.
,Dr Ali Alkazzaz
Babylon collage of medicine
Lupus history
• Lupus is the Latin word for wolf
• 1
st
used medically in the 10
th
century
• Described clinically in the 19
th
century
• Butterfly rash in 1845
• Arthritis in 1892
• Nephritis in 1895 by Osler
• Serologic tests become available in the 20
th
century
• LE cell in 1948
• Lupus anticoagulant in 1952
• ANA in 1954

LINES
•
Basics
•
Diagnosis
•
Pathogenesis
•
Treatment
• The better we know about clinical out come
of disease and immune abnormalities we
better can fight the disease
•
Systemic Lupus Erythematosus
•
Inflammatory multisystem disease
•
1.5 million cases
•
Women>Men- 9:1 ratio (90% cases are women)
•
African Americans>Whites
•
Onset usually between ages 15 and 45 years, but
can occur in childhood or later in life
•
Highly variable course and prognosis, ranges from
mild to life threatening
•
Characterized by flares and remissions
•
Associated with characteristic autoantibodies

different forms of lupus
1. Systemic Lupus Erythematosus
2. Discoid or Cutaneous Lupus
3. Drug-Induced Lupus
4. Neonatal Lupus

symptoms of lupus
Painful swollen joints a
Unexplained fever
Extreme fatigue
Rashes
Sensitivity to the sun
Mouth Sores
Hair loss
Pale or purple fingers or toes from cold
Swollen glands
Headache and/or Depression
Chest pain with deep breathing
Low blood count
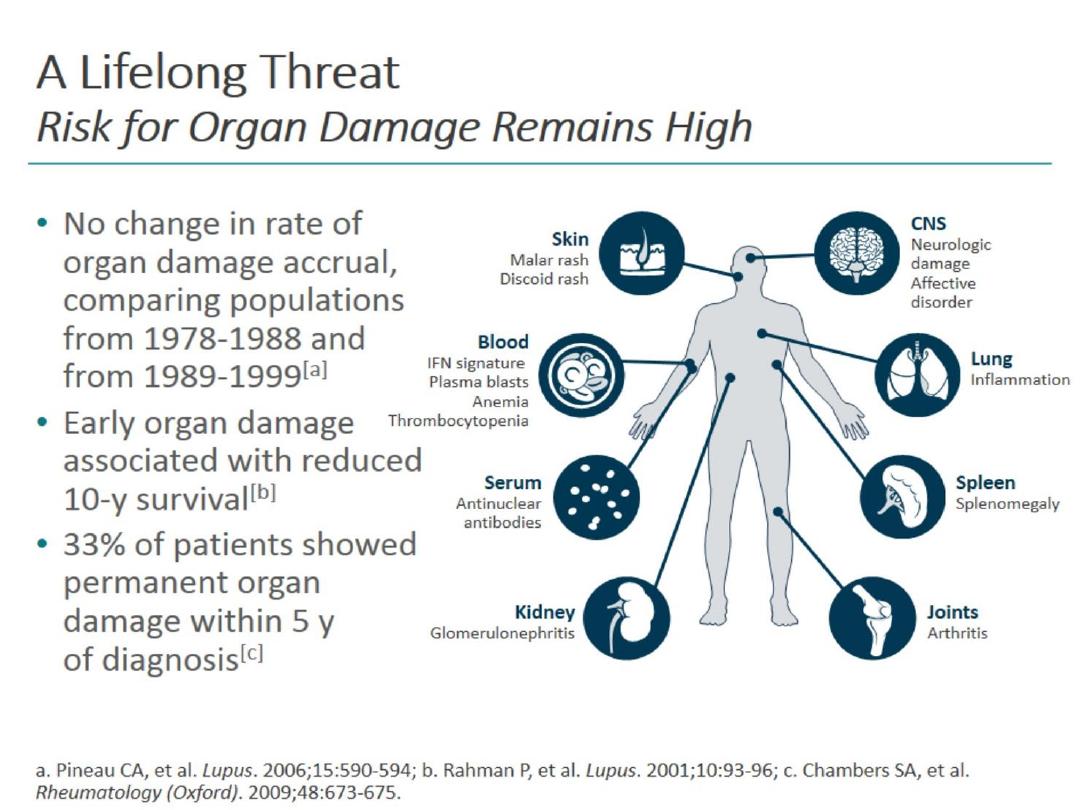

