
Reactive arthritis
(spondylo)arthritis (ReA)
Refers to a form of non purulent arthritis, often
accompanied with clinical features keeping with all
SpA
that appear shortly after certain infections of the
genitourinary tract or GIT.
“The classical triad of Reiter’s disease constitutes
non-specific urethritis, conjunctivitis and reactive
arthritis”.

Reactive arthritis can follow or triggered by:
Bacterial dysentery. (Salmonella, Shigella,
Campylobacter, Yersenia).
Sexually acquired reactive arthritis (SARA )with
Chlamydia.
• SARA is considered a disease of young men, with
ratio of male/female 15:1. HLA B27 is +ve in Reiter’s
disease in up to 90% and when there is sacroiliitis,
uveitis or balanitis. Peak incidence between age 16-
35 years but can occur at any age. Reactive arthritis
become most common in people with AIDS.
• Clinical features:
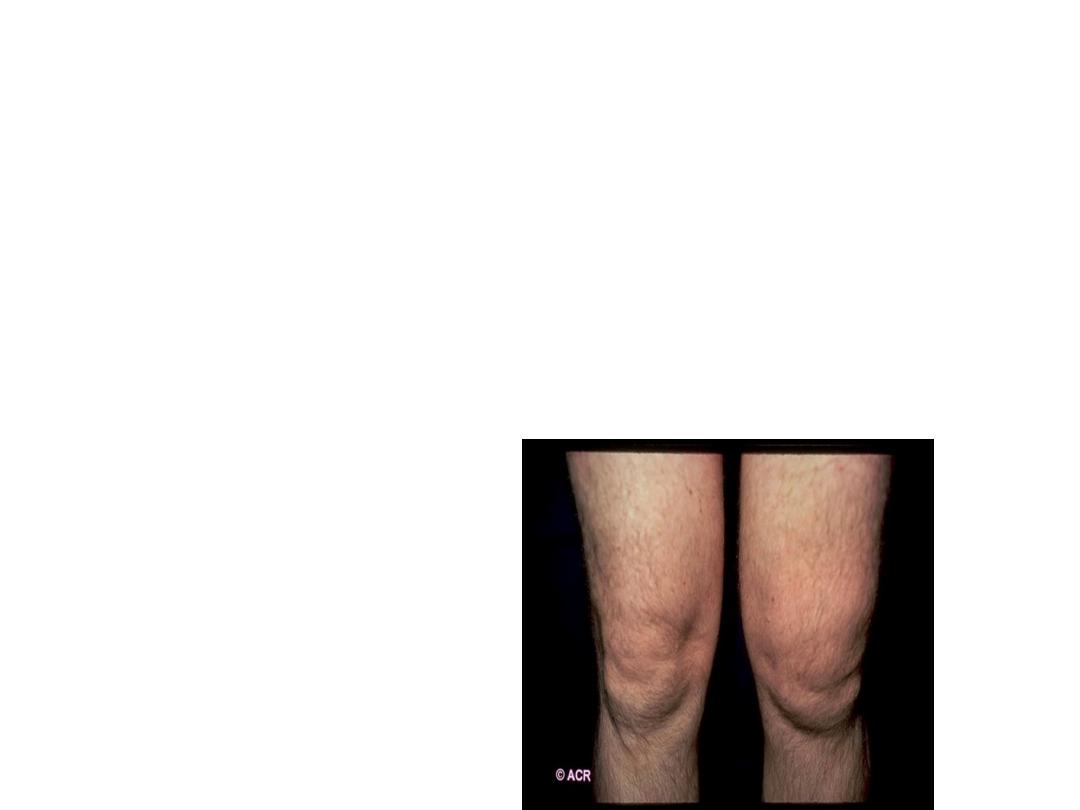
• Onset usually acute, with peripheral arthritis,
usually,assymetric, oligoarticular, mainly joints of
lower limbs knees, ankles , MTP joints , 1-3 weeks
following dysentery or sexually acquired genitor-
urinary tract infection
• . Dactylitis “sussage” digit can occur. Conjunctivitis
and/or non specific urethritis occur in about 50%.
Less classical attacks are common, with insidious
onset of single joint involvement, minimal or
absent features of conjunctivitis and urethritis and
some times
• there is no clear history of trigger illness.
• Achilles tendonitis and plantar fasciitis may occur.
Constitutional systemic features like fever, malaise
and wt loss may occur.

• The first attack can be self – limited with
spontaneous remission with in 2-4 months. But but
recurrent or chronic arthritis can develop and about
10% still
• have active disease 20 years after the initial
presentation. and it is not necessary to preceded by
infection.
• Some of them 15-20% develop progressive
spondylitis with back pain and stiffness due to
sacroiliitis.

