Pneumonia
Pneumonia
• Is inflammatory of parenchyma of the lungs ,
associated with consolidation of alveolar spaces.
• Is substantial cause of morbidity & mortality in
childhood Particularly among children below 5
years of age .

Etiology :--- depend on the
1- age of patient
2- immune state
3- presence of cystic fibrosis or other chronic lung dis
4- exposure history & nosocomial versus community .
• The cause of pneumonia in an individual patient is often difficult
to determine because the direct culture of lung tissue is invasive
and rarely performed even culture performed.
on specimen obtained from URTI or sputom often does not
accurately reflect the cause of lower respiratory tract infection .
• Strepto –coccus pneumonia ( pneumococcus) is most common
bacterial pathogen from 3 wk -5 years, where as chlamydia &
mycoplasma are frequent above 5 years.
• Other bacterial causes in previously healthy children include
group A strepto coccus & staph aureus .
• Pneumo-coccus , staph , H. influnza are a major causes of
hospitalization & death from pneumonia among children .

• Viral pathogens are a prominent cause of lower RTI in
infant & children below 5 years of age , its responsible for
45% of the episodes identified in hospitalized children (
highest frequency between the age 2-3 years of age &
decreased slowly after which unlike bronchiolitis with
peak incidence in Ist year of life .
Pneumonia is caused by :--
1- infection : viral ( common cause ) , bacterial , Ricketisial,
fungal parasite .
2-inflammatory process like SLE, sarcoidosis , histiocytosis
3- toxic substances like hydrocarbon , gastric contents ,
dust, gases & chemical substances .

• Common causes according to age :- bacterial viral
others
1. Neonate :-group B strep., E-coli , Listeria ,
H.infl,CMV,Herprs , ureoplasma urolyticum
2. 1-3 months : strept. , H. inf.,: RSV, PIV , CMV, :
chlamydia
3. 3-12 month : strep. , H. infl, staph : RSV,PIV
,adeno :
4. 2-5 years :-pneumo coccus , strepto. Group A ,
staph , H.inf. PIV, Influ. Virus , adeno
mycoplasma , chlamydia
5. 5-18 years ; strept. , H. infl . adeno, influnza
mycoplasma

• Pathogenesis :--
LRTI is normally kept sterile by physiological
defense mechanism including the mucocilliary
clearance , properties of normal secretion such as
secretory IgA& clearing of air way by coughing
Viral pneumonia :- usually result from :-
1- direct injury to epithelium resulting in air way
obstruction from swelling , abnormal secretion ,
cellular debris .
2- is predisposed to secondary bacterial infection by
disturbances of normal host defense mechanism ,
altering secretion , modifying bacterial flora .

