
Principles of fracture
Definition: a fracture is a break in structural continuity of bone. If the
overlying skin remains intact, the fracture is simple or closed fracture. If
not, it is open or compound fracture, i.e. there is connection between the
fracture haematoma and the atmosphere or one of the body cavities, so
liable to contamination and infection.
How fracture happen?
The cause is trauma which may be:
1-Single trauma like fall or road accident.
2-Repetitive stress like March fracture in solders (stress fracture).
3-Minor trauma or even normal stress can cause fracture if the bone
is already weakened by some pathology e.g. secondary deposit
(pathological fracture).
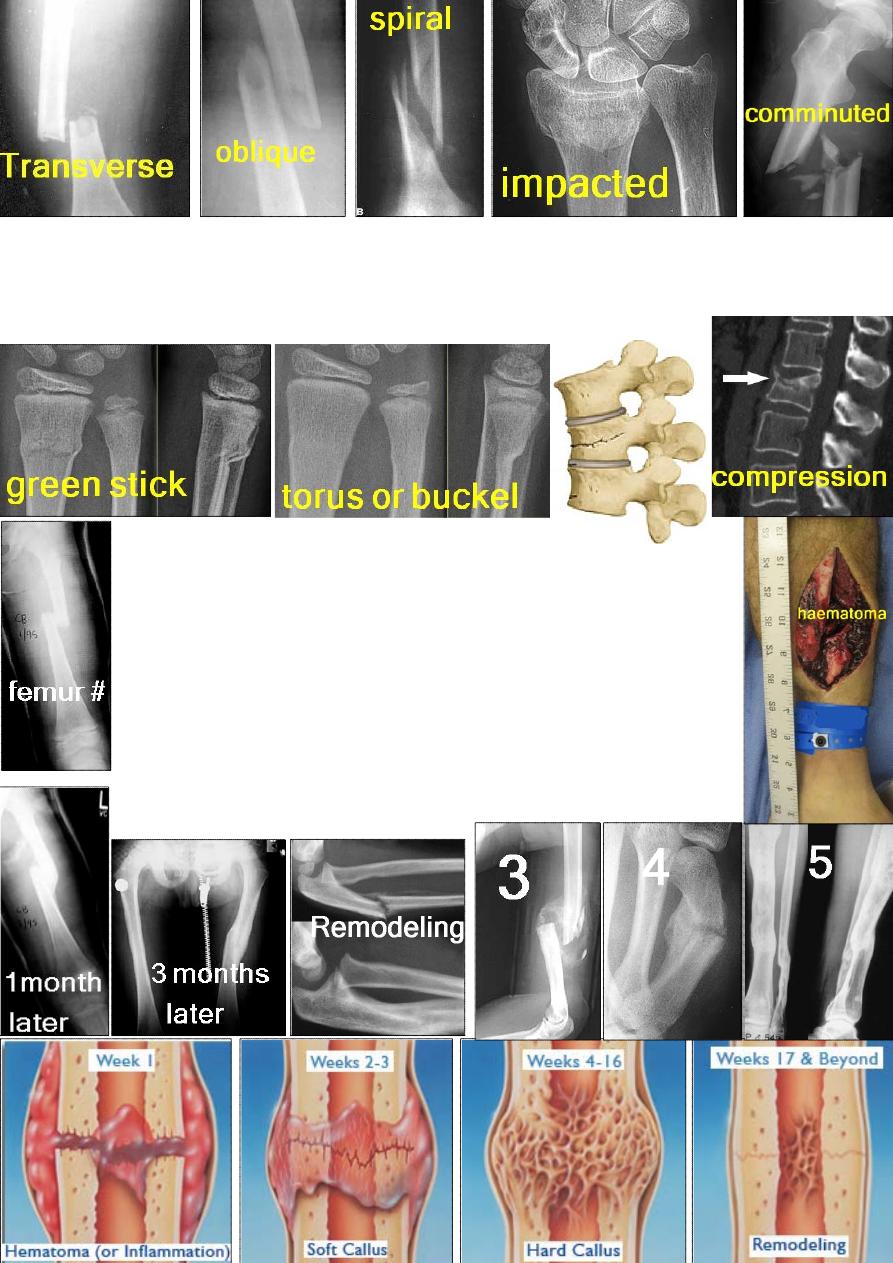
Types of fractures:
1- Complete fracture: may be transverse, oblique, spiral, impacted (the two
fragments are driven together)or comminuted fracture (> 2 fragments).