• Extra-articular features:
• In addition to conjunctivitis and urethritis mainly in first
attack.
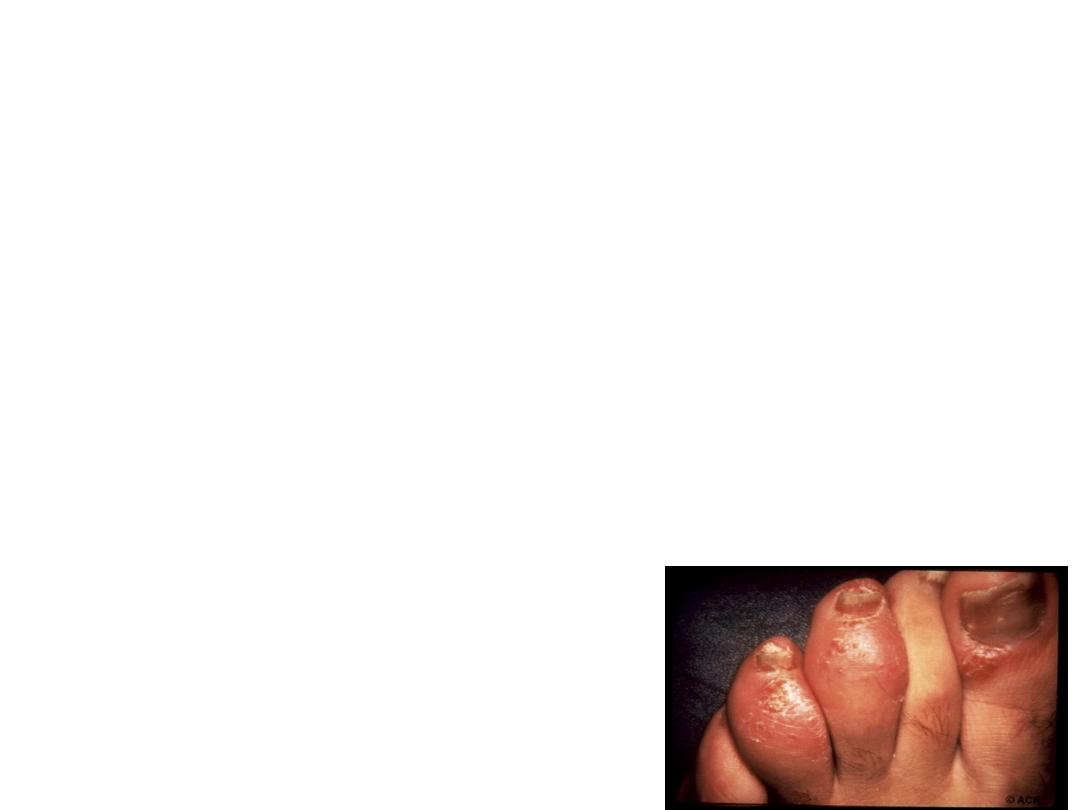
• Circinate balanitis and keratoderma blennorrhagica are
considered a characteristic skin lesion and can give a
clue for diagnosis in atypical cases.
• Nail dystrophy.
• Mouth ulcer shallow ,red, and may occur on buccal
mucosa, tongue, palate and they are painless, transient
“only a few days”.
• Uveitis: Especially up to 30% in recurrent and chronic
type. While rare in first episode. other features are rare
which include:
• -Cardiac: Aortic incompetence, conductive defect,
pleuro-pericarditis.
• Peripheral neuritis, CNS :fits, meningo-encephalitis.