Bacterial infection :--
A. S. pneumonia : producing local edema that aids
in proliferation of organism & then spreads to
adjacent portion of lung causing lobar
pneumonia
B. group A strepto-coccal ; result in more diffuse
infection with interstial pneumonia .
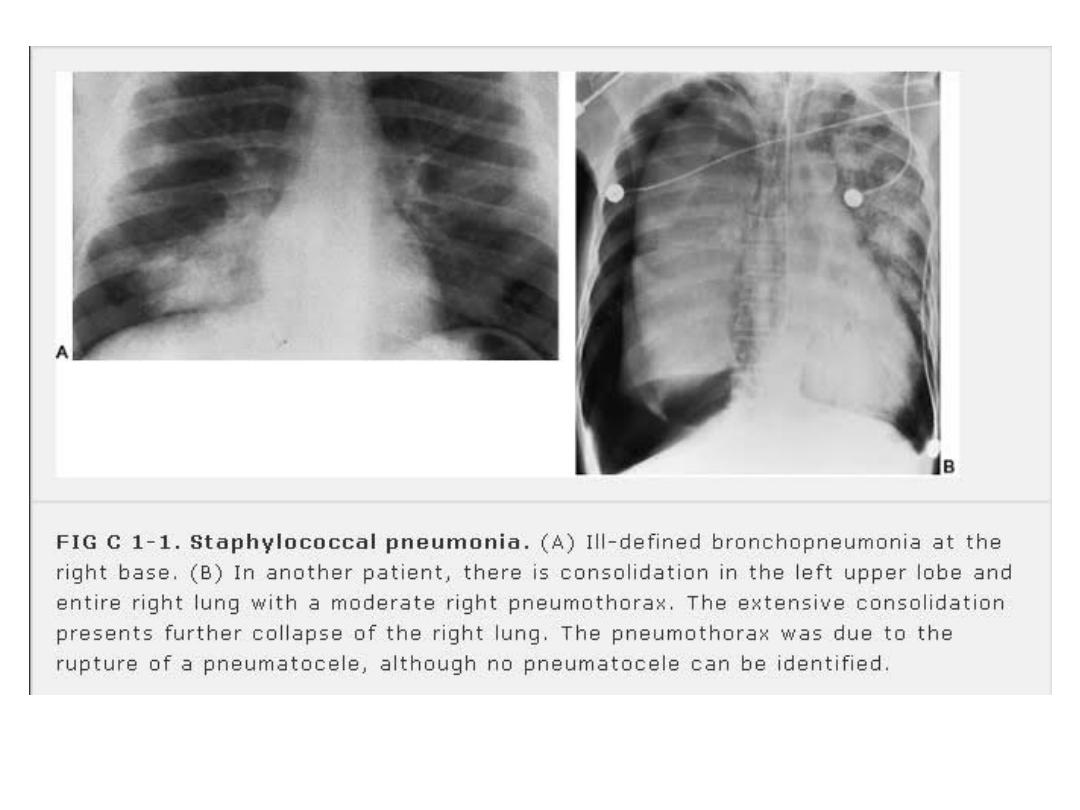
C. staph infection :- manifest as confluent broncho
pneumonia which is unilateral & characterized by
extensive area of haemorrhage, necrosis &
irregular area of cavitation resulting in
pneumatocele , empyma, broncho pleural fistula
• C. Recurrent Pneumonia :--
is defined as 2 or more episode in a single year Or 3 or more
episode ever , with x-ray clearing between occurrence.
DD of recurrent pneumonia :--
1- hereditary disorders ;- cystic fibrosis , SCA.(sickle cell
anemia)
2- disorder of immunity :-AIDS , Bruton a gama globulinemia
,CVIDS(common variable immune deficiency syndrome) ,
SCIDS(sever combined immune deficiency syndrome) .
3- WBC disorders :-chronic granulomatous dis, Job syndrome ,
WBC adhesive defects .
4- Disorder of cilia : immotile cilia syndrome & kartagner synd.
5- Anatomical defects :- sequestration , Lobar emphysema ,
esophageal reflux , Foreign body , G .O.R, Tracheo-esoph
fistula ( H-type ) , oro-pharyngeal incoordination .

ClF :-
• viral & bacterial are often proceeded of several
days symptoms of an URTI.
• in viral pneumonia : fever is less than in Bacterial
infection
• Tachypnea is consistant with pneumonia
• cynosis in sever infection especially in infant
• by auscultation :- rhonchi , cripitation ( difficult to
localize the source of these in very young
infant)

Bacterial Pneumonia :--
in older children :-typically begin suddenly with a shaking chill
followed by high fever , cough , chest pain , may accompany by
drowsiness with intermittent episode of restlessness , rapid
respiration & many children noted to be splinting on affected side
to reduce pain and improved ventilation .
OlE :- depend on stage of pneumonia :
• early in course of disease ; diminished breath sound , scattered
cripitation & rhonchi .
• with development of consolidation or CX like effusion ,
empyema , shows dullness on percussion .
• abdominal distension may be prominent due to gastric
dilatation , ileus , swallowed air .
• Abdominal pain is common in lower lobar pneumonia & nuchal
rigidity in upper lobar pneumonia with out meningitis .
• In infant :-- may proceeded by URTI , depressed appetite leading
to abrupt onset of fever , restlessness, apprehensive & resp
distress, may associated with G.I.T disturbances .