2- Incomplete fracture: only one side of the cortex is fractured like green
stick # in children and incomplete vertebral body fracture in adult.
How fractures heal?
Five stages:
1-Tissue injury and haematoma formation as a result of trauma.
2-Inflammation: after 8 hours the cells at bone ends will die
→ acute
inflammatory reaction with cellular proliferation under the periosteum &
inside the medullary canal with growth of new blood vessels. This
cellular tissue will bridge the bone ends.
3-Callus formation: now the proliferating cells will differentiate into
bone and cartilage cells, and these with time will form the callus which
is immature bone.
4-Consolidation: in this stage the immature bone will be changed by
bone cells into mature lamellar bone.
5-Remodeling: finally the crude bone which bridge the # site will be re
shaped and the medullary canal re formed.
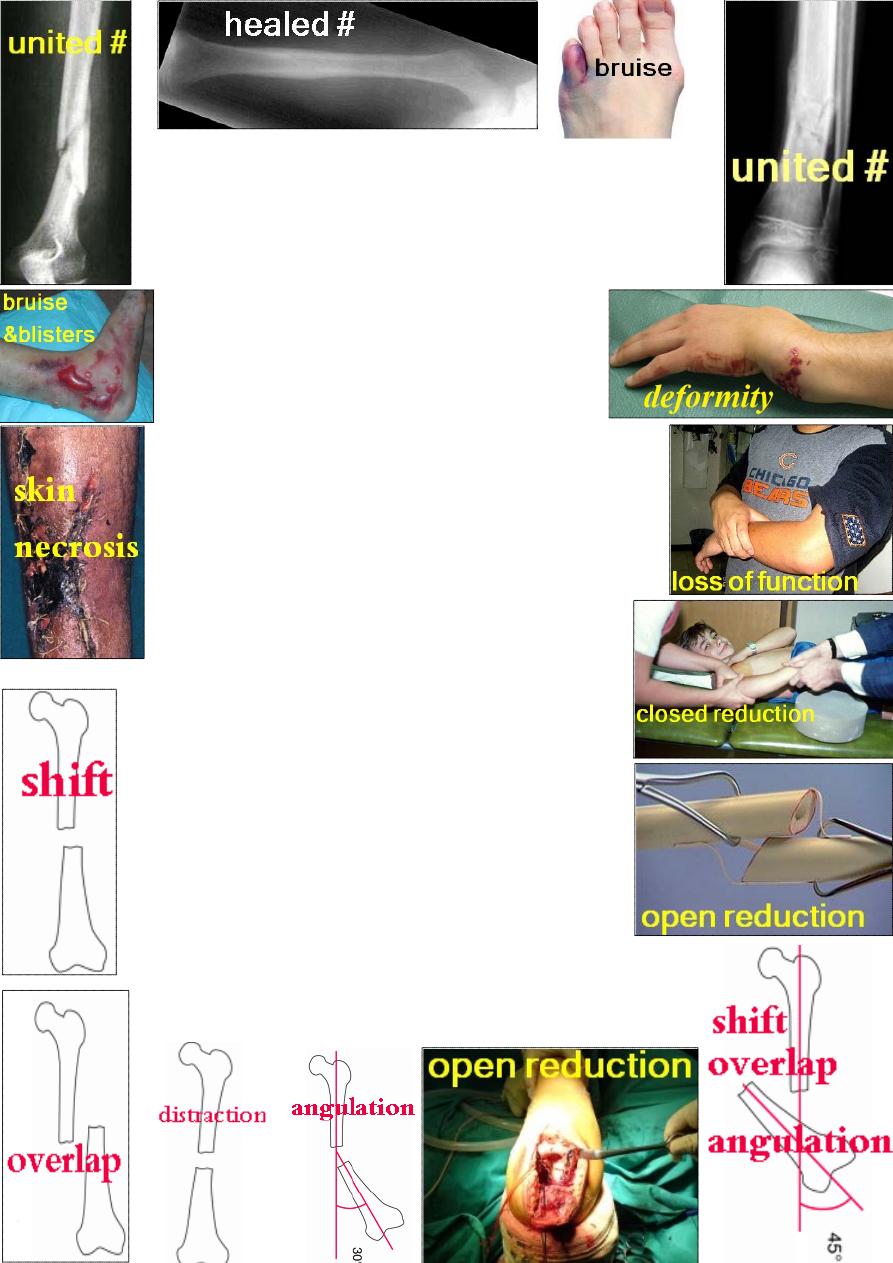
Union
: is incomplete repair of a fracture; there is tenderness at the
fracture site, and although the fragments move together, but if you
try to angulate the bone it is painful. X-ray will show immature bone.