Majors
problems
• Repeated Miscarriages
• Disease in organs
– Kidney
– Heart
– Lungs
– Brain and nerves
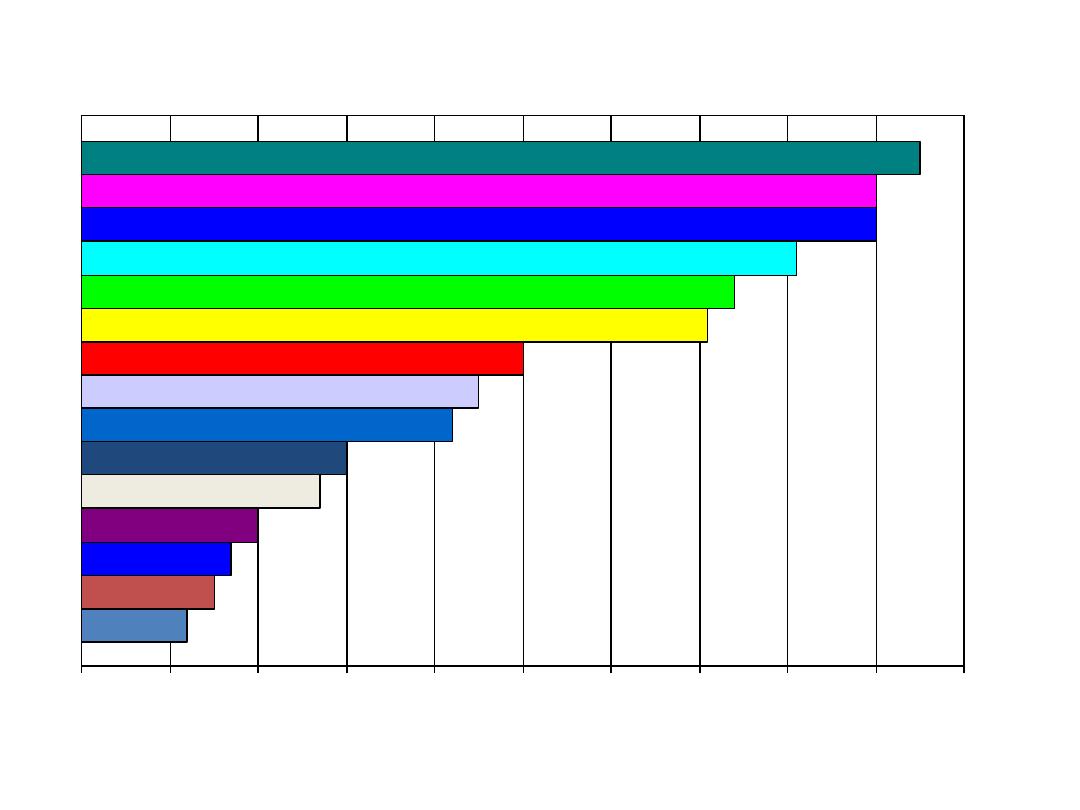
Lupus presenting symptoms
Raynauds
Hair Loss
Photosensitivity
Facial Rash
Pluerisy
Ulcers
Seizures
Clotting
Renal
Anemia
