
Bronchial Asthma

• Bronchial asthma :--
is chronic inflammatory condition of the lung air way
resulting in a episodic air flow obstruction ( this is
resulting heightens the twitchiness of the air way ( air
way hyper responsiveness to provocative exposure.
• Or is defined as a paroxysmal , diffuse obstructive lung
dis with hyper-reactivity of the air way to variety of
stimuli & high degree of reversibility of the obstructive
process which may occur either spontaneously or by
treatment
• Asthma is most common chronic disease of childhood
and is leading cause of emergency room visit , hospital
admission and school absenteeism

• Asthma management is aimed of reducing air way
inflammation :--
1- minimizing post inflammation environmental
exposures.
2- using daily controller ( anti inflammatory
medication )
3- control comorbid condition that can worsen asthma (
rhinitis , sinusitis & G.O.R )G.O.R mean gastro esophageal
reflux
• Less inflam is better control with fewer exacerbation .

• Trigger factors of asthma :--
1- respiratory tract infection like RSV, influenza( which are trigger
asthma in early life ) & para influenza , rhino virus trigger in adult
patients . rhino virus
2- aero allergen in sensitized asthma like ( animal dander ,wet paint,
indoor allergen (dust mite , pet, molds, cockroaches ) , seasonal aero
allergen ( trees , grass , weeds)
3- environmental tobacco smoke
4- air pollution ( sulfure dioxide ,dust , wood , coal burning smoke &
endotoxin )
5 exposure to cold air & dry air
6- exercise
7-strong & noxious odor fumes.
8- comorbid condition
9-drug administration (aspirin, NSAID, B-blocker ) 10.cough after
laughing or crying

• risk factors for persistant asthma in early childhood ;
1-parental asthma .
2-allergy ( eczema ,allergic rhinitis , food allergy
3-severLRTI as in pneumonia and bronchiolitis
4- wheezing apart from cold 5- male gender 6-LBW
7-exposure to chlorinated swimming pool 8-envirmontal exposure
• Asthma predictive index( API ) :- its aim to help whose children are
more likely to have asthma later in life .it includes frequent
wheezing during first 3 years of age and either 1 major risk factors (
parent history of asthma or child diagnosis of eczema ) or 2 of 3
minor risk factors ( blood eosinophilia , wheezing without cold and
allergic rhinitis ) ,
• Children with positive API were 4.3—9.8 times more likely to have
active asthma between 6—13 years than children with negative API
while those with negative API risk factors had a negative predictive
value of 94%for development of asthma at age 6 year.

• Attack of asthma occurs in 30% in Ist year of life & 80-90% within 4-
5years of age . If onset in first year of age & there is family history
of asthma or allergic disorder
those patients have :--
1- growth retarded unrelated to cortico-steriod
2- chest deformity secondary to hyper-inflation & persistant
abnormality of PFT( pulmonary function test ) .
• Fate of asthma :-- in general , the prognosis is good in young
children :--
1- 50% of all patients are virtually free of symptoms within 10-
20years but recurrence are common in adulthood .
2- children who have mild asthma with onset between 2year &
puberty , the remission rate is about 50% & only 5% experience sever
asthma .
3- children with sever asthma characterized by steroid dependant
with frequent hospitalization rarely improved & about 95% become
adult asthma .

Etiology :--
the cause of childhood asthma has not been
determined , implicated a combination of
environmental exposures , biological , genetic &
immunological factors .
• Mediators release causing broncho-spasm by :--
1-direct action on smooth muscle
2-stimulation of vagal sensory receptor.
Viral infection trigger asthma through :-
1-afferant vagal receptor
2- IgE response to RSV which occur in both infant &
children ( RSV & PIV trigger asthma in early life while
rhino virus & influenza virus trigger in adult asthma .