• Investigation:
• the diagnosis usually made on clinical background
• Joint aspiration is needed especially in single to exclude
infectious and crystal arthritis.
• Synovial fluid, inflammatory containing giant
multinucleated macrophage “Reiter’s cells”.
• ESR,CRP are raised in acute attack.
• RF, ACPA and ANF are negative.
• Urethritis could determined by examinant of void
specimen “two glass test”.
• Stool culture, apart from salmonella infection, usually
negative.
• Previous bacillary dysentery could be tested by serum
agglutinin test.
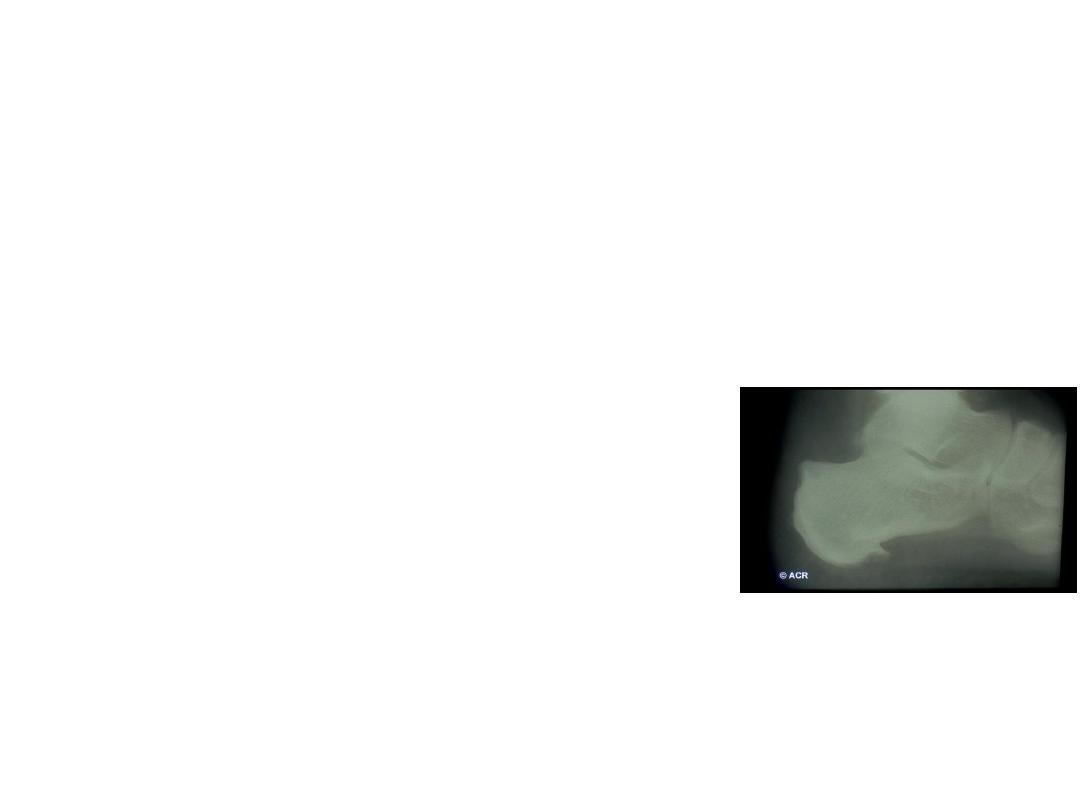
• Radiographic changes:
• No changes in 1
st
acute attack apart of soft tissue
swelling.
• In recurrent or chronic form: Periarticular
osteopenia, j. space narrowing, marginal
proliferative erosion.
• Periostitis of metatarsal, phalanges.
• Fluffy calcaneal spur.
• In contrast to AS :Sacroiliac involvement usually
asymmetrical and may unilateral, and coarse
asymmetrical , non marginal syndesmophyte
•
•

• Management:
• In 1
st
acute attack symptomatic treat. by rest , NSAID and
analgesia.
• Joint aspiration, with intra art. corticost inj. “after
exclusion of septic arthritis”. There is no convincing
evidence for the use of
• antibiotics unless a triggering infection is identified
• If chlamydial urethritis is diagnosed, it should be treated
empirically with a short
• course of doxycycline or a single dose of azithromycin.
• DMARD (methotrexate or salazopyrine) should be
considered in severe progressive, persistent marked
symptoms, recurrent form and these with
keratodermablenn.

• Uveitis must be treated urgently as a medical
emergency requiring local or
• systemic steroid by ophthalmologist. In severe
case recalcitrant to DMARDs and those with
progressive spondylitis , Anti TNF therapy should
be considered .

• Spondylitis, chronic erosive arthritis, recurrent
arthritis and uveitis are major causes of long-
term morbidity.

• Psoriatic Arthritis
• This term describes a variety of different patterns
of arthritis and enthesitis seen in people with
psoriasis or with family history of psoriasis.
• 7-20% may be up to 40%of individuals with
psoriasis develops psoriatic arthritis. It occurs
mainly between age 25-40 years old. Sometimes
the arthritis predate psoriatic lesion. Occasionally
both occur synchronously.