Skin Rashes
Extreme Fatigue
Swollen Joints
Fevers
Painful Joints
0
10
20
30
40
50
60
70
80
90
100
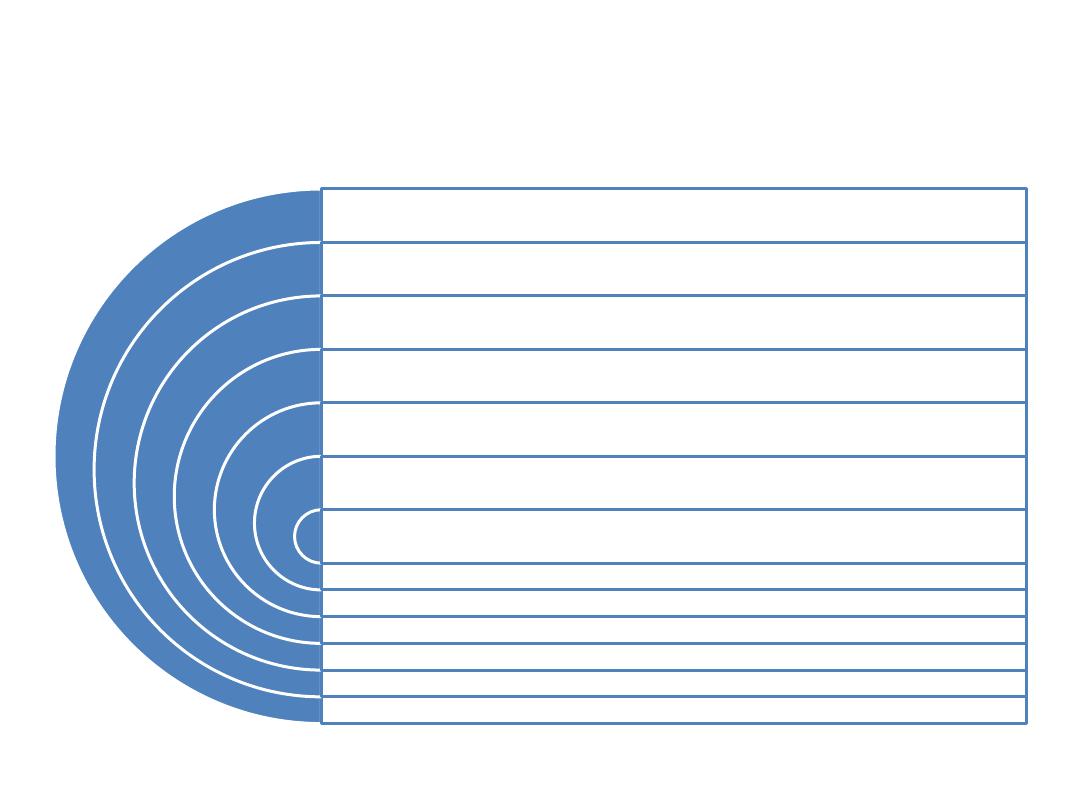
lupus prevalence
More people have
Lupus than
Cerebral Palsy,
Multiple Sclerosis,
Sickle Cell Anemia
and Cystic Fibrosis
combined.