Types of asthma :--
classify into: -
a- recurrent wheezing : ( trigger by common
respiratory viral infection in early childhood ) .
b- chronic asthma : associated with allergy that persist
into later childhood and often adulthood .
C- 3rd type emerge in female who experience obesity
,early puberty.
Or classify into :--
1-extrensic asthma ( allergic type) (has positive skin
test & increased IgE& specific IgE agaist allergen
2- intrinsic asthma( non allergic type ) has –ve skin test

ClF :-- into 2 forms ;--
a- acute episode :-occurs within minutes which commonly
happen at night due to decreased patency of air way ( classify
into 2 types either as early asthma response occur with IgE
induced mediator release from mast cell within minute of
exposure and last for 20-30 minute and late onset asthma
occur 4-12 hr after exposure resulting in more sever symptoms
and last for hours , where inflammatory cell infiltration and
inflammatory mediator play role in late onset asthma it is
usually follow exposures to irritant like cold air , noxious fumes
like smoke , wet paint , allergen & drug like aspirin .
b- insidious episode :- usually proceeded by viral infection
C/F is variable from mild to sever as :-
• respiratory distress , wheezing ( S.T without wheezing) just
cough , may associated with abdominal pain , excessive
sweating , Vomiting is common
• Cough may be only symptoms especially in case exercise
induced asthma and nocturnal asthma

• In nocturnal asthma :-the cough usually occur after
midnight and early morning hours
• In mild chronic asthma , patient is entirely normal in
between attack
• In sever attack ( associated with danger sign ) :-
characterized by:-
1-silent chest 2- inability to talk or walk
3- tripod position 4-cynosis 5- exhaustion
In chronic asthma : characterized by :--
1- barrel chest 2- harrison sulci
3- antero lateral depresion of thorax at insertion of
diaphragm
4-clubbing of fingers which suggest cystic fibrosis .

Diagnosis :--
1- clinical diagnosis by
a- recurrent episodic of wheezing or coughing ( S.T only
persistent cough ) +
b-rapid improvement with using bronchdilator +
c-+ve family history of atopy
2- laboratory evaluation :-
a-eosinophil in blood & sputum IgE is increased in
allergic type
b-skin test & RAST( RAST is determined specific IgE
concentration in serum ) RAST mean radio sorbent immune
assay .
3- exercise test

4- chest x-ray :- ( as hyper-inflation of chest , some time
atelactasis as small patches or may associated with
pneumothorax or pneumomediastinum .
indication CXR in the following :--
a- first attack of wheezing
b- associated with high fever
c- suspected cx like pneumothorax or pneumo
mediastinum
d- if resp rate of more than 60 & pulse rate of more than
160
e- localized wheeze or rales or decreased breath sound
5- blood gas analysis ( elevation of PCO2 is ominous sign)

5- pulmonary function test :-importan
t in (not reliable bellow 5 years of age)
a- asses degree of air way obstruction & disturbances of gas exchange
b- in measuring response of air way to inhaled allergen , exercise ,
chemical
c-asses response to therapeutic agent
d-in evaluation of long term course of diseases
• Measuring PEFR & FEV1 before therapy & after broncho-dilator :-
if increased 10% strongly suggestive asthma Failure of response is not
exclude asthma due to :--
1- status asthmaticus 2- near maximal PFT
Note :-it is feasible to monitor PEFR 2-3 times per day which provide
objective measuring of degree of air way obstruction .
• DD of wheezy chest :--
1- infection 2- anatomical & congenital ( G.O.R, H-type fistula,
cystic fibrosis , vascular ring ) 3- vasculitis
4- others like Foreign.Body , broncho- pulmonary dysplasia
,psychogenic cough , pul thrombo embolism

Pathophysiology of asthma :
firstly exposure to trigger factors ( various stimuli ) resulting in mast
cell destruction with releasing of chemical mediator like histamine ,
leukotrine , platelet activated factors causing bronchospasm , mucosal
oedema and excessive secretion
• air way obstruction ( early immune response resulting in
bronchospasm which prevented by mast cell stabilizing agent , while
late immune response occurs 6-8 hrs later resulting from infiltration
of eosinophile and neutrophile which prevented by steriod and mast
cell stabilizing drug) .
• Obstruction is more sever with expiration ( due to smaller air way
than through inspiration ) which clinically appeared as wheezing or
rhonchi ) .
• If obstruction is increased leading to inspiratory and expiratory
rhonchi and this obstruction causing :--
1. hyper inflation of chest( partial obstruction )
2. atelectasis ( complete obstruction )
3. non uniform ventilation

• Hyperinflation causing decreased compliance of lung with
increasing work of breathing causing hypoxia and
hypercapnia leading acidosis and pulmonary
vasoconstriction leading to decreased surfactant resulting
in atelactasis .
• Hypoxia is interfere with conversion of lactic acid into co2
+ H2O resulting in metabolic acidosis
• Hypercapnia that increased carbonic acid dissociation into
Hydrogen ion and Hco3 causing in respiratory acidosis .
• Increased intrathoracic pressure may interfere with
venous return and reduced cardiac output manifested
clinically as pulsus paradoxsus .