• Clinical Features:
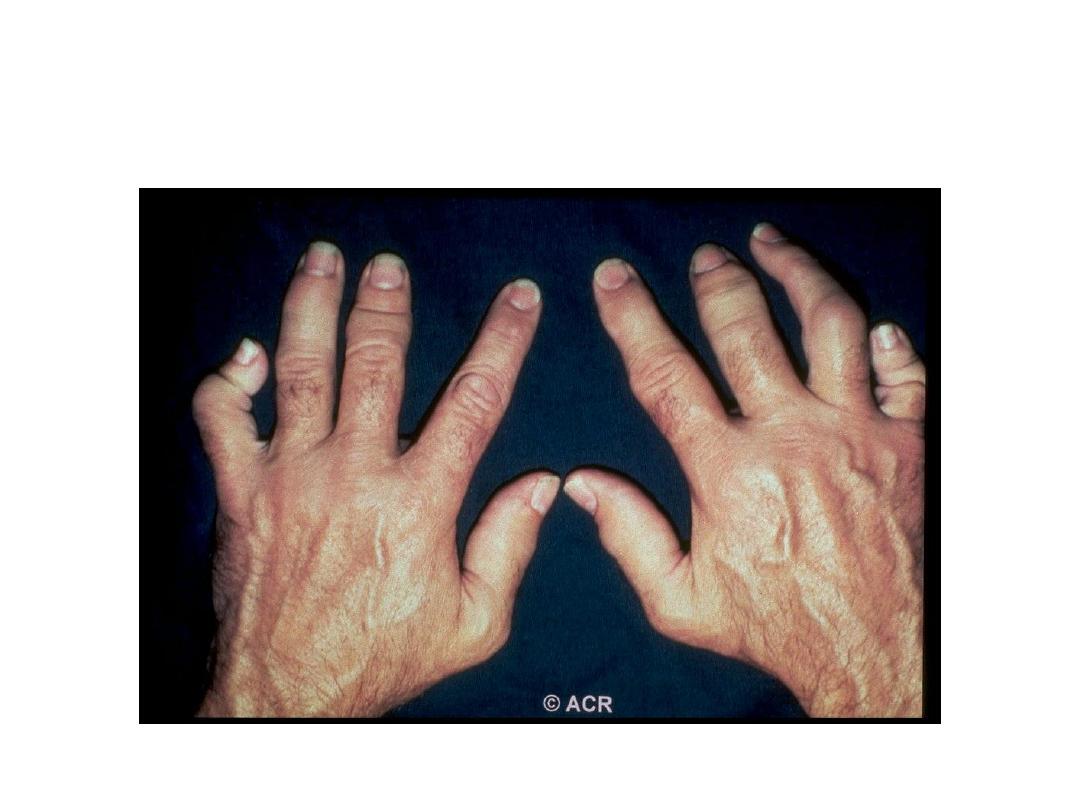
•
Five
main arthritis patterns can be presented as psoriatic
arthritis:
Asymmetrical inflammatory oligoarthritis
: affecting lower
and upper limbs. -
• Association of synovitis with periarticular tenosynovitis,
enthesitis gives a characteristic appearance when affecting
the digit “Sausage digit” or datylitis.
• -
Symmetrical polyarthritis
: especially in women, is similar
to RA but absence of Rh. Nodules and extra-articular
features of RA, persistent absence of RF, characteristic
radiological features and typical DIP joint involvement, and
may associated with spondylitis as well, in addition to
presence of Ps. Skin and/or nail lesion, “all of these points
are important to differentiate psoriatic arthritis from RA”.

• Predominantly DIP joint: Arthritis usually in men,
mainly associated with nail psoriasis.
• Psoriatic Spondylitis, either alone or associated with
peripheral arthritis.
• Arthritis Mutilans: erosive form, affecting mainly
fingers and toes, causes severe bone and cartilage
loss with bone shortening. The overlying skin
invaginated, telescoped (so traction can pull the
• digit back to its original length).
• Enthesitis predominant

• Extra-articular Features:
–
Psoriatic skin lesion.
–
Psoriatic nail lesion.
–
Eye: conjunctivitis, Uveitis mainly in
patient with HLA-B27, especially with
sacroiliitis and spondylitis.
•