Consolidation:
is complete repair with mature bone. There is no
tenderness, no pain, and x-ray show no fracture line and the area is
crossed by bone trabecullae (mature bone).
Clinical features of fracture:
There is a history of injury and loss of function, pain,
swelling, bruising, and deformity. Always look for
nerve, vessel and visceral injury.
Examination:
General: look for shock, hemorrhage and associated injuries.
Local exam.: look for skin damage (open or closed #),
& for distal pulse and sensation.
Imaging: X-ray; CT (for # vertebra, pelvis, calcaneum);
MRI (spine injury) and isotope scan (stress fracture).
Treatment of closed fracture:
I-General treatment: 1- first aid. 2- Transport.
3-
Ŗ of shock, hemorrhage and associated injuries.
П-Treatment of the fracture: three steps:
1- Reduction (reduce).
2- Immobilization (hold).
3- Rehabilitation (exercise).
Reduction:
means you reduce the fragments into normal
position with no shortening, no overlap, no angulation &
no rotation. Either by closed or open procedure.
Closed reduction: under anesthesia, do manipulate the
fragments into normal position by reversing the force
which causes the fracture.
Open reduction: you surgically open the # site and reduce
under direct vision. The indications are: 1-failure of closed
reduction. 2-Soft tissue interposition. 3-Intraarticular fractures.
Immobilization
: to prevent displacement of bone ends. There are five