• Exercise test :--
running for 1-2 minutes causing bronchdilator , while
prolong strenous exercise leading to bronchconstriction .
• Before test doing : bronchodilator and cromolyn withhold
for at least 6-8 hour , while slow releasing theophylin
should not be administered at least 12 -24 hr prior the test
.
• The test done by treadmill through running 3-4 mile / hr
up to 15% grade while breathing through mouth for at
least 6 minute leading to air way obstruction .
• PFT ( pulmonary function test ) done immediately before
and after test , 5 , 10 minute
• Showing decreased PEFR or FEV in one second of at least
15% without premedication .
• Note :-- if no air way obstruction , it is best to repeat the
test in other day when relative humidity is low .

How to control dust mite :--
• Mite allergens presented in mattresses , box
springs , pillow and carpet
1- carpet should be washed at least once per week
in hot water 70%, where cold water does not kill
mites .
2- if removal of carpet from bed room is impossible ,
washed by tannic acid that inactivate mite and
repeated every 2-3 months .
• or used Benzyl benzoate that kill mite and
repeated every few months .

• Differentiation between intrinsic and extrinsic asthma :--
factors extrinsic intrinsic
clinical differentiation
1-age 2-12 years Ist 2 years and after 12
years
2-onset of symptom acute insidious
3- response to treatment rapid response slow response
4-type of trigger factors allergen like dust , mite viral infection
indoor allergen , drugs , etc
Investigation :
1- skin test positive usually negative
2-IgE increased usually not
elevated
3-RAST positive usually negative
4- eosinophile increased usually normal