How do we diagnose lupus?
•
Skin criteria
Systemic criteria
•
1. Malar rash
5. Arthritis
•
2. Discoid Rash
6. Serositis
•
3. Photosensitivity
7. Kidney
•
4. Oral Ulcers
8. Neurologic
•
Lab criteria
•
9. Anti-nuclear antibody
•
10. Immunologic
•
11. Hematologic
•
*4 criteria simultaneously or serially for
diagnosis

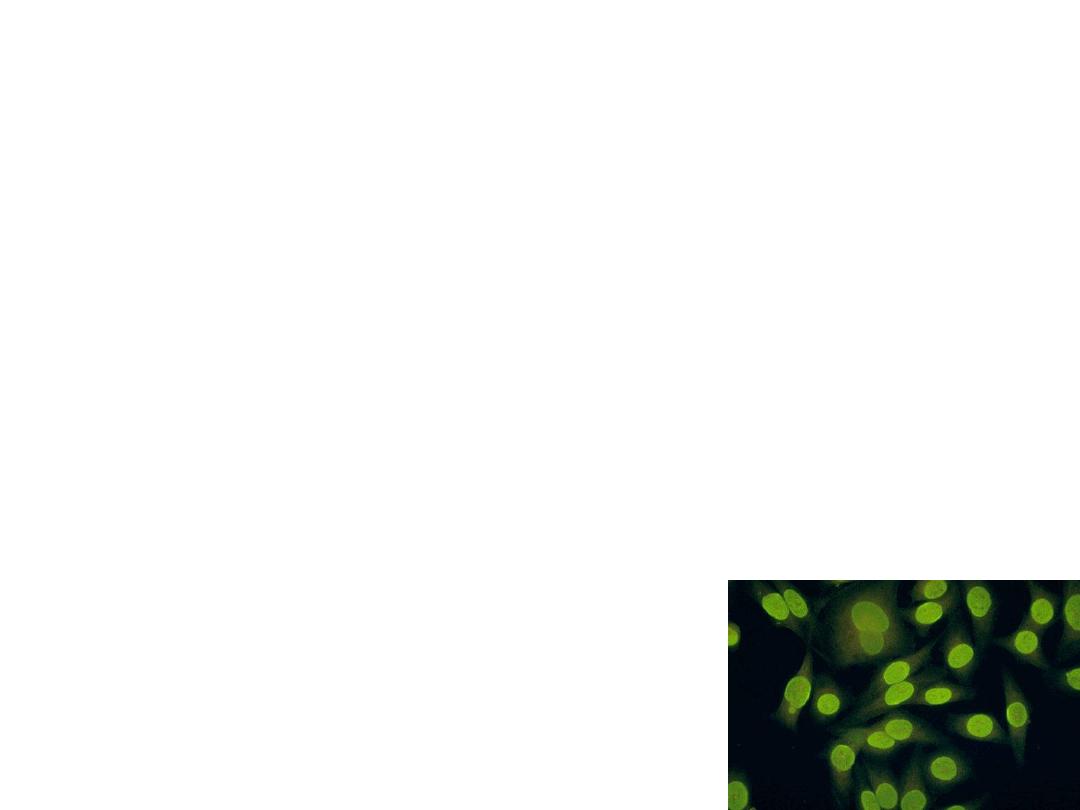
ANA&lupus Dx
•
ANA
•
Seen in 99% of SLE
•
Not specific for SLE
•
Seen in many inflammatory, infectious, and
neoplastic diseases
•
Seen in 5% to 15% of normal persons
Causes of lupus
genetics
hormones
environment