• Infant appeared ill , with sign of respiratory distress , may
associated with gastro intestinal disturbances Rapid
progressive symptoms is characteristic in most sever cases of
bacterial pneumonia .
Dignosis
1- clinical diagnosis
2- chest x-ray :-may confirm pneumonia,& may indicate the CX
like pleural effusion , empyema
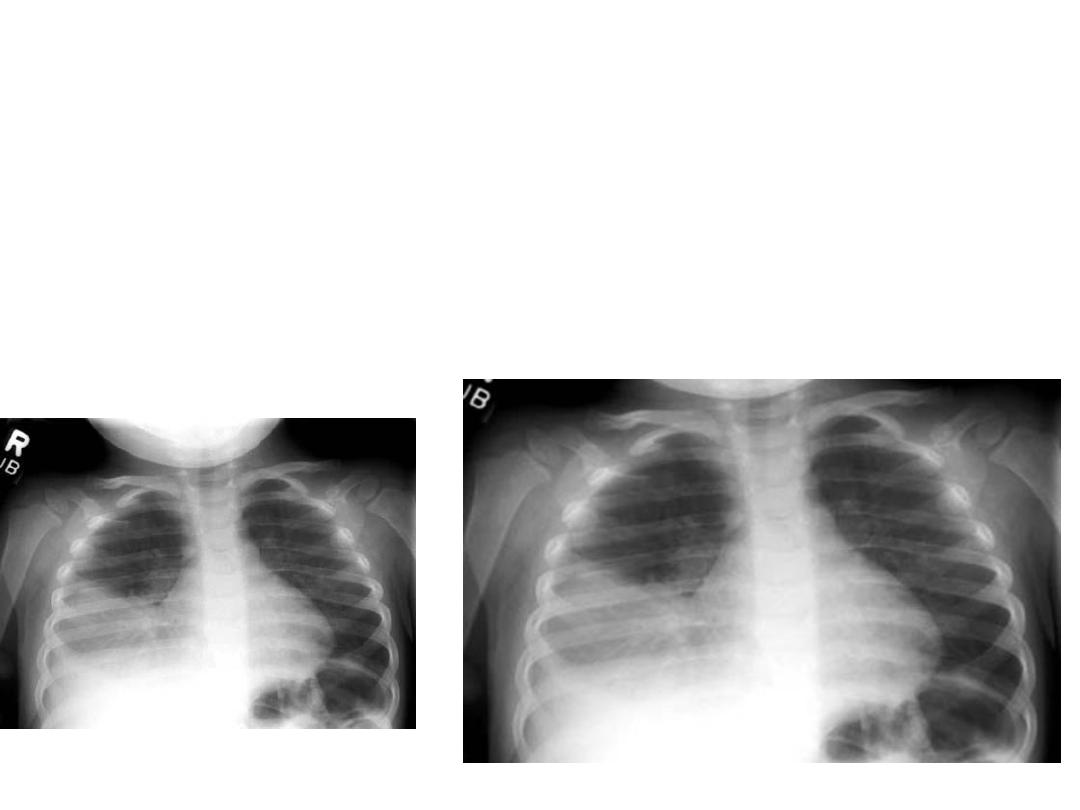
in viral pneumonia : hyperifilteration with bilateral interstitial
infiltration
lobar consolidation is typically seen in patients with
pneumococcal pneumonia .
3- WBC : important to differentiate between viral from
bacterial

• Note : pleural effusion , lobar pneumonia , & high
fever suggested
A. bacterial pneumonia .
B. Atypical pneumonia due to chlamydia or
mycoplasma is difficult to differentiated from
pneumococcal pneum by x-ray & other lab.
C. although pneumococcal is associated with high ESR,
WBC&C-RP
D. Viral pneumonia : WBC are normal or slightly
elevated ( of not more than 20000/mm with
lymphocyte prominent
E. In bacterial pneumonia ( and usually adeno virus )
often associated with increased WBC ( 15000—
40000 )with PMN predominant ..

• Definitive diagnosis of viral pneumonia by
isolation of virus or detection viral genome or
antigene in resp tract secretion .
• While bacterial pneumonia required isolation of
Micro-Organism from blood ,lung and pleural fluid
• sputum culture is little value in diagnosis of
pneumonia in young children .
• In mycoplasma is diagnosed on basis of PCR or
sero-conversion in an IgG assay ( cold agglutinine
at titer of more than 1:64 are found in 50% ) .cold
aggluti. are not specific which may +ve in
influenza virus .
• ASOT is useful for group A strepto coccal pneum.