Approach to patient with asthma

• Approach patient with asthma to asses severity of
asthma by :--
a- scoring of asthma
b- classification of severity of asthma
A- scoring of asthma :
• depend on many factors including mental state ,
cyanosis , accessory muscle , air exchange , pulsus
parodoxus , Pao2 , Paco2
Scoring :--
1. 0-4 no needs admission
2. 5-6 – impending resp failure
3. more than 7 – resp failure – needs I.C.U with
intubation
I.C.U ( intensive care unit )
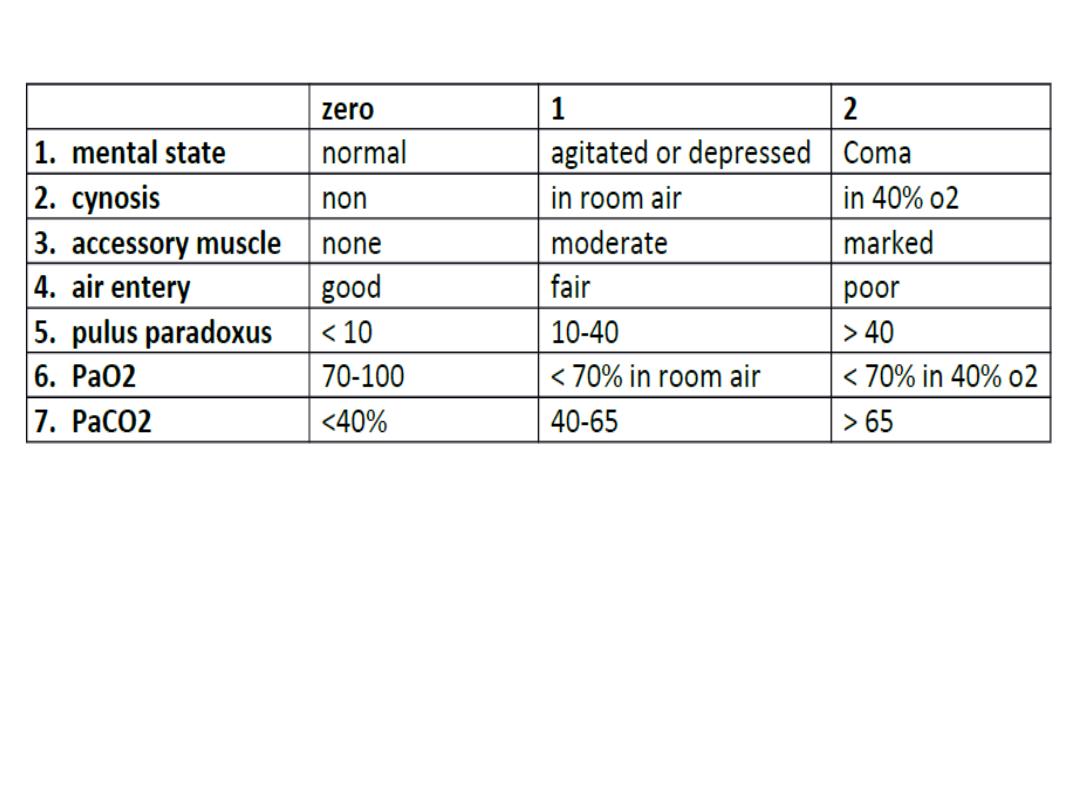
• Scoring of asthma
• Scoring :-
1. 0-4 :- no immediate danger ---------- home
discharge
2. 5-6 :- impending respiratory failure ------ hospital
admission
3. > 7 :- respiratory failure --------- intensive care unit
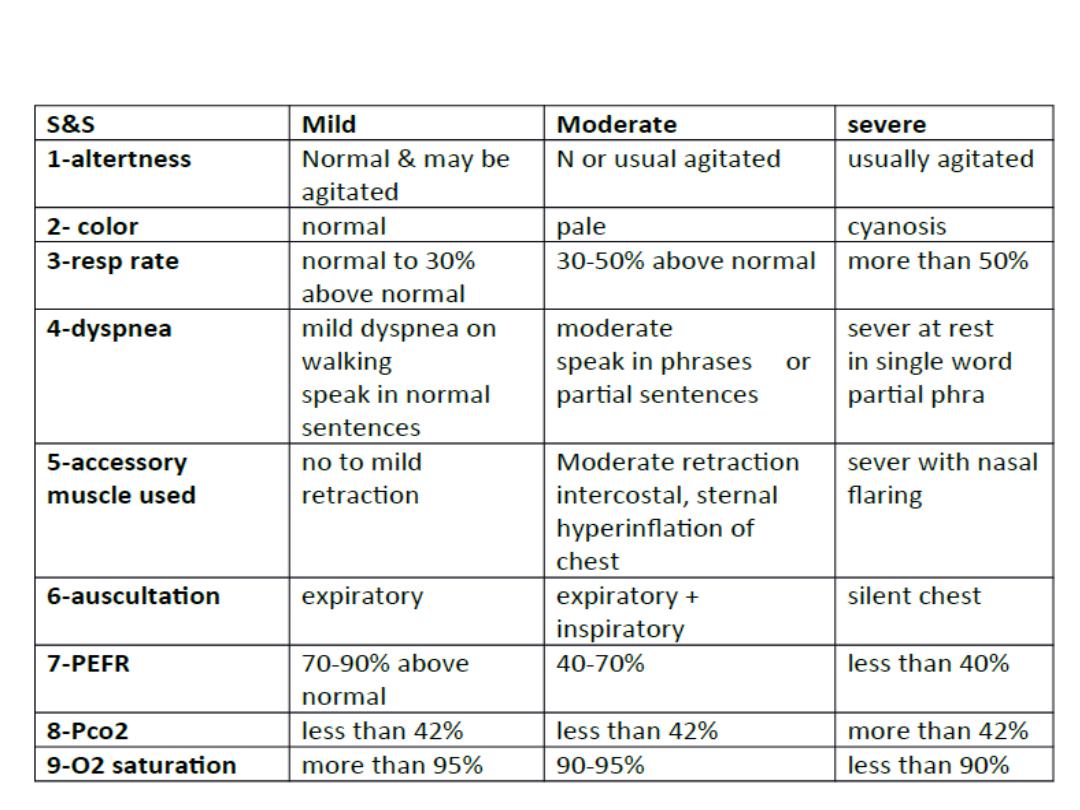
• B-classification :- can asses severity of acute exacerbation in
children :