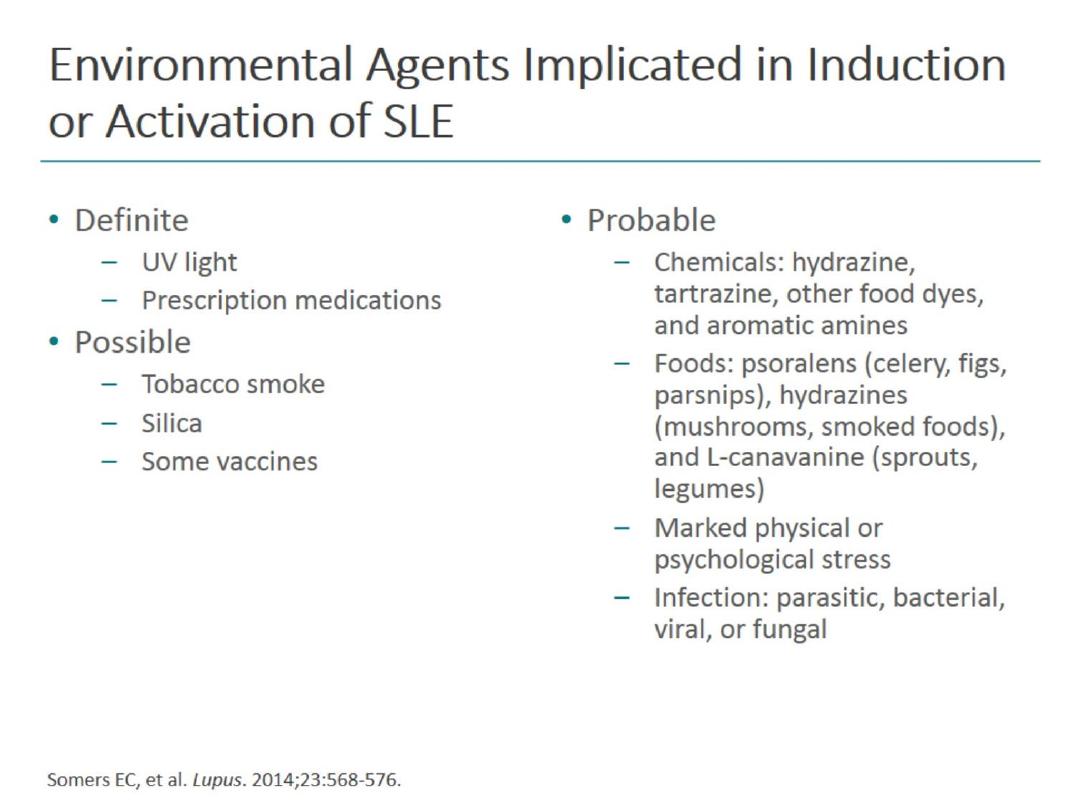
Triggers
Ultraviolet
light
Stress
Medication
s
Infections
Hormonal
Changes

New thoughts on causes and triggers
•
Human Microbiome Project (HMP) an NIH
initiative started in 2008 to identify the
microorganisms which are found in association
with both healthy and diseased humans (the
human microbiome)
•
Can contribute to development of a variety of
autoimmune diseases including multiple sclerosis,
rheumatoid arthritis, and possibly lupus

System Specific Symptoms
• Nervous System
– Headaches, numbness, tingling, seizures, psychosis
• Digestive System
– Nausea, vomiting, dyspepsia
• Cardiovascular System
– Arrhythmias, pericarditis, myocarditis
• Respiratory System
– Pleurisy, pleural effusion, pneumonitis, pulmonary
hypertension
• Integumentary system
– Raynaud’s phenomenon, malar rash
• Excretory system Edema, weight gain, acute renal failure

Genetic Predispositions
• HLA genes most studied
– HLA Class II gene polymorphisms
– HLA DR2 and DR3
• Associated with autoantibodies:
– Anti-Sm, anti-Ro, anti-La, anti-nRNP, anti-dsDNA,
anti-PL
• Other Associated Genes
–
BANK1
,
BLK
, IL-21-R, CD40, Lyn,
PTPN22
, TNFAIP3,
FcγRs,
Blimp-1
• Klinefelter Syndrome
– Contributes to female susceptibility
– Hypogonadotrophic hypogonadism

Immunological Mechanisms
Two Stage Disease
• Loss of self-tolerance/Auto-Abs generation
• Immune complex formation, causes
inflammation/disease
Stage One: Loss of Self-tolerance
• Involves self-antigen presentation by DCs
Role of Apoptosis
• Impaired clearance of apoptotic cells
• Results from defective complement system
• C2, C4, C1q defects
• Reduced CR1 receptors

Results of Immune Complexes
Local inflammation
Local complement
activation
Local apoptosis
Positive feedback loop

