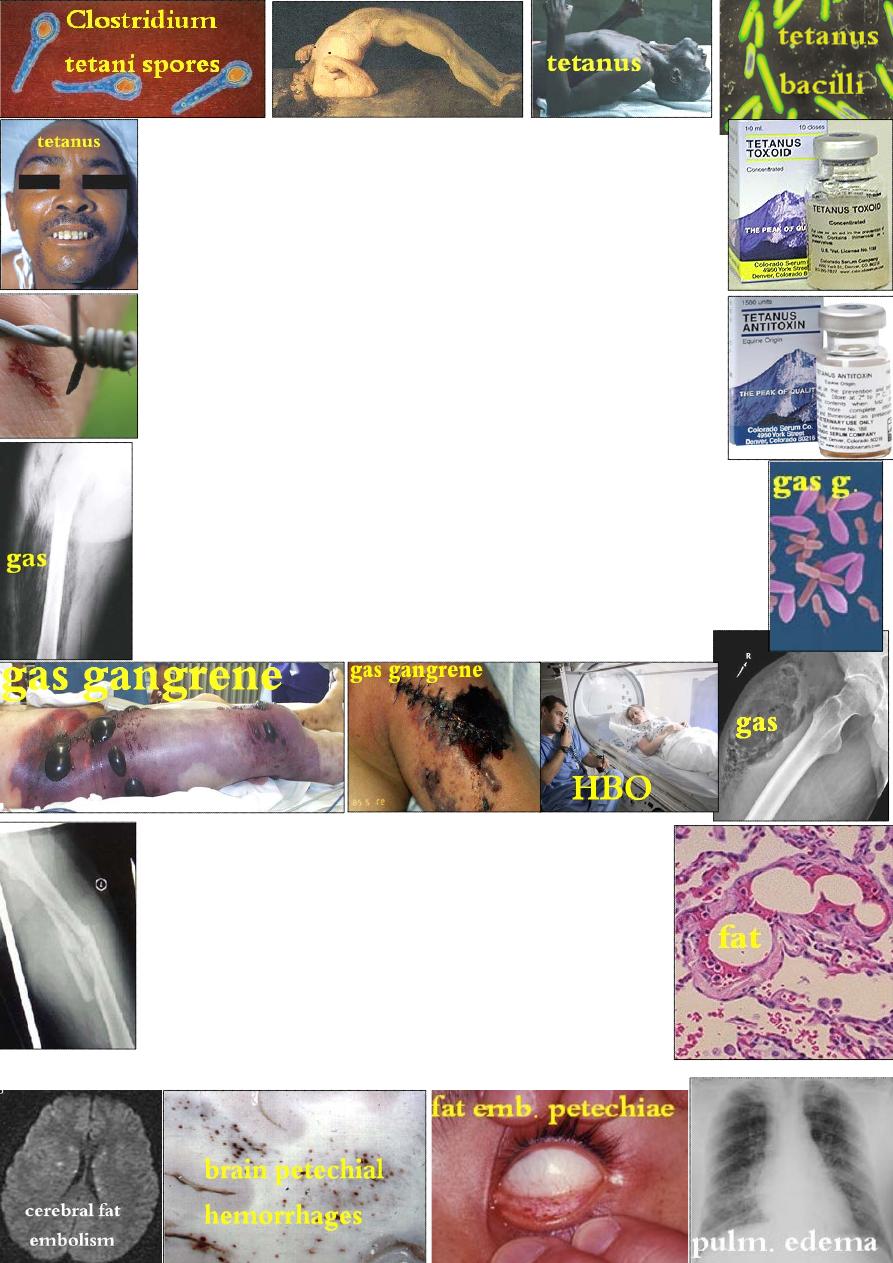
4- Tetanus: tetanus organism require dead tissue to grow, so good
debridement is important in prevention. The exotoxin is carried to
the CNS via blood and lymphatics. Once it reach the anterior horn
cells, it will be fixed there and can not be neutralized by antitoxin.
CF: early tonic and later clonic muscle contraction, especially of the
jaw, face, those near the wound &later, those of the neck & back.
If the diaphragm and intercostal muscles are affected, the patient
may die because of asphyxia.
Prophylaxis: good wound toilet, active immunization using
toxoid &booster dose after injury (those who were not immunized,
are human antitoxin serum).
Ŗ of established tetanus: IV antitoxin, sedation, muscle relaxant
(diazepam), AB (penicillin) &if required, assisted ventilation.
5- Gas gangrene: caused by Clostridia perfringens(welchii), anaerobic
gram +ve rods growing only in tissue with low oxygen tension, so the
usual site is dirty wound with dead muscle that has been closed with
inadequate debridement. Clinically, within 24 hrs, the wound become
swollen, painful, brown discharge with specific smell, gas in the tissue,
rapid pulse, little fever and later, the patient may become toxic and
comatose.
Ŗ: excision of all dead tissue, IV AB, hyperbaric oxygen may
limit infection. In severe cases, amputation may required.
6- Fat embolism: is thought to be due to liberation into the
circulation
of fat globules larger than 10μm, the aggregation
of them may obstruct capillaries especially in the lungs.
CF: usually, a young adult, within 72 hrs from injury, gets
slight fever, rapid pulse, dyspnea, confusion, skin petechiae
and in severe cases, respiratory distress and coma.
Diagnosis: is suspected if blood Po
2
is < 60 mmHg.
Ŗ→ assisted ventilation, fluid balance, heparin to prevent
thromboembolism & steroid to ↓ pulmonary edaema.
7- Fever: absorption of #
haematoma may ↑body temp by 0.5˚C.