types: 1- Cast splintage. 2- Continuous traction.
3- Functional bracing. 4- Internal fixation. 5- External fixation.
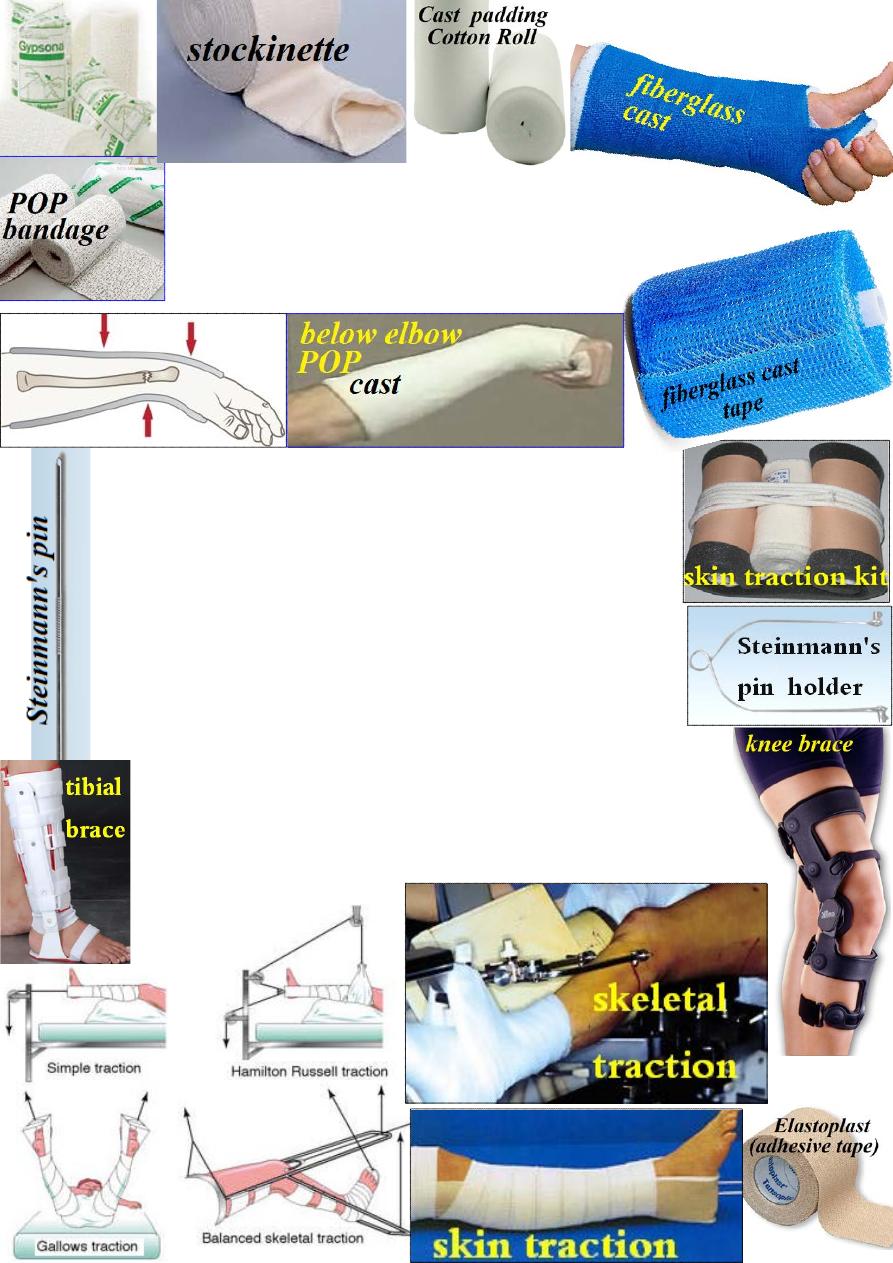
Cast splintage:
Plaster of Paris (POP) casting is the standard
method. It is hemi hydrated calcium sulphate which reacts with water
to form hydrated calcium sulphate with heat production (exothermic
reaction). A new fiberglass cast is lighter &impervious to water.
The disadvantages of casting are: tight cast, pressure
sore & stiffness.
Continuous traction:
in oblique or spiral shaft # usually there
is displacement because of muscle pull, so by applying continuous
traction distal to the #, reduction and holding of the fragments
could be achieved. Traction is either through skin or bone:
Skin traction: Elastoplasts is applied to the skin distal to the
fracture and held on with bandage, the cords are used to hold
the weight (up to 5 kg otherwise it may slip).
Skeletal traction: Steinmann's pin is inserted transversely through
the bone e.g. fracture femur, it is inserted one inch below and one
inch behind tibial tubercle. A loop is attached to move freely on
the pin and holding the cords that lifting the weight.
Functional bracing:
a plastic cast is applied only to the shafts of the
bones leaving the joints free to avoid stiffness; the casts are connected by
hinges which allow movements in one plane. it should be used only when
the fracture started to unite to avoid redisplacement.