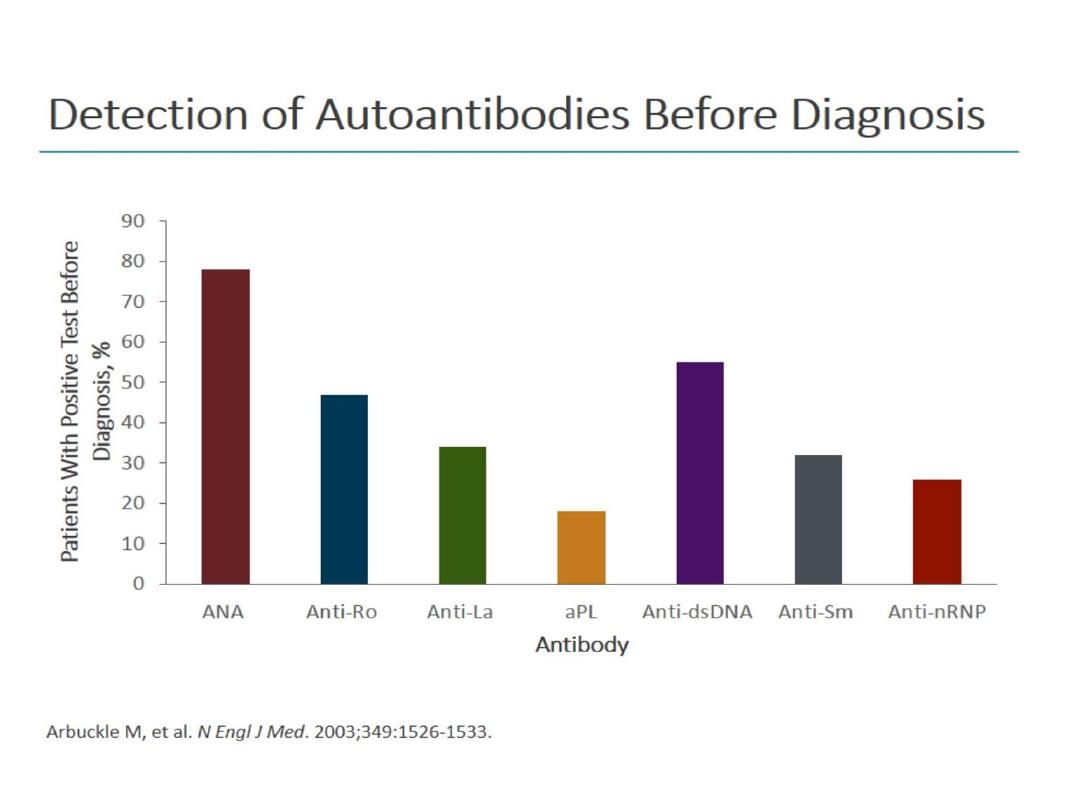
What laboratory tests should use to diagnose lupus?
ANA
Negative ANA inconsistent with diagnosis of SLE
If positive, test for antigen-specific ANAs
Those targeting dsDNA or ribonucleoprotein complexes Ro/SSA,
La/SSB Smith,
RNP (extractable nuclear antigens)
Basic investigations for SLE
Complement C3 and C4
CBC, ESR, CRP, comprehensive
m
etabolic panel
Urinalysis
Direct
Coombs’ test (if hemolytic anemia + reticulocytosis)
Creatine phosphokinase (if muscle weakness)

other diagnoses should consider in
patients with possible lupus?
Chronic fatigue syndrome
Fibromyalgia
Rheumatoid arthritis
Small or medium vessel vasculitides
Thrombotic thrombocytopenic purpura
Viral arthritis
Hematopoietic cancer
Malignant lymphoproliferative syndromes
Goals
0f management

medications are used to treat lupus
1-2 mg \kg Glucocorticoids
First-line agents for most
manifestations
Dosage and duration based on clinical
experience
Antimalarials
Hydroxychloroquine: cornerstone of SLE
treatment
To prevent disease flares
NSAIDs
Immunosuppressive treatment
In lupus nephritis: based on histopathologic
classifications
Other manifestations: treatment often includes
immunosuppressives and a multidisciplinary
approach
stable patient who is not having a flare
• Used to treat inflammatory arthritides for
>50 years
• Prevents relapses
• Reduces risk for congenital heart block in
neonatal SLE
• Antithrombotic effects are important in
antiphospholipid antibody-related
prothrombotic diathesis
• Well-tolerated with rare side effects
(retinopathy; skin hyperpigmentation;
neuromuscular or cardiac toxicity
Hydroxychloroquine
and other
antimalarials

drug therapy for arthritis?
First-line agents
0.5 mg per kg Low-dose glucocorticoids
Antimalarials
Other treatment
Methotrexate (particularly in patients without
other systemic manifestations)