Treatment :--
treatment of suspected pneumonia is based on
presumptive cause , & clinical appearance of child
• mild ill ( home treatment ) by amoxyline 80-90 mg
/Kg / day & alternative with cefuroxime axetil 15-
30mg/kg/day or augmentin .
• In school age children with suspected mycoplasma
azithromycin
• Hospital treatment parenteral cefuroxime 75-150
mglkglday or cefotaxime or ceftriaxone.
If suggest staph : vancomycin or clindamycin
• In viral pneumonia ; no need antibiotic 30% of viral
pneumonia may have coexisting bacterial pathogene .
• Oral zinc 20mg l day may accelerate recovery for sever
pneumonia

Indication of admission of pneumonia :---
1- age of less than 6 month
2- SCA with acute chest syndrom or multiple lobe involvement
4- immune compromized pt.
5- toxic pt.
6- sever resp distress
7- required 02 therapy
8- dehydration
9- vomiting
10- non compliance
11- non response to oral therapy
Response to therapy :---
• clinical improvement in uncomplicated pneumonia
within 48-96 hr of initiation of A.B( antibiotic)
• x-ray evidence of improvement lags behind clinical
improvement

• Number of factors must be considered if patient not respond to treatment ;---
1-Cx like empyema
2- bacterial resistance
3- non bacterial etiology like viral or aspiration of F.B or food
4- bronchial obstruction from endobronchial lesion , F.B & mucous plug
5- pre-existing dis like immune def , pulmonary sequestration
malformation , cystic fibrosis
6-other non infectious causes like bronchiolitis obliterance , aspiration
CX :--
• are usually the result from direct spread of infection within thoracic (
pleural effusion , empyema , &pericarditis ) . or bacteremia or
hematological spreads ( meningitis , suppurative arthritis ,
osteomylitis ) are rare cx of pneumoccocus or H influenza ) Staph
aureus , S.peneumonia , S.pyogene are important causes of
parapeumonia effusion and of empyema .

• Staphylo-coccus pneumonia :- is serious & rapidly progressive
infection that is associated with prolong morbidity &high
mortality ( unless recognize early & treated
appropriately ), is more common in infant than in children ( 30%
under 3 month & 70% under Ist year of life ) .
ClF :-
1- frequently proceeded by URTI of several days to one wk then
patient abruptly has high fever , cough & evidence of resp distress
& S.T associated with gastro intestinal disturbances characterized
by vomiting , anorexia & abdominal distension which Secondary to
paralytic illeus .
Diagnosis :-
• ClF + WBC ( leucocytosis of more than 20000/mm with
predominantly PMN ( in young infant S.T WBC remains normal )
& if WBC of less than 5000 is poor prognosis
3- pleural tap or tracheal aspiration for gram stain &culture
4- chest –x ray :- non specific broncho pneumonia
in early stage( Rt lung only in 65%and bilateral in
20% ) May associated with pleural effusion or
empyema May associated with pneumatocele .
CXR should be obtained at frequent interval when
diagnosis is suspected
• Note ;-rapid progressive from bronch-pneumonia
to effusion or pyo-Pneumothorax with or without
pneumatocele is highly suggestive staph
pneumonia .
• Clinical improvement usually proceeded chest x-
ray which cleared by days or wks & pneumatocele
may persist for months .

CX :-
1- empyema ,pyo-pneumothorax
2-septic lesion outside resp. Tract which rarely occur in young
infant like pericarditis , osteomylitis , meningitis
Treatment ;--
1- supportive therapy ( 02 ,I.V fluid , S.T needs assisted
ventilation , chest tube is indicated if effusion with empyema
Repeated pleural tap to reduce chance of fistula
2- specific therapy ( naficilin 200mg/kg . Methicilin , cloxacilin )
if sensetive to pencillin , used vancomycin 40mg/kg by infusion
• prevention of pneumonia :- by vaccine
1- pnumococcal ( 7 valent &13 valent conjugated.
2-infunza vaccine which. given to all children after 6 months of
age .
• 13 valent given protection to those not covered by 7 valent
vaccine .