• Aims of therapy :--
1-to reverse asthmatic symptoms .
2-prevent or diminished the frequency of recurrence of symptoms
3-maintain normal or close to normal pulmonary Function test
4-maintain normal activity level including exercise .
Treatment of acute asthma :---
• depend on severity & location ( home , emergency ward
,hospital)
Home management :--
1-PEFR :- done every 2-3 times per day ( if PEFR is decreased
needs medical intervention & if decreased between 50-80% needs
change in medical therapy & if below 50% needs acute
intervention
2-inhalation therapy by ventolin inhaler
3-incomplete response needs short course of cortico steriod like
prednisolone 1-2mg/kg/day .
4- medical attention:-should be looking for or sought for sever
exacerbation & persistent respiratory distress .

• In emergency ward :--
1-O2 therapy :-to improve oxygenationwhich given by mask or
nasal
prongs 2-3/ min.( hypoxia caused by acute episode of
asthma and drugs used in treatment like B-agonist , aminophylin
( as result in VPM through pulmonary vasodilator and increased
cardiac output . Mist tent should not be used as resulting in
irritation leading to coughing and worsening wheezing . .
2-ventolin or albuterol nebulizer 0.15mglkg every 20 minutes for
one hour.
Inhaled iprotropium bromide ( given every 6 hr in a dose o.25
mg for 6 years of age and o.5 mg for those 12 years of age )
3-may need systemic Cortico.Steriod either orally or I.V
4-in sever case , used S.C adrenalin 0.01ml/kg given once or twice
at interval 20 minutes to obtain optimum relief ( 0.05 ml is often
effectively in infant and young children )

• after one hr ---re-asses :-
1-if sustained improvement of symptoms , normal
physical finding & O2 saturation of more than 92% ,
PEF of more than 70% for 3 hr ----home discharge .
if discharge , on 1-ventolin inhaler for above 5 years
or oral salbutamol
2- 3-7 day course of C.S
2- if no response ( persistent symptoms ) ---asses &
hospital admission :
a- if moderate distress needs ward admission
b- if sever distress needs I.C.U

• Indication of hospital admission :--
1-moderate to sever exacerbation that not improved
within 1-2hr from intensive therapy in emergency ward .
2-has risk factors for morbidity & mortality ( risk factors
for sever
asthma ) :---
A- biological –
1-previous sever asthma exacerbation
2-sever air way obstruction
3- rapid attack
4- sever air way hyper-responsiveness
5-poor response to systemic C.S
6-repeated visit to emergency ward in last 48 hrs
7-2 or more hospital admission of the past year .

• B-economic & psycho-social :--
1- poverty
2- crowding
3-mother less than 20 years
4- poor education
5-family dysfunction
6- psychopath in parent & children
• C-environment :-
1- allergen exposure
2-smoking
3-air pollution
4-urban environment

• Status asthmatics :--
defined by increasing sever asthma that is not respond
to treatment that are usually effective .
• When dignosis is made
A-admission to I.C.U & doing chart for observation for
PR,RR, BP , send for CBP, S.electrolyte , cardiac monitor &
blood gas analysis ( PO2, PCO2, PH )
• B-start therapy :-
1- O2 therapy to maintain PO2 70-90% or O2 saturation
above 92%
2- correction of dehydration: from insensible water loss ,
decreased intake of fluid
and duiretic effect of aminophylin ( should be given 2/3 of
maintainance )

3- bronch-dilator by
a-continuous or frequent Nebulizer with O2
b- aminophylin( 5mg/kg ) or continuous in a dose 0.75-1.25
mglkg /hr
c- anti muscurine like atropin sulfate ( 0.05- 0.1mglkg atropin
sulfate in adose of not > o.25mg ( S.E like mental confusion ,
tachycardia ) iprotropium bromide has fewer S.E than atropin
4- C.S ( methyl prednisolone in adose of 1-2 mg /kg /every 6 hr
5-mechanical ventilation for sever hypoxia o2 saturation of <
90%
6 – sedation is Contra indication .
7-chest x-ray should be done in all patients & repeated as
indicated to detect complication . 8-other therapy like Mg
sulfate in a dose 25-75 mg/kg with maximum dose 2.5 gm ,
inhaled heliox ( has adjuvent therapy ) ,