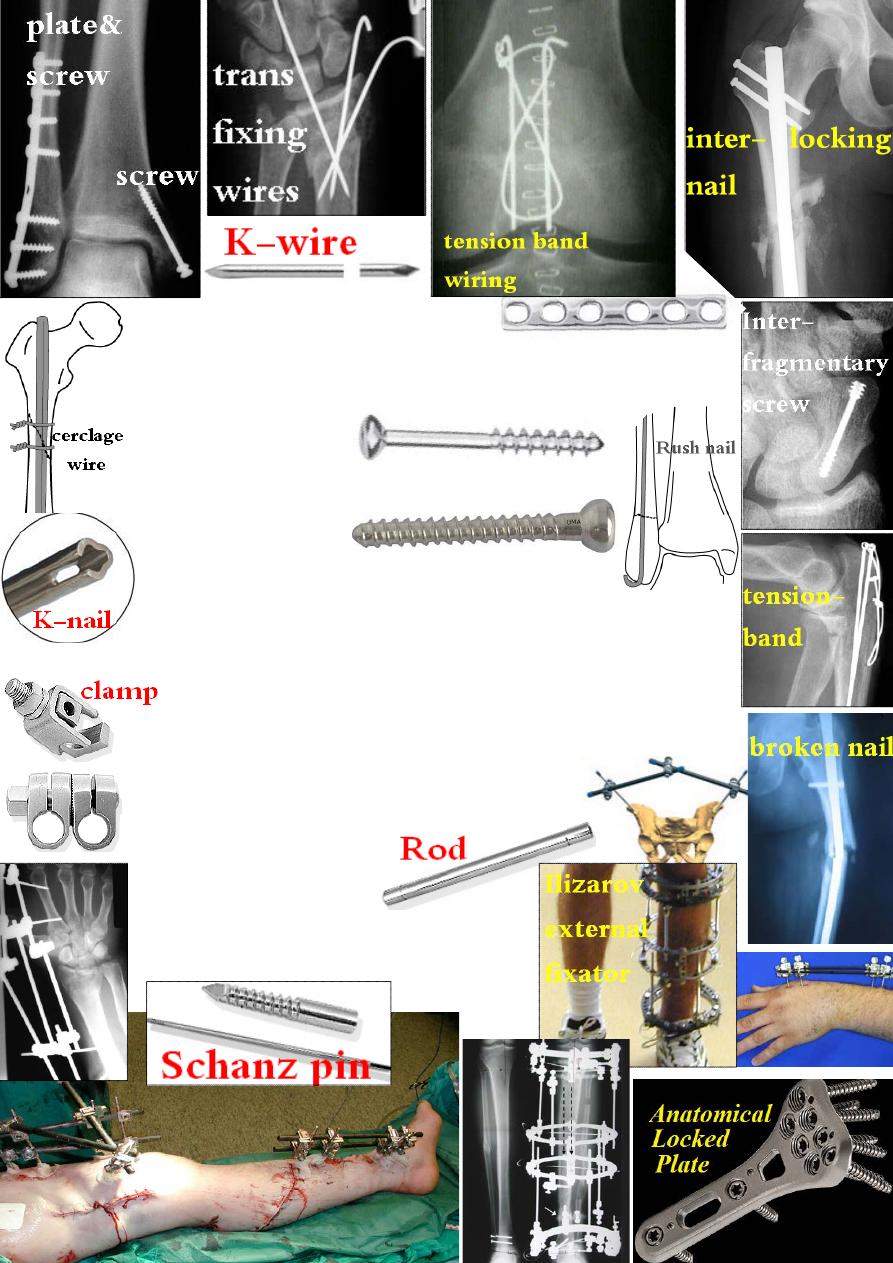
Internal fixation:
types:
1- Plate and screws (conventional, anatomical & locked).
2- Wires (transfixing, cerclage and tension-band).
3- Intramedullary nail (locked &unlocked Kuntscher nail &Rush nail).
4- Interfragmentary screw.
Indications:
1- Fractures that cannot be reduced except by operation.
2- Unstable fractures.
3- Pathological fractures.
4- Multiple fractures.
5- To avoid nonunion e.g. femoral neck and scaphoid.
6- In elderly to avoid bed sore, DVT, pulmonary embolism and chest
infection.
Complications: 1-Infection. 2-Nonunion. 3-Implant failure. 4- refracture.
Contraindication: open fracture because of fracture contamination.
External fixation:
using certain pins or wires that pass through the
bone above and below the # and attached to external frame or bar.
Indications: 1- open # with severe soft tissue damage.
2- Fracture with nerve or vessel injury.
3- Severely comminuted and unstable fracture.
4- Infected fracture.
5- Pelvis fracture.
6- Severe multiple injuries.
7- Ununited # (compression/ elongation).
Complications: 1- neurovascular damage.
2- over distraction. 3- pin-track infection.