Indications for kidney biopsy in SLE
Increasing serum creatinine
Without compelling alternative causes
Confirmed proteinuria ≥1.0gm per 24h
24-h urine specimens or spot protein/creatinine
ratio
Combination of the following:
Proteinuria ≥0.5 gm per 24h + hematuria (≥5
RBCs/high-power field)
or Proteinuria ≥0.5 gm per 24h + cellular casts

therapy for respiratory manifestations?
Pleuritis
NSAIDs, low- to moderate-dose glucocorticoids
alveolar hemorrhage
IV glucocorticoids + immunosupressants; consider
plasmapheresis
• Pulmonary hypertension
• PDE-5 inhibitors, ERAs, and prostacyclin analogs may be used; with
or without immunosuppressants
In interstitial lung disease: glucocorticoids, and, if poor
response, cyclophosphamide or azathioprine
Acute lupus pneumonitis
High doses of glucocorticoids and cyclophosphamide

Monitoring patients who are being treated for lupus
Routinely test: CBC, basic metabolic panel, urinalysis
• Allows evaluation of target-organ manifestations
• Routinely test?: dsDNA antibodies + C3 & C4 levels
• Controversial for clinically stable patients
• Treatment with prednisone of clinically stable but serologically
active patients may avert severe flare
Monitor individual disease manifestations
• Monitor for immunosuppressant toxicity
• If treated with hydroxychloroquine: ophthalmological evaluation
(particularly if >40y and treated for a long time)
• Monitor for osteoporosis, osteonecrosis
• Consider periodic lipid testing, ECHO

When should patients with lupus be hospitalized?
Severe thrombocytopenia
Severe or rapidly progressive renal disease
Suspected lupus pneumonitis or pulmonary
hemorrhage
Chest pain or severe cardiovascular manifestations
CNS and neurological manifestations
Unexplained fever

CLINICAL BOTTOM LINE: Treatment
Hydroxychloroquine
Prevents disease flares
Cornerstone of SLE treatment
Glucocorticoids
First-line for most SLE manifestations
Dose & duration based on clinical experience, consensus
Immunosuppressive treatment in lupus nephritis
Based on histopathologic classification
Guided by ACR recommendations
Treatment of other lupus manifestations
Based on clinical experience
Often immunosuppressive Rx + multidisciplinary approach
Multiple Choice Questions
What immunological aberration is the principle cause for SLE?
– Overproduction of T-helper cells
– Inhibition of complement activity
– Production of self-reactive antibodies
– Stimulation of perforin and granzyme activity in facial tissue
2) What are the two stages of SLE pathogenesis?
– Loss of immune-tolerance and degradation of secondary
lymphoid organs
– Overabundance of immune-tolerance and generation of
immune complexes causing inflammation
– Overabundance of immune-tolerance and manifestation of
SLE causing bacteria
– Loss of immune-tolerance and generation of immune
complexes causing inflammation

3) What type of immune of cells are least effected by
SLE?
– Neutrophils
– T cells
– B cells
– Dendritic cells
4) What reason listed below accounts for impaired
clearance of immune complexes in SLE?
– Insufficient CTL activity
– Serum viscosity is too high for complexes to fall out of
solution
– Insufficient quantities of macrophages to snarf up
complexes
– Defective complement system
Study Questions Answers
1: C
2: D
3: A
4: D
•
Thanks
•
For
•
Listening