• Chronic asthma :--classify into :--
( mild , moderate , severe ) depend on history , physical
examination & pulmonary function test .
• severity of asthma Day with symptom night sym FEV1
1-mild intermittent <2episode per wk <2 per month >80%
2-mild persistent 3-6 episode per wk 3-4 per moth >80%
3-moderate persistent daily symptoms >5night per month 60-80%
4-Sever persistent Continuous Sym. Frequent <60%
Prevention :--
Mild intermittent :--
1-no daily medication needed
2-used short acting inhaled B2 agonist ( salbutamol , albuterol ) as
needed ( 1-3 puff every 4 hr )
Mild persistent :-
one daily medication like ( low dose inhaled
C.S 40micro-gram 1-4 puff per day ), intal ( cromolyn) ,nedocromil
& leukotrin antagonist like montolukast , zafirlukast Lipo-oxygenase
inhibition like zileuton which given above 12 years

Moderate persistent:--either:-
A-one daily medication by medium dose inhaled C.S ( 80micro-gram
2-4 puff / twice a day Or
B-two daily medication like low to medium dose inhaled c.s + long
acting bronch-dilator especially for night time symptoms ( salmetrol
) sustained released theophylin or long acting B2 agonist
Sever persistent :--3 daily medication :-
1- high dose inhaled c.s 80 micro gram puff l twice a day +
2-long acting brncho-dilator( salmetrol )or B2 agonist +
3-oral c.s in a dose 1 mg /kg l day of not exceed 60 mg l day then
gradually reduce dose to lowest dose which control symptoms
4- correction comborbid condition & emotional disturbances.
Exercise induced asthma :--prevented by :--
1- inhalation adrenerhic drug immediately before exercise like
inhaled albuterol which give protection for 4 hr . OR inhaled
salmetrol given halve hr before exercise .
2-inhaled cromolyn or nedocromil shortly before exercise

• Theophylline :----
important in treatment of asthma in both acute and
chronic
action of aminophylin:--
1- inhibit CAM phosphodiasterase
2-adenosin antagonism ( affect on ca flux across cell membrane
)
3- prostaglandin antagonism
4-synergism with B agonist
5-enhanse binding of CAMP to CAMP binding protein and
enhance contractility of fatigue diaphragm .
6- increase concentration of endogenous catecholamine .
7. relaxation of bronchial smooth muscle .
• Aminophylin can inhibit both immediate and late phase
asthmatics response .

• Heliox : is a helium- O2 ( 80;20 or 70;30) mixture
that may provide dramatic benefit for emergency
department patients with severe asthma
exacerbation , it is dense as room air and
consequently travel more easily down narrow
passage , which lead to quickly decreasing the
work of breathing ., .
• The gas mixture is used to drive the nebulizer ,by
better delivery of the inhaled bronchodilator .
• Briefly , heliox driven nebulizer treatment should
have the gas set at rate of 8-10 l/min.and with
double usual amount of albuterol .

Steroid action as anti inflammatory
1- alteration of WBC number and activity redistribution
, suppression of migration to site of inflammation ,
decreased response to mitogen , decreased cytotoxicity
and suppressed of delayed hypersensitivity .
2- suppression of mediator release .
3- enhance response to agent that increased CAMP (
PGE2 ).
4-enhance response to catecholamine
• Systemic steroid inhibit late phase response to
antigen , while topical steroid like inhaler steroid
inhibit both early and late phase reaction .

• How to control dust mite :-
• Mites allergen presented in mattresses , pillow ,
carpet :
1-bedding should be washed at least once per
week in hot water ( more than 70 c ) , where the
cold water does not kill mite .
2-if removal of the carpet from bed room is
impossible , we wash the carpet by tannic acid
every 2-3 month which inactivate the mite.
3- or used benzyl benzoate which kill mite which
repeated every few months