• Investigation:
• ESR and CRP may be raised, especially in active
polyarticular.
• autoantibodies are generally absent.
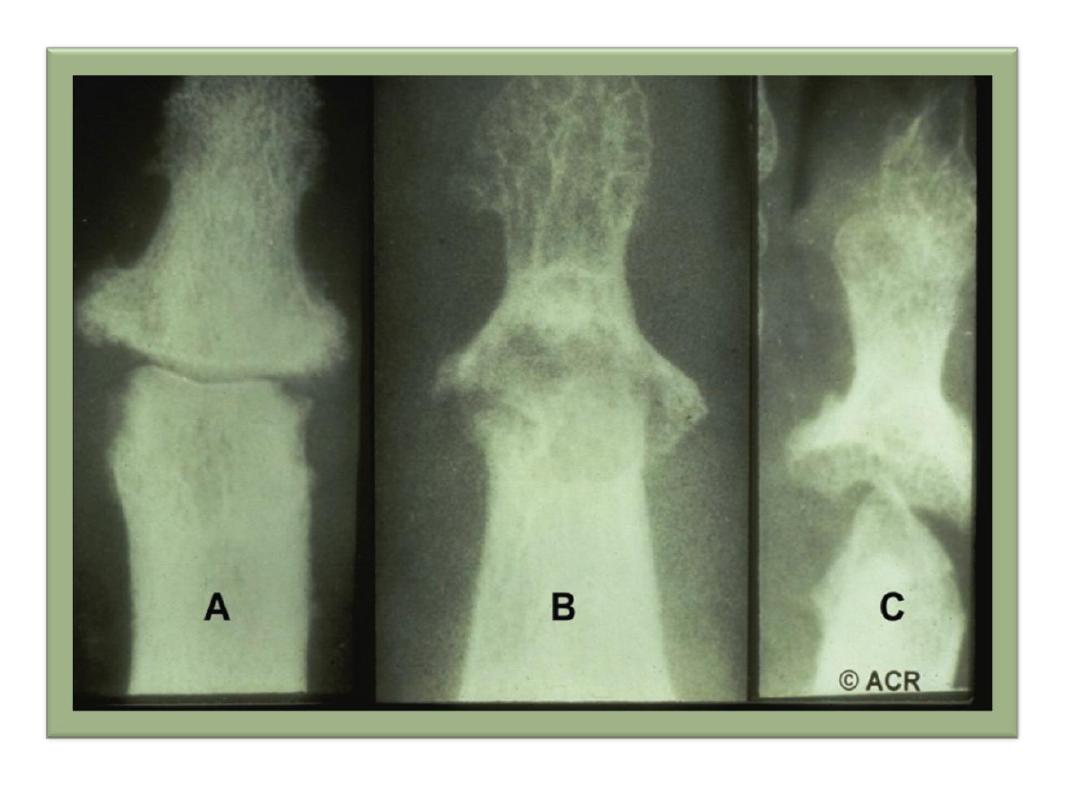
• X-ray findings may be normal, or in persistent synovitis
may show marginal proliferative erosions , sometimes
give an appearance of “pencil in cup”, also the bone
density is maintained and increased in bone sclerosis
giving the appearance of “ivory phalanx”.
• Radiological changes in spondylitis and sacroiliitis are
mostly similar to that of axial involvement of reactive
arthritis . MRI and Doppler ultrasound are
• employed to detect early synovial inflammation and
enthesitis.

• Management:
• -Symptomatic, simple analgesia, NSAIDs.
• - intra-articular injection of corticosteroid in florid synovitis.
• -Regular exercises to maintain joint mobility and avoid prolong rest
and splintage because of tendency to fibrous or bony ankylosis.
• -Similar advices and physiotherapy and exercise, in axial
involvement as in AS.
• -Therapy with DMARDs should be considered for
• persistent synovitis unresponsive to conservative treatment.
• Methotrexate is the drug of first choice because it
• may also help skin psoriasis, but other DMARDs may
• also be effective, including sulfasalazine, ciclosporin and
• leflunomide. Monitoring of DMARD is needed with special
attention to liver function as abnormalieies can associated with
PsA..

•
Anti TNF-α agent are highly effective for severe skin and
joint disease. Other biological treatments, such as
ustekinumab, Is used, which target the IL-12/23 receptor.
•
Ustekinumab is highly effective in the treatment of
psoriatic skin disease and is often effectve in PsA.
•
Anti-malarial should be avoided because it can cause
exfoliative
•
Apremilast is an oral small-molecule inhibitor
•
effective in PsA when
•
DMARD therapy fails, although it appears to be less
efficacious
•
than biologic treatment. Adverse effects include weight
loss,
•
depression and suicidal ideation. reaction.
•

• Arthritis associated with Inflammatory Bowel Disease
(Enteropathic (spondylo)arthritis):
• Two patterns of arthritis are associated with ulcerative
colitis and Crohn’s disease:
• Enteropathic peripheral arthritis: 12% in ulcerative colitis and
20% in Crohn’s disease. Lower large joints are commonly
affected, but the wrist and small joints of toe and finger of
hand can be affected also.
• The arthritis follow the underlying bowel disease activity, so it
usually appears with the exacerbation of bowel disease, also
it cease after colectomy of U.C, Extra-articular features:
aphthous oral lesion, iritis and erythema nodosum.
• Axial(Sacroiliitis 16% and AS 6%) : especially in HLA-B27
patients, can predate or follow bowel disease . Here the
course it is independent of bowel disease activity.
•